Abstract
Purpose
To report three cases of Loa loainfestation presenting over the course of 12 months to ophthalmology departments in the South West Thames region around London.
Methods
Case series (three case histories are described) and literature review.
Results
All three patients had a history of travel to West Africa. All had worms surgically removed and were referred to an infectious diseases hospital, where these were confirmed as adult Loa loanematodes and treatment was initiated.
Conclusions
Although ocular loiasis is endemic in West Africa, European ophthalmologists in areas of diverse ethnicity should be aware that it is presenting increasingly frequently, that there is often no history of recent travel abroad, and that loiasis is a differential diagnosis for any ‘at-risk’ patient with an unexplained foreign body sensation.
Similar content being viewed by others
Introduction
Loa loa is one of nine nematode worms that use humans as the definitive host. It is endemic in West Africa, where prevalence in some areas is as high as 50%.1 Transmission occurs when an infected human's blood is ingested by Chrysops flies that host partial microfilarial maturation. Infected flies then inoculate other humans, in whom adult worms mature and roam subcutaneously, occasionally eliciting pruritic (Calabar) swellings. Despite one report of Loa loa transmission in a non-endemic area,2 immigrants from, and travellers to, endemic areas are at greatest risk. Here we describe three cases of loiasis presenting to ophthalmology departments in the South West Thames region over a 12-month period.
Case reports
Case 1
A 35-year-old Ghanaian male, who had migrated to the United Kingdom 8 years ago, attended the Mayday University Hospital (Croydon, UK) in October 2008 complaining of a 1-day history of left eye redness. These episodes had occurred approximately yearly for the preceding 6 years, during which he felt something moving near his eye. On examination, a live subcutaneous worm was seen in the left upper eyelid. This was removed and typed as a male Loa loa worm. Further management was at the Hospital for Tropical Diseases (London, UK).
Case 2
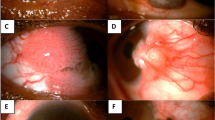
A 21-year-old female medical student presented to St Thomas’ Hospital in October 2009, having felt something move in her left eye periodically for over a year. She had not travelled to any endemic region for loiasis as her schooling in Nigeria had ended 6 years earlier. She reported an itchy (Calabar) swelling at her left elbow 2 months earlier. On examination, a live worm was seen moving in the superior subconjunctival space (Figure 1). This was removed under a topical anaesthetic and typed as a male Loa loa worm (Figure 2). A video demonstrating removal of the nematode has been published online.3 Blood tests revealed a raised eosinophil count, normal inflammatory markers, positive filarial serology, and a high microfilarial load of 125 microfilariae per 5 ml. She was treated with 4 days of oral prednisolone 40 mg OD, followed by oral diethylcarbamazine.
Case 3
A 20-year-old female Cameroonian student, who had migrated to the United Kingdom 6 years earlier, presented to St George's Hospital (London, UK) in January 2009 with a 3-day history of a foreign body sensation, irritation, and redness of the right eye. She described ‘something moving’ in the eye. A live worm was seen subconjunctivally, removed under a local anaesthetic, and typed as a male Loa loa worm. Systemic treatment was initiated at the Hospital for Tropical Diseases (London, UK).
Discussion
Some 20–40 million people carry Loa loa infestations worldwide. In Europe, loiasis has been almost unknown until recent years, with ‘first’ cases reported recently from Norway4 and Italy.5 As our series demonstrates, the worm is increasingly common here, and with rising population mobility, this trend may continue.
Both Loa loa and another nematode, Onchocerca volvulus, have a predilection for ocular tissues. In onchocerciasis, this usually comprises anterior chamber microfilariae; in loiasis, it is adult worms that affect the eye. Loa loa worms usually appear subconjunctivally or (as in Case 1) in the periorbital subcutis, but may rarely present in the anterior chamber.2, 6 The presentation of ocular Loa loa is characteristic, with patients complaining of something moving in or near their eye (100% in our series). The World Health Organisation uses this complaint, and questions regarding Calabar swellings, as part of their screen for endemicity.7 Localisation of a worm subconjunctivally or in the periocular subcutis is highly indicative of Loa loa, but other nematodes have been found in similar locations, including Wuchereria bancrofti,8 Brugia malayi,9 Dracunculus medinensis,10 and Mansonella perstans.11
Importantly, the patient's history need not include recent foreign travel. After inoculation by an infected fly, adult worms take approximately 3–4 years to mature in the human host and have been reported to live for as long as 17 years.12 Consequently, Loa loa may present many years after the patient was last in an endemic region—as late as 8 years in our series.
Blood films taken at noon and midnight are important in the detection and quantification of microfilaraemia. Definitive diagnosis of filarial species is made parasitologically.13 The principal treatment used for loiasis is diethylcarbamazine, starting with 1 mg/kg/day and increasing over 3 days to 6 mg/kg/day. In heavy infestations, rapid microfilaricide may precipitate febrile reactions and encephalopathy, and pre-treatment with corticosteroids may mitigate this. Ivermectin and albendazole are alternative systemic treatments. During ocular worm removal, subconjunctival lidocaine may facilitate removal by paralysing the worm.
In summary, we report three cases of Loa loa presenting to South West Thames ophthalmology departments over a recent 12-month period. The incidence of loiasis may continue to increase, and ophthalmologists are advised to consider this diagnosis in any ‘at-risk’ patient with unexplained foreign body sensation.

References
Kamgno J, Boussinesq M . Hyperendemic loaiasis in the Tikar plain, shrub savanna region of Cameroon. Bull Soc Pathol Exot 2001; 94 (4): 342–346.
Barua P, Barua N, Hazarika NK, Das S . Loa loa in the anterior chamber of the eye: a case report. Indian J Med Microbiol 2005; 23 (1): 59–60.
Shah AN, Saldana M . Images in clinical medicine. Ocular loiasis. N Engl J Med 2010; 363: e16.
Varhaug P . Subconjunctival Loa loa: first case report from Norway. Acta Ophthalmol 2009; 87 (8): 929–930.
Aiello F, Palma S, Varesi C, Cerulli A, Valente R, Aiello L . A rare case report of Loa loa ocular filariasis. Eur J Ophthalmol 2010; 20 (1): 237–239.
Osuntokun O, Olurin O . Filarial worm (Loa loa) in the anterior chamber. Report of two cases. Br J Ophthalmol 1975; 59 (3): 166–167.
Takougang I, Meremikwu M, Wandji S, Yenshu EV, Aripko B, Lamlenn SB et al. Rapid assessment method for prevalence and intensity of Loa loa infection. Bull World Health Organ 2002; 80 (11): 852–858.
Gautret P, Bain O, Gicquel JJ, Hue B, Kauffmann-Lacroix C, Rodier MH et al. Subconjunctival localization of a Wuchereria bancrofti adult female. Bull Soc Pathol Exot 1999; 92 (2): 104–106.
Rohela M, Jamaiah I, Yaw CC . Eye lesion caused by adult Brugia malayi: a first case reported in a child from Malaysia. Southeast Asian J Trop Med Public Health 2006; 37 (4): 652–655.
Burnier Jr M, Hidayat AA, Neafie R . Dracunculiasis of the orbit and eyelid. Light and electron microscopic observations of two cases. Ophthalmology 1991; 98 (6): 919–924.
Baird JK, Neafie RC, Connor DH . Nodules in the conjunctiva, bung-eye, and bulge-eye in Africa caused by Mansonella perstans. Am J Trop Med Hyg 1988; 38 (3): 553–557.
Padgett JJ, Jacobsen KH . Loiasis: African eye worm. Trans R Soc Trop Med Hyg 2008; 102 (10): 983–989.
Walther M, Muller R . Diagnosis of human filariases (except onchocerciasis). Adv Parasitol 2003; 53: 149–193.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Bowler, G., Shah, A., Bye, L. et al. Ocular loiasis in London 2008–2009: a case series. Eye 25, 389–391 (2011). https://doi.org/10.1038/eye.2010.192
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2010.192
Keywords
This article is cited by
-
Ocular loiasis in Ohio: a case report
International Ophthalmology (2018)