Abstract
Objectives
To determine the relationship between the preoperative macular height of a macular detachment and visual outcome of the post retinal reattachment.
Methods
Prospective case series of 26 patients who presented to the Wolverhampton Eye Infirmary with a primary rhegmatogenous macula-off retinal detachment. Macular detachment height was assessed by B-scan ultrasound (10 Mhz) in the seated and supine postures before surgery. Age, gender, duration of the detachment, type of surgery, preoperative (pre-op) and postoperative (post-op) visual acuities at 3 and 6 months and status of the fellow eye were noted.
Results
A total of 26 eyes of 26 patients (mean age: 61.4 years±15.56 SD) were recruited. The mean logMAR pre- and post-op visual acuities at 3 and 6 months were 1.5±1.1 SD (range: 0.2–3), 0.38±0.23 SD (range: 0–0.84), and at 6 months 0.29±0.22 SD (range: 0–1.0). The median period of the macular detachment was 4.5 days (95% CI: 2–8 days). There was no significant difference between the mean macular heights while seated 2.42 mm±1.2 or supine 2.39 mm±1.0 (t-test, P=0.9). Correlation showed that the pre-op macular height is a statistical predictor of post-op visual acuity in our group of patients with macula-off retinal detachments.
Conclusions
The shallower the macular detachment the greater the likelihood of a good visual outcome.
Similar content being viewed by others
Introduction
Several factors affect the visual prognosis of a macula-off retinal detachment. The preoperative (pre-op) visual acuity is the most significant factor (P<0.0005) affecting postoperative (post-op) visual acuity.1, 2 Visual prognosis is better if they are repaired within 7 days, and is significantly poorer if the delay is ⩾6 weeks.1, 2, 3, 4 Macular height estimation by ultrasound (US) has been shown to have a positive correlation for retinal detachments of ⩽7 days duration.5 The aim of our study is to assess the effect of macular height on visual recovery in macula-off retinal detachments at the Wolverhampton Eye Infirmary.
Patients and methods
This was a prospective study on patients with primary rhegmatogenous macula-off retinal detachments who attended the Wolverhampton Eye Infirmary between June 2002 and June 2004.
The research protocol was approved by the Institutional Review Board/Ethics Committee at New Cross Hospital, and the study was carried out in accordance with the tenets of Helsinki Declaration. All patients gave written voluntary informed consent. The inclusion criteria included all patients with primary macula-off rhegmatogenous retinal detachments that were able to give voluntary consent. All patients had to be able to clearly identify when they lost central vision (corresponding to the time when the macula detached). Exclusion criteria included all patients that had previous retinal surgery in the affected eye, patients with glaucoma, optic neuropathy, age-related macular degeneration, or amblyopia.
All patients underwent a full ophthalmic examination with slit-lamp biomicroscopy and indirect ophthalmoscopy with indentation. They then underwent ultrasonography by a single doctor (ST).
Ultrasonic measurements were carried out with the CineScan (Quantel Medical Inc., Bozeman, MT, USA) 10 MHz probe. The patient was examined initially in a sitting position. A single point on the retinal pigment epithelium, 4 mm temporal from the centre of the optic nerve, was identified. Digital calipers were used to measure the perpendicular distance between the RPE and the outer neurosensory detached retina. This was repeated in a supine position.
Data were collected on age, gender, affected eye, duration of macular detachment, type of surgical repair, pre- and post-op visual acuities at 3 and 6 months, and status of other eye. The method of repair included scleral buckling or pars plana vitrectomy, cryotherapy/endolaser, and gas or oil (in two cases). The best-corrected visual acuity was documented pre-op, and at 3 and 6 months post-op. All patients were followed for 6 months. All snellen acuities were converted into logMAR equivalent for statistical analysis. *Count finger and hand movements were converted to logMAR equivalent of 1.8 and 36 (*count finger at 3 feet=1/60, logMAR 1.8; hand movements at 3 feet=20/20000,logMAR 3).6
Statistical analysis was carried out by MINITAB 14.0, simple and multivariate linear regression and correlation were determined. The patients were analysed as a total group and then as a subgroup of those with macula-off retinal detachment of ⩽7 and >7 days duration.
Results
A total of 26 eyes of 26 patients with a mean age 61.4 years±15.6 SD were enrolled in the study. There were 11 female (26–77 years, mean 59.7±18.8 SD) and 15 male patients (40–84 years, mean 62.7±13.2 SD). In all, 73% (19/26) of cases were on right eyes; 57% were repaired by vitrectomies and 43% were repaired by scleral buckling procedures.
Duration of macula-off retinal detachment
The duration of the macular detachment was 1– 90 days (median: 4.5 days, 95% CI: 2–8 days; Figure 1). This was skewed by one patient whose duration was 90 days. A total of 69.2% (18/26) of patients had macula-off detachment of ⩽7 days duration at the time of surgery (mean: 3.1 days, 95% CI: 2–4.2 days). All patients had macular reattachment at the 6 month visit.
Visual outcome (total group)
The mean pre-op logMAR visual acuity was 1.5±1.1 SD (range: 0.2–3). The mean post-op logMAR visual acuity at 3 months was 0.38±0.23 SD (range: 0–0.84) and at 6 months it was 0.29±0.22 SD (range: 0–1.0). The 3 and 6 month post-op visual acuity pearson's correlation was very strong (0.78; P=0.005). All patients in the study had improved visual acuity at the 3 and 6 month visit except one patient who had 0.8 logMAR at 3 months and decreased to 1.0 at 6 months because of an epiretinal membrane. However, two patients had vitrectomy with cryo and silicone oil. The silicone oil was removed before the 3-month visit. Three patients were noted to have a cataract in the operated eye postoperatively (their post opvisual acuities were 0.44, 0.46 and 0.76 logMAR). No patient underwent cataract surgery during the study period.
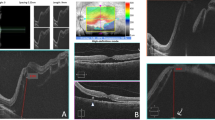
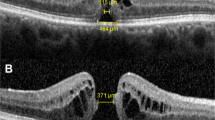
Height of macular detachment (total group)
The heights of the detachment were 0.92–5.10 and 0.82–4.75 mm in sitting and supine positions, respectively (Figure 2). The mean macular height for the total group was higher in the sitting group (2.42 mm±1.2) than that in the supine group (2.39 mm±1.0; Table 1). There was no significant difference between the macular height in sitting or supine position (t-test, P=0.9). Two patients had pre-op macular height measurements over 5 mm, one of whom had a wide variation between the two postures. She was a 77-year-old woman whose macular heights were 5.1 and 1.85 mm in sitting and supine positions, respectively. Her detachment was 28 days old, with a pre-op visual acuity of 1.0 logMAR, which improved to 0.3 and 0.2 logMAR at 3 and 6 months, respectively. The other patient was a 59-year-old woman with a macula-off detachment of 2 days duration. Her pre-op macular height was elevated at 5.05 mm in sitting and 4.65 mm in supine positions, and had a pre-op visual acuity of 1.8 logMAR, which was improved to 0.48 and 0.44 at 3 and 6 months, respectively. The correlation between the sitting and supine height was 0.73 (P<0.0005).
Macular height vs post-op visual acuity (total group)
There was a weak correlation of the pre-op visual acuity with the macular detachment height (sitting and supine; Table 2); however, this was not statistically significant. There was a positive correlation between the post-op 3-month visual acuity and the macular height (Figure 3). The correlations were 0.38 (P=0.05) and 0.4 (P=0.04) for the macular height in the seated and supine position, respectively, with the visual acuity at 3 months. The correlation of macular height and improvement of visual acuity was significant when the height was measured in the supine position.
Analysis of the patients with macula-off detachment of ⩽7 days duration
In all, 69.2% of the total patients recruited were with the macula-off detachment of ⩽7 days duration. Mean age of the patients was 59.3±14.7 years; 33.3% (6/18) were women; 72.2% (13/18) were on right eyes; 50% (9/18) had lattice in the fellow eye that required treatment by laser or cryotherapy. The mean macular heights were 2.21±1.2 (sitting) and 2.26±1.0 mm (supine; Table 2). There was no statistically significant difference between the macular heights of the total group (P=0.8) and the subgroup of patients with macular detachments of ⩽7 days duration.
The pre-op visual acuity was 0.2–3.0 logMAR with a mean pre-op visual acuity of 1.6±1.2 logMAR. The post-op visual acuity was 0–0.54 logMAR , with a mean post-op visual acuity of 0.33±0.24 and 0.24±0.17 logMAR at 3 and 6 months post-op, respectively.
There was a weak correlation between the pre-op visual acuity and the macular height (Table 2).
Analysis of patients with macula-off retinal detachment of >7 days duration
There were eight patients who had retinal detachment of >7 days duration. In all, 50% were women and the mean age was 66.1±6.2 years. The duration of detachment varied from 11 to 90 days. The patient whose macular detachment was 90 days duration was a 34-year-old woman whose pre-op visual acuity was 1.0 logMAR ; her post-op visions were 0.3 and 0.22 at 3 and 6 months, respectively. A total of 50% of patients had post-op visual acuity of 0.42 logMAR or better. The mean duration was 28.5±25.6 days. The mean pre-op macular heights were 2.9±1.2 and 2.7±0.8 mm in sitting and supine positions, respectively (Table 1).
The mean pre-op logMAR was 1.2±0.8. The mean post-op logMARs were 0.5±0.2 and 0.41±0.2 at 3 and 6 months, respectively. There was no statistically significant correlation between macular height and the post-op visual acuity in this subgroup (Table 2).
Discussion
The height of a macular detachment depends on the volume and mobility of subretinal fluid, which varies depending on the size and location of the retinal break, presence of retinal traction, status of vitreal liquefaction, and posture. Our study shows that the lower the macular height the better the visual outcome for the total group of macula-off detachments. The macular height in supine position had a higher correlation to the post-op visual acuity for the total group. However, when we looked at subgroups, it was not statistically significant. This may be because of the fact that the sample size of the subgroups was not large enough to pick up a statistical difference.
Ross and Kozy1 had shown that the final visual outcome is not affected by the duration of the macular detachments for macula-off retinal detachments of ⩽7 days duration, but by the height of the macular detachment.5 There are no other published studies using B Scan ultrasound (US) to assess the macular height with correlation to visual outcome. A review of the literature establishes that pre-op visual acuity, duration of macular detachment, absence of proliferative retinopathy, age of patient, and now, macular height can assist the clinician in determining the visual prognosis.1, 2, 5, 7 However, microstructural changes in the retina, including damaged photoreceptor outer segments, residual subretinal oedema, and cystoid macular oedema (not clinically seen with ophthalmoscopy or fundus fluorescein angiography), may have an adverse effect on the final vision.6, 8, 9, 10, 11
We concur with Ross and Kozy1 that the assessment of pre-op macular height with B-scan US as a predictive factor of final visual outcome for our total group of macula-off retinal detachments. The B-scan US is the standard equipment in most ophthalmic departments and can be used to assess the macular height of the macula-off detachments. Further studies with larger numbers would be required to quantitate the possible visual outcome according to the macular height.
References
Ross WH, Kozy DW . Visual recovery in macula off rhegmatogenous retinal detachments. Ophthalmology 1998; 105: 2149–2153.
Mowatt L, Shun-shin GA, Arora S, Price N . Macula off retinal detachments. How long can they wait before it is too late. Eur J Ophthalmol 2005; 15 (1): 109–117.
Abouzeid H, Wolfensberger TJ . Macular recovery after retinal detachment. Acta Ophthalmol Scand 2006; 84 (5): 597–605.
Hassan TS, Sarrafizadeh R, Ruby AJ, Garretson BR, Kuczynski B, Williams GA . The effect of duration of macular detachment on results after the scleral buckle repair of primary, macula off retinal detachments. Ophthalmology 2002; 109 (1): 146–152.
Ross W, Lavina A, Russell M, Maberley D . The correlation between height of macular detachment and visual outcome in macula off retinal detachments of < or =7 days' duration. Ophthalmology 2005; 11 (7): 1213–1217.
Friberg TR, Eller AW . Prediction of visual recovery after scleral buckling of macula off retinal detachment. AM J Ophthal 1992; 114: 715–722.
Tani P, Robertson DM, Langworthy A . Prognosis for central vision and anatomic reattachment in rhegmatogenous retinal detachment with macula detached. Am J Ophthalmol 1981; 92 (5): 611–620.
Wolfensberger TJ, Gonvers M . Optical coherence tomography in the evaluation of incomplete visual acuity recovery after macula-off retinal detachments. Graefes Arch Clin Exp Ophthalmol 2002; 240 (2): 85–89.
Schocket LS, Witkin AJ, Fujimoto JG, Ko TH, Schuman JS, Rogers AH et al. Ultrahigh-resolution optical coherence tomography in patients with decreased visual acuity after retinal detachment repair. Ophthalmology 2006; 113 (4): 666–672.
Lecleire-Collet A, Muraine M, Menard JF . Brasseur evaluation of macular changes before and after successful retinal detachment surgery using stratus optical coherence tomography. Am J Ophthalmology 2006; 142 (1): 176–179.
Lecleire-Collet A, Muraine M, Menard JF, Brasseur G . Predictive visual outcome after macula-off retinal detachment surgery using optical coherence tomography. Retina 2005; 25 (1): 44–53.
Acknowledgements
We thank Dr Anthony Frankson and Mr Michael Yee-Shui (University of the West Indies) for statistical advice and Ms Annegret Dahlmann.
Author information
Authors and Affiliations
Corresponding author
Additional information
Proprietary interests: none
Rights and permissions
About this article
Cite this article
Mowatt, L., Tarin, S., Nair, R. et al. Correlation of visual recovery with macular height in macula-off retinal detachments. Eye 24, 323–327 (2010). https://doi.org/10.1038/eye.2009.74
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.74
Keywords
This article is cited by
-
Functional and perfusion changes associated with silicone oil tamponade after macula-off rhegmatogenous retinal detachment surgery: an optical coherence tomography angiography/microperimetry study
International Ophthalmology (2024)
-
Factors affecting visual recovery after successful repair of macula-off retinal detachments: findings from a large prospective UK cohort study
Eye (2021)
-
Correlation between preoperative factors and final visual acuity after successful rhegmatogenous retinal reattachment
Scientific Reports (2019)
-
Correlation of visual recovery with macular height in macular-off retinal detachment
Eye (2010)
-
Reply to Young-Hoon Park
Eye (2010)