Abstract
Choroidal neovascularisation (CNV) is characterised by new blood vessel growth under the retina that usually results in significant visual impairment when the fovea is involved. Though CNV is more commonly associated with age-related macular degeneration (AMD), it can occur secondary to a variety of other diseases. Recent successes with anti-angiogenic therapies suggest that they may outperform other therapies for all types of CNV. As non-AMD-related CNV cases are rare, randomised controlled trials are often not possible. This review compares the less prevalent reports of non-AMD CNV and pools evidence on the success and limitations of a variety of therapies.
Similar content being viewed by others
Background
Choroidal neovascularisation (CNV) can cause visual loss because of exudation of intraretinal or subretinal fluid, haemorrhage, or fibrosis at the macula.1 Age-related macular degeneration (AMD) and pathologic myopia are the most common causes of CNV. Less common causes include angioid streaks, inflammatory conditions such as punctate inner choroidopathy, multifocal choroiditis, ocular histoplasmosis syndrome, and hereditary retinal diseases.2 A diagnosis of idiopathic CNV (INCV) is made when no apparent cause of CNV can be determined. Non-AMD-related CNV has a younger age of onset than AMD CNV and typically presents as a smaller type 2 lesions, with CNV growing above the RPE and with a ‘classic’ appearance on angiography.3
Vascular endothelial growth factor (VEGF) is an important pro-angiogenic factor that is normally produced by RPE and retinal photoreceptors. In CNV, the RPE initiates and supports abnormal neovascularisation.3, 4 A recent development in the treatment of CNV is the use of pharmacologic agents that block VEGF. Several recent reports have shown that intravitreal injection of anti-VEGF agents such as pegaptanib sodium (Macugen), ranibizumab (Lucentis), and bevacizumab (Avastin) are effective in the treatment of both AMD and non-AMD CNV. Pegaptanib (Macugen, Eyetech Pharmaceuticals, New York, New York, USA) is an aptamer that targets VEGF 165,5 and ranibizumab (Lucentis, Novartis Pharmaceuticals Corporation, East Hanover, New Jersey, USA) is an antibody fragment that targets all VEGF isoforms.6, 7 Bevacizumab (Avastin, Genentech, South San Francisco, California, USA) is an anti-VEGF drug originally developed to treat metastatic carcinoma of the colon and rectum and is a recombinant humanised monoclonal antibody against all VEGF isoforms.8, 9 Although this drug is ‘unlicensed’ for intraocular use, it has been widely used as intravitreal therapy for all types of CNV. In fact, reports about bevacizumab treatment of CNV far outnumber those about other anti-VEGF agents for CNV treatment.
As non-AMD-related CNV cases are rare, it is not often possible to rely on randomised controlled trials for evidence on how best to manage these cases. The objective of this review is to compile and analyse the current evidence on the use of intravitreal bevacizumab to treat CNV in non-AMD patients.
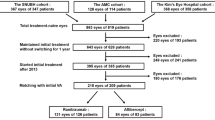
Methodology
We conducted a systematic search of MEDLINE for publications between January 2004 and May 2009. The National Institutes of Health clinical trial databases were also searched for ongoing trials in these areas up to May 2009. For the database searches, we used the following terms or term combinations: CNV, anti-VEGF, bevacizumab, avastin, AMD, age-related maculopathy, retinal degeneration, retinal inflammation, uveitis, choroiditis, retinal dystrophy, myopia, angioid streaks, punctate inner choroidopathy, choroidal rupture, trauma, and idiopathic. Our search strategy combined keywords and medical subject heading terms. We included all data that could be extracted from the abstracts of articles in languages other than English. Visual acuity values were converted to log minimum angle of resolution (logMAR) units where appropriate. We included all reports on subfoveal non-AMD CNV that had described treatment with bevacizumab, with a minimum of 3 months follow-up. There were two main criteria for excluding reports; we excluded reports that did not provide visual or anatomical outcomes, those that involved extrafoveal CNV, or those that involved systemic bevacizumab.
We extracted two main outcome measures from all collected reports. The first is the mean change in best-corrected visual acuity at designated time points. The second is the mean number of treatments required for each condition at specified time points. In addition, we noted all reported complication rates in all reports. We also compared the visual outcomes achieved with bevacizuamb treatment to other published treatments for each condition.
Pathological myopia
High myopia affects approximately 2% of the global population. Ethnic origin seems to influence the likelihood of developing pathologic myopia, as prevalence is high in Asian populations, and low in African and Pacific island groups.10 Myopic maculopathy is the main cause of vision loss among highly myopic patients and is the leading aetiology of subfoveal CNV among patients younger than 50 years. Nearly 10% of eyes with degenerative retinal findings consistent with high myopia develop CNV.11 The precise pathogenesis of myopic CNV remains unclear. However, some authors have suggested that mechanical tissue strain caused by stretching may lead to the development of choroidal ischaemia, followed by atrophy of both the RPE and the overlying retina, and the subsequent release of growth factors.12
The visual prognosis of untreated myopic CNV is generally poor because of the associated progressive retinal atrophy. The natural history data on myopic CNV indicate that visual outcomes may be variable for up to 3 years. For most patients, obvious decline is noted after this variable period, and approximately 95% of patients decline to a visual acuity of ⩾20/200 by 10 years.13
Therapeutic options
There are several treatments for myopic CNV, but they show limited efficacy. These include thermal laser photocoagulation,14 photodynamic therapy (PDT),15 macular translocation,16 and surgical removal of CNV tissue.17 The frequency of CNV complications undermines these treatments and generally bears poor long-term results.
Photodynamic therapy Evidence for the use of PDT for subfoveal myopic CNV is based on a Verteporfin PDT study (VIP).18, 19 In this prospective, multicentre, randomised controlled trial, a statistically significant positive visual outcome was noted at 12 months. Specifically, 72% of PDT-treated eyes lose fewer than eight letters, whereas only 44% of placebo-treated eyes show this outcome. However, this effect was not sustained at 2 years, likely because of expansion of macular atrophy caused by the treatment. The mean number of treatments required in the first year was 3.4, and 5.1 treatments were performed over the 2-year period.18, 19 A combination of intravitreal triamcinolone and PDT have also been attempted to reduce treatment rates and improve visual outcomes.20 However, these data are limited.
Anti-VEGF agents There are more reports about intravitreal bevacizumab treatment than treatment with the other two anti-VEGF agents, ranibizumab and pegatanib sodium. There are two published reports on ranibizumab and one for pegaptanib sodium treatment.21, 22, 23 Treatment outcomes after intravitreal bevacizumab in 15 studies are summarised in Table 1 .24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38
A cumulative analysis of all study data reveals the following trends. Of all studies examined, a total of 181 eyes received treatment for naïve lesions, and 74 eyes were treated earlier. Of the earlier treatments, 72 included PDT and 2 included sub-tenon's triamcinolone. The dosing schedule varied between studies. A majority of eyes (n=174) were treated with one injection, followed by additional injections pro re nata (prn). A total of 81 eyes were treated with an initial cycle of monthly injections for 3 months, followed by an optical coherence tomography (OCT)-guided re-treatment.
Pooled study data analysis We pooled and analysed common variables among the bevacizumab studies. Overall, the dose of bevacizumab varied from 1 to 2.5 mg. The mean number of injections was 1.65 (range: 1.1–2.20) at 6 months and 2.49 (range: 1.4–3.6) at 12 months. Eyes that received a cycle of monthly injections for first 3 months required an average of one cycle. At 6 months, the change in visual acuity for naïve patients (baseline 0.81 logMAR to 0.48 logMAR) was better than earlier treated patients (0.68 logMAR to 0.40 logMAR). However, at 12 months, there was no significant difference in visual acuity between these patient groups (Table 2 ).
Different end points were used in most studies. However, on average, 64–68% eyes gained 15 or more letters at the end of 6 months and this gain was maintained in 40–44% eyes at the end of 12 months in studies that reported 12 months outcomes.
Eyes that received a cycle of monthly injections for first 3 months had better visual outcomes at 6 months than eyes that had prn treatment (three injection monthly=0.66 logMAR to 0.33 logMAR vs prn treated=0.91 logMAR to 0.66 logMAR); however, there was no significant difference at 12 months. There were few reported complications; there was only one case each of retinal detachment,28 RPE rip,24 and low grade iridocyclitis.30
These pooled 12-month data suggest that visual outcomes with bevacizumab treatment are better than other available options for myopic CNV. Cumulative data indicates that a mean of 1.56 injections is sufficient to stop the activity of myopic CNV. Under these circumstances, treatment with bevacizumab on a prn basis seems more logical than a cycle of three injections. Nonetheless, the recurrence of CNV is often difficult to assess in myopic CNV because of associated atrophic changes and the small size of the lesion. However, the long-term effects of bevacizumab on RPE atrophy remain unknown.
Currently, there are three ongoing clinical trials for the treatment of myopic CNV with bevacizumab, either alone or in combination with other therapeutics (clinicaltrials.gov). The results of these studies are pending.
Angioid streaks
Angioid streaks are linear breaks in the Bruch's membrane. These streaks may be an ocular manifestation of systemic conditions, such as pseudoxanthoma elasticum, Paget's disease, or sickle cell haemoglobinopathies. The most common complication of angioid streaks is the development of CNV and consequent impairment of vision. This phenomenon occurs in 72–86% of patients, and more than half of these patients present with bilateral CNV.39 Angioid streaks usually affect young people and may have a profound effect on their working life. The natural history of CNV associated with angioid streaks is an irreversible deterioration of central vision. In most cases, this leads to legal blindness because of macular scarring and the development of a large central scotoma.
Therapeutic options
Therapeutic interventions such as laser photocoagulation, PDT, and surgery have shown variable success at preserving vision. New anti-angiogenic agents have opened up some alternatives for treatment of CNV secondary to angioid streaks.
Photodynamic therapy There are conflicting results for the treatment of angioid-streak-related CNV with PDT with verteporfin. In the short term, visual stabilisation and improved visual acuity of 1.37 lines have been reported at 8 months after PDT.40, 41 Browning et al40 presented a minimal decrease of mean visual acuity from baseline in 16 eyes from 20/100 to 20/125 after a follow-up of 12 months in a study group of subfoveal CNV, whereas four out of seven eyes in the juxtafoveal CNV group progressed to a subfoveal location during the follow-up of 12 months. Other studies with longer follow-up also report enlarged CNV or disciform lesions in most patients with poor visual acuity of 20/600.42, 43 A study with longer mean follow-up of 26.1 months on 15 eyes (10 with subfoveal, 5 with extra- or juxtafoveolar CNV) showed that the mean visual acuity decreased from 20/32 to <20/200 in nearly half the patients and only 13% was noted to have ⩾20/63 at final follow-up.44
Anti-angiogenic agents Owing to the rarity of this condition, single case reports are the prevalent source of treatment outcome data. Intravitreal bevacizumab (1.25 mg/0.05 ml) was used in all reports except for one, wherein pegaptanib sodium (0.3 mg/0.09 ml) was administered.45 All reports indicate an improvement of vision in the short term (Table 3 ).46, 47, 48, 49, 50, 51, 52, 53, 54 The longest follow-up is approximately 2 years (range: 3–24 months).
There are several interesting trends among studies of angioid-streak-related CNV treatment with anti-angiogenic agents. Gains in vision and the mean number of injections were not significantly different between patients with naïve lesions and those with earlier treated eyes. There was also no difference in outcome after a cycle of three monthly injections when compared with prn administration. The mean number of injections administered in the treatment of angioid-streak-related CNV was higher than those for myopic CNV and lower than those for AMD CNV. Most studies reported decreased or absent leakage at the end of the follow-up. No injection-associated complications were reported.
The current evidence indicates that anti-angiogenic agents are the only treatment that might help patients with angioid-streak-related CNV. However, long-term studies are necessary to understand the full potential and adverse events of these treatments, particularly for co-morbidities such as pseudoxanthoma elasticum.
Angioid-streak-related CNV is aggressive and has a high rate of recurrence. These patients must be strongly encouraged to self-monitor their vision with Amsler charts and immediately report any visual distortion, even after initiation of anti-VEGF therapy. The area of CNV may be small, and OCT evidence of subretinal fluid may be the first sign of disease when a patient presents with a recurrence, even before angiographic evidence is obvious. Thus, for the first time, there is a useful therapy for this cohort of patients who harbour an aggressive disease that is often bilateral and blinding.
Inflammatory eye disease
CNV is a well-documented complication of posterior uveitis and white dot syndrome, with and without inflammation. Within this group of inflammatory diseases, CNV is a major sight-threatening complication, and patients with subfoveal CNV have the most guarded prognosis.55, 56
Therapeutic options
Subfoveal CNV in various inflammatory chorioretinal disorders often responds to systemic,57 periocular, or intraocular corticosteroid therapy. When this approach fails, additional therapies have included laser photocoagulation,58, 59, 60 PDT,61, 62 and submacular surgery,63 with limited success.
Anti-inflammatory and immunosuppressive agents Corticosteroids have been used in the treatment of inflammatory CNV. Mechanisms of intravitreal corticosteroids include reduction of retinal capillary permeability by increasing the activity and/or density of tight junctions in the retinal capillary endothelium,64 inhibition of the VEGF gene expression, inhibition of the VEGF metabolic pathway,65 and suppression of intracellular adhesion molecule-1 (ICAM-1)-mediated leucocyte adhesion to vessel walls.66 Corticosteroids help keep vision stable, but increase the incidence of cataracts and glaucoma.
Photodynamic therapy Several studies have reported a beneficial effect of PDT in subfoveal and juxtafoveal inflammatory CNV. Stabilised or improved vision occurred in 70–92.3% of cases reported in retrospective studies.67, 68 One study reported on 13 multifocal choroiditis with panuveitis and subfoveal CNV patients who received PDT and reported stabilisation of vision over a 12-month follow-up.62 A prospective study after a combination of intravitreal triamcinolone and PDT therapy reported stabilised or improved vision in 92.9% of patients at the end of 1 year.69
Anti-VEGF agents Seven studies have reported on the use of anti-VEGF therapy for CNV that is secondary to inflammation (Table 4 ).70, 71, 72, 73, 74, 75, 76 Data pooled from these studies are derived from the treatment of 110 eyes. Although the inflammatory disease process varies between diseases, a sub-analysis reveals that the visual outcomes for the treatment of naïve eyes (mean gain of 0.28 logMAR) is better than for earlier treated eyes (0.25 logMAR). In most studies, inflammatory CNV responded favourably after a single dose of bevacizumab, especially in the treatment of naïve eyes. With few exceptions,71, 73 most studies have used prn regimens for treating CNV. Both prn and monthly injection for first 3 months schedules have shown favourable outcomes. No injection-related complications have been reported. Intravitreal injection of bevacizumab seems to be effective for treating extrafoveal, juxtafoveal, and subfoveal CNV, with no additional risk of exaggerated inflammatory response to the drug. Although the limited number of patients with CNV secondary to intraocular inflammation makes it difficult to carry out a prospective, randomised study of the effectiveness of anti-VEGF therapy, our literature analysis suggests that primary treatment with bevacizumab is useful to preserve vision in these patients.
Idiopathic CNV
For many young patients with CNV, there is no apparent cause. These cases are diagnosed as ICNV.77 The natural history of idiopathic subfoveal CNV is not necessarily associated with a profound loss of vision. Lesions of one disc area or smaller at the time of initial fluorescein angiography are more likely to be associated with a final visual acuity of 20/60 or better and less likely to be associated with a final visual acuity of 20/200 or worse.77
Therapeutic options
Several studies have shown PDT to be effective in ICNV.78 In up to 94% of cases, PDT stabilises vision at the end of 1 year.78 Similar results are reported at the end of 2 years in small case studies.79 Visual outcomes after other treatments, such as TTT, submacular surgery, or macular translocation, have not been satisfactory.80
We pooled data from three studies that successfully treated a total of 52 ICNV eyes with bevacizumab30, 71, 73. Overall, visual acuity changed from an initial mean value of 0.8 logMAR to 0.33 logMAR at the end of a mean 5.1 months follow-up. One study71 used three monthly injections in nine eyes, and the other two used a prn regimen.30, 73 Most cases respond favourably within 1 month and required a mean of 1.55 injections per eye (range: 1.4–1.7). Though the average follow-up was short, no injection-related, long-term complications were reported. One eye developed anterior uveitis, which was successfully treated with topical steroids (Table 5).
Other causes of CNV
Numerous other case reports have described the successful use of bevacizumab for the treatment of non-AMD CNV. These include studies with a short follow-up for CNV secondary to Best disease,81 vitelliform degeneration,82 choroidal oesteoma,83 and pseudotumour cerebri.84
Discussion
Owing to the low incidence of non-AMD-related CNV, randomised controlled trials are difficult to conduct. Owing to the rarity of the CNV conditions described, we did not limit our study to only those that met the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement writing standards.85 Consequently, this review examined all possible published reports, and included case series on small numbers of patients, with variable follow-up periods. Our aim was to report trends and that would be relevant to the treatment of patients with these rare diseases.
The cumulative evidence provides good indication of successful ‘off-label’ use of bevacizumab for the improvement of visual outcomes in non-AMD CNV patients. These conditions require very few injections and respond well to OCT-guided prn-treatment schedules. On the basis of PRONTO86 study for AMD, several investigators have tried a cycle of three injections for these conditions. However, the outcomes of single injections followed by prn were similar to those given a loading dose of three injections.
Similarly, although the follow-up periods of these studies are short, there are no significant differences in the rates of complications for this therapy in non-AMD CNV, compared with AMD CNV. We recommend centralised reporting of the effects of treatment and side effects of these rare conditions to ensure improved understanding of the best-treatment strategy.
Conclusions
Definitive conclusions are not possible when examining retrospective studies with small sample sizes, variable follow-up, and a lack of a standard phenotypic and anatomical CNV classification. Regardless, consistently favourable outcomes have been reported with intravitreal bevacizumab treatment of non-AMD-related CNV.
Conflict of interest
The authors declare no conflict of interest.
References
Green WR, Wilson DJ . Choroidal neovascularization. Ophthalmology 1986; 93: 1169–1176.
Cohen SY, Laroche A, Leguen Y, Soubrane G, Coacas GJ . Etiology of choroidal neovascularization in young patients. Ophthalmology 1996; 103: 1241–1244.
Kvanta A, Algvere PV, Berglin L, Seregard S . Subfoveal fibrovascular membranes in age-related macular degeneration express vascular endothelial growth factor. Invest Ophthalmol Vis Sci 1996; 37: 1929–1934.
Lopez PF, Sippy BD, Lambert HM, Thach AB, Hinton DR . Transdifferentiated retinal pigment epithelial cells are immunoreactive for vascular endothelial growth factor in surgically excised age-related macular degeneration-related choroidal neovascular membranes. Invest Ophthalmol Vis Sci 1996; 37: 855–868.
Doggrell SA . Pegaptanib: the first antiangiogenic agent approved for neovascular macular degeneration. Expert Opin Pharmacother 2005; 6: 1421–1423.
Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med 2006; 355: 1419–1431.
Brown DM, Michels M, Kaiser PK, Heier JS, Sy JP, Ianchulev T et al. Ranibizumab vs verteporfin photodynamic therapy for neovascular age-related macular degeneration: two-year results of the ANCHOR study. Ophthalmology 2009; 116: 57–65.
Avery RL, Pieramici DJ, Rabena MD, Castellarin AA, Nasir MA, Giust MJ . Intravitreal bevacizumab (Avastin) for neovascular age-related macular degeneration. Ophthalmology 2006; 113: 363–372.
Spaide RF, Laud K, Fine HF, Klancnik Jr JM, Meyerle CB, Yannuzzi LA et al. Intravitreal bevacizumab treatment of choroidal neovascularization secondary to age-related macular degeneration. Retina 2006; 26: 383–390.
McCarty CA, Livingston PM, Taylor HR . Prevalence of myopia in adults: implications for refractive surgeons. J Refract Surg 1997; 13: 229–234.
Ohno-Matsui K, Yoshida T, Futagami S, Yasuzumi K, Shimada N, Kojima A et al. Patchy atrophy and lacquer cracks predispose to the development of choroidal neovascularisation in pathological myopia. Br J Ophthalmol 2003; 87: 570–573.
Grossniklaus HE, Green WR . Pathologic findings in pathologic myopia. Retina 1992; 12: 127–133.
Hampton GR, Kohen D, Bird AC . Visual prognosis of disciform degeneration in myopia. Ophthalmology 1983; 90: 923–926.
Secretan M, Kuhn D, Soubrane G, Coscas G . Long-term visual outcome of choroidal neovascularization in pathologic myopia: natural history and laser treatment. Eur J Ophthalmol 1997; 7: 307–316.
Ohno-Matsui K, Moriyama M, Hayashi K, Mochizuki M . Choroidal vein and artery occlusion following photodynamic therapy in eyes with pathologic myopia. Graefes Arch Clin Exp Ophthalmol 2006; 244: 1363–1366.
Glacet-Bernard A, Simon P, Hamelin N, Coscas G, Soubrane G . Translocation of the macula for management of subfoveal choroidal neovascularization: comparison of results in age-related macular degeneration and degenerative myopia. Am J Ophthalmol 2001; 131: 78–89.
Ruiz-Moreno JM, de la Vega C . Surgical removal of subfoveal choroidal neovascularisation in highly myopic patients. Br J Ophthalmol 2001; 85: 1041–1043.
Verteporfin in Photodynamic Therapy Study Group. Photodynamic therapy of subfoveal choroidal neovascularization in pathologic myopia with verteporfin. 1-year results of a randomized clinical trial--VIP report no. 1. Ophthalmology 2001; 108: 841–852.
Verteporfin In Photodynamic Therapy Study Group. Verteporfin therapy of subfoveal choroidal neovascularization in age-related macular degeneration: two-year results of a randomized clinical trial including lesions with occult with no classic choroidal neovascularization--verteporfin in photodynamic therapy report 2. Am J Ophthalmol 2001; 131: 541–560.
Chan WM, Lai TY, Wong AL, Liu DT, Lam DS . Combined photodynamic therapy and intravitreal triamcinolone injection for the treatment of choroidal neovascularisation secondary to pathological myopia: a pilot study. Br J Ophthalmol 2007; 91: 174–179.
Mones JM, Amselem L, Serrano A, Garcia M, Hijano M . Intravitreal ranibizumab for choroidal neovascularization secondary to pathologic myopia: 12-month results. Eye 2009; 23: 1275–1280.
Bennett MD, Yee W . Pegaptanib for myopic choroidal neovascularization in a young patient. Graefes Arch Clin Exp Ophthalmol 2007; 245: 903–905.
Konstantinidis L, Mantel I, Pournaras JA, Zografos L, Ambresin A . Intravitreal ranibizumab (Lucentis) for the treatment of myopic choroidal neovascularization. Graefes Arch Clin Exp Ophthalmol 2009; 247: 311–318.
Arias L, Planas N, Prades S, Caminal JM, Rubio M, Pujol O et al. Intravitreal bevacizumab (Avastin) for choroidal neovascularisation secondary to pathological myopia: 6-month results. Br J Ophthalmol 2008; 92: 1035–1039.
Chan WM, Lai TY, Liu DT, Lam DS . Intravitreal bevacizumab (Avastin) for myopic choroidal neovascularization: six-month results of a prospective pilot study. Ophthalmology 2007; 114: 2190–2196.
Gharbiya M, Allievi F, Mazzeo L, Gabrieli CB . Intravitreal bevacizumab treatment for choroidal neovascularization in pathologic myopia: 12-month results. Am J Ophthalmol 2009; 147: 84–93.
Hernandez-Rojas ML, Quiroz-Mercado H, ma-Weiszhausz J, Fromow-Guerra J, Amaya-Espinosa A, Solís-Vivanco A . Short-term effects of intravitreal bevacizumab for subfoveal choroidal neovascularization in pathologic myopia. Retina 2007; 27: 707–712.
Ikuno Y, Sayanagi K, Soga K, Sawa M, Tsujikawa M, Gomi F et al. Intravitreal bevacizumab for choroidal neovascularization attributable to pathological myopia: one-year results. Am J Ophthalmol 2009; 147: 94–100.
Laud K, Spaide RF, Freund KB, Slakter J, Klancnik Jr JM . Treatment of choroidal neovascularization in pathologic myopia with intravitreal bevacizumab. Retina 2006; 26: 960–963.
Mandal S, Garg S, Venkatesh P, Mithal C, Vohra R, Mehrotra A . Intravitreal bevacizumab for subfoveal idiopathic choroidal neovascularization. Arch Ophthalmol 2007; 125: 1487–1492.
Rensch F, Spandau UH, Schlichtenbrede F, von Baltz S, Libondi T, Jonas JB et al. Intravitreal bevacizumab for myopic choroidal neovascularization. Ophthalmic Surg Lasers Imaging 2008; 39: 182–185.
Rheaume MA, Sebag M . Intravitreal bevacizumab for the treatment of choroidal neovascularization associated with pathological myopia. Can J Ophthalmol 2008; 43: 576–580.
Ruiz-Moreno JM, Gomez-Ulla F, Montero JA, Ares S, Lopez-Lopez F, Rodriguez M et al. Intravitreous bevacizumab to treat subfoveal choroidal neovascularization in highly myopic eyes: short-term results. Eye 2007; 23: 334–338.
Sakaguchi H, Ikuno Y, Gomi F, Kamei M, Sawa M, Tsujikawa M . Intravitreal injection of bevacizumab for choroidal neovascularisation associated with pathological myopia. Br J Ophthalmol 2007; 91: 161–165.
Silva RM, Ruiz-Moreno JM, Nascimento J, Carneiro A, Rosa P, Barbosaa A et al. Short-term efficacy and safety of intravitreal ranibizumab for myopic choroidal neovascularization. Retina 2008; 28: 1117–1123.
Tewari A, Dhalla MS, Apte RS . Intravitreal bevacizumab for treatment of choroidal neovascularization in pathologic myopia. Retina 2006; 26: 1093–1094.
Wu PC, Chen YJ . Intravitreal injection of bevacizumab for myopic choroidal neovascularization: 1-year follow-up. Eye 2009; 1476–5454. (Electronic).
Yamamoto I, Rogers AH, Reichel E, Yates PA, Duker JS . Intravitreal bevacizumab (Avastin) as treatment for subfoveal choroidal neovascularisation secondary to pathological myopia. Br J Ophthalmol 2007; 91: 157–160.
Lim JI, Bressler NM, Marsh MJ, Bressler SB . Laser treatment of choroidal neovascularization in patients with angioid streaks. Am J Ophthalmol 1993; 116: 414–423.
Browning AC, Chung AK, Ghanchi F, Harding SP, Musadiq M, Talks SJ et al. Verteporfin photodynamic therapy of choroidal neovascularization in angioid streaks: one-year results of a prospective case series. Ophthalmology 2005; 112: 1227–1231.
Menchini U, Virgili G, Introini U, Bandello F, Ambesi-Impiombato M, Pece A et al. Outcome of choroidal neovascularization in angioid streaks after photodynamic therapy. Retina 2004; 24: 763–771.
Arias L, Pujol O, Rubio M, Caminal J . Long-term results of photodynamic therapy for the treatment of choroidal neovascularization secondary to angioid streaks. Graefes Arch Clin Exp Ophthalmol 2006; 244: 753–757.
Shaikh S, Ruby AJ, Williams GA . Photodynamic therapy using verteporfin for choroidal neovascularization in angioid streaks. Am J Ophthalmol 2003; 135: 1–6.
Heimann H, Gelisken F, Wachtlin J, Wehner A, Völker M, Foerster MH et al. Photodynamic therapy with verteporfin for choroidal neovascularization associated with angioid streaks. Graefes Arch Clin Exp Ophthalmol 2005; 243: 1115–1123.
Molina GI, Calvo-Gonzalez C, Reche-Frutos J, Donate-López J, García-Feijoó J, Leila M et al. Intravitreal pegabtanib sodium in choroidal neovascularization secondary to angioid streaks. Acta Ophthalmol 2008 (E-pub ahead of print 17 October 2008).
Apte RS . Intravitreal bevacizumab for treatment of choroidal neovascularization secondary to angioid streaks. Eye 2008; 22: 734–735.
Bhatnagar P, Freund KB, Spaide RF, Klancnik Jr JM, Cooney MJ, Ho I et al. Intravitreal bevacizumab for the management of choroidal neovascularization in pseudoxanthoma elasticum. Retina 2007; 27: 897–902.
Derriman L, Marshall J, Moorman C, Downes SM . The use of intravitreal bevacizumab to treat choroidal neovascular membranes (CNVMs). Retina 2008; 28: 910–911.
Finger RP, Charbel IP, Ladewig M, Holz FG, Scholl HP . Intravitreal bevacizumab for choroidal neovascularisation associated with pseudoxanthoma elasticum. Br J Ophthalmol 2008; 92: 483–487.
Japiassu RM, Japiassu MA, Pecego MG . Intravitreal bevacizumab in choroidal neovascularization secondary to Gronblad-Strandberg syndrome: case report. Arq Bras Oftalmol 2008; 71: 427–429.
Neri P, Salvolini S, Mariotti C, Mercanti L, Celani S, Giovannini A . Long-term control of choroidal neovascularization secondary to angioid streaks treated with intravitreal Bevacizumab (Avastin(R)). Br J Ophthalmol 2008; 93: 155–158.
Rinaldi M, Dell’omo R, Romano MR, Chiosi F, Cipollone U, Costagliola C . Intravitreal bevacizumab for choroidal neovascularization secondary to angioid streaks. Arch Ophthalmol 2007; 125: 1422–1423.
Teixeira A, Moraes N, Farah ME, Bonomo PP . Choroidal neovascularization treated with intravitreal injection of bevacizumab (Avastin) in angioid streaks. Acta Ophthalmol Scand 2006; 84: 835–836.
Wiegand TW, Rogers AH, McCabe F, Reichel E, Duker JS . Intravitreal bevacizumab (Avastin) treatment of choroidal neovascularization in patients with angioid streaks. Br J Ophthalmol 2008; 93: 47–51.
Brown Jr J, Folk JC, Reddy CV, Kimura AE . Visual prognosis of multifocal choroiditis, punctate inner choroidopathy, and the diffuse subretinal fibrosis syndrome. Ophthalmology 1996; 103: 1100–1105.
Olk RJ, Burgess DB, McCormick PA . Subfoveal and juxtafoveal subretinal neovascularization in the presumed ocular histoplasmosis syndrome. Visual prognosis. Ophthalmology 1984; 91: 1592–1602.
Flaxel CJ . The use of systemic steroids and photodynamic treatment for choroidal neovascularisation in young patients. Br J Ophthalmol 2007; 91: 564–565.
Macular Photocoagulation Study Group. Krypton laser photocoagulation for neovascular lesions of ocular histoplasmosis. Results of a randomized clinical trial. Arch Ophthalmol 1987; 105: 1499–1507.
Macular Photocoagulation Study Group. Persistent and recurrent neovascularization after krypton laser photocoagulation for neovascular lesions of ocular histoplasmosis. Arch Ophthalmol 1989; 107: 344–352.
Macular Photocoagulation Study Group. Five-year follow-up of fellow eyes of individuals with ocular histoplasmosis and unilateral extrafoveal or juxtafoveal choroidal neovascularization. Arch Ophthalmol 1996; 114: 677–688.
Leslie T, Lois N, Christopoulou D, Olson JA, Forrester JV . Photodynamic therapy for inflammatory choroidal neovascularisation unresponsive to immunosuppression. Br J Ophthalmol 2005; 89: 147–150.
Parodi MB, Di CL, Lanzetta P, Polito A, Bandello F, Ravalico G . Photodynamic therapy with verteporfin for subfoveal choroidal neovascularization associated with multifocal choroiditis. Am J Ophthalmol 2004; 138: 263–269.
Hawkins BS, Bressler NM, Bressler SB, Davidorf FH, Hoskins JC, Marsh MJ et al. Surgical removal vs observation for subfoveal choroidal neovascularization, either associated with the ocular histoplasmosis syndrome or idiopathic: I. Ophthalmic findings from a randomized clinical trial: submacular Surgery Trials (SST) Group H Trial: SST Report No. 9. Arch Ophthalmol 2004; 122: 1597–1611.
Antonetti DA, Wolpert EB, DeMaio L, Harhaj NS, Scaduto Jr RC . Hydrocortisone decreases retinal endothelial cell water and solute flux coincident with increased content and decreased phosphorylation of occludin. J Neurochem 2002; 80: 667–677.
Nauck M, Karakiulakis G, Perruchoud AP, Papakonstantinou E, Roth M . Corticosteroids inhibit the expression of the vascular endothelial growth factor gene in human vascular smooth muscle cells. Eur J Pharmacol 1998; 341: 309–315.
Tamura H, Miyamoto K, Kiryu J, Miyahara S, Katsuta H, Hirose F et al. Intravitreal injection of corticosteroid attenuates leukostasis and vascular leakage in experimental diabetic retina. Invest Ophthalmol Vis Sci 2005; 46: 1440–1444.
Hogan A, Behan U, Kilmartin DJ . Outcomes after combination photodynamic therapy and immunosuppression for inflammatory subfoveal choroidal neovascularisation. Br J Ophthalmol 2005; 89: 1109–1111.
Rogers AH, Duker JS, Nichols N, Baker BJ . Photodynamic therapy of idiopathic and inflammatory choroidal neovascularization in young adults. Ophthalmology 2003; 110: 1315–1320.
Chan WM, Lai TY, Lau TT, Lee VY, Liu DT, Lam DS . Combined photodynamic therapy and intravitreal triamcinolone for choroidal neovascularization secondary to punctate inner choroidopathy or of idiopathic origin: one-year results of a prospective series. Retina 2008; 28: 71–80.
Adan A, Mateo C, Navarro R, Bitrian E, Casaroli-Marano RP . Intravitreal bevacizumab (avastin) injection as primary treatment of inflammatory choroidal neovascularization. Retina 2007; 27: 1180–1186.
Chan WM, Lai TY, Liu DT, Lam DS . Intravitreal bevacizumab (avastin) for choroidal neovascularization secondary to central serous chorioretinopathy, secondary to punctate inner choroidopathy, or of idiopathic origin. Am J Ophthalmol 2007; 143: 977–983.
Guthoff R, Goebel W . Intravitreal bevacizumab for choroidal neovascularization in toxoplasmosis. Acta Ophthalmol 2008 (E-pub ahead of print 8 July 2008).
Mansour AM, Mackensen F, Arevalo JF, Ziemssen F, Mahendradas P, Mehio-Sibai A et al. Intravitreal bevacizumab in inflammatory ocular neovascularization. Am J Ophthalmol 2008; 146: 410–416.
Schadlu R, Blinder KJ, Shah GK, Holekamp NM, Thomas MA, Grand MG et al. Intravitreal bevacizumab for choroidal neovascularization in ocular histoplasmosis. Am J Ophthalmol 2008; 145: 875–878.
Tran TH, Fardeau C, Terrada C, Ducos De Lahitte G, Bodaghi B, Lehoang P et al. Intravitreal bevacizumab for refractory choroidal neovascularization (CNV) secondary to uveitis. Graefes Arch Clin Exp Ophthalmol 2008; 246: 1685–1692.
Rosen E, Rubowitz A, Ferencz JR . Exposure to verteporfin and bevacizumab therapy for choroidal neovascularization secondary to punctate inner choroidopathy during pregnancy. Eye 2008.
Ho AC, Yannuzzi LA, Pisicano K, DeRosa J . The natural history of idiopathic subfoveal choroidal neovascularization. Ophthalmology 1995; 102: 782–789.
Chan WM, Lam DS, Wong TH, Lai TY, Kwok AK, Tam BS et al. Photodynamic therapy with verteporfin for subfoveal idiopathic choroidal neovascularization: one-year results from a prospective case series. Ophthalmology 2003; 110: 2395–2402.
Fujisato K, Otani A, Sasahara M, Yodoi Y, Aikawa H, Tamura H et al. Two-year results of photodynamic therapy for choroidal neovascularization in young patients. Nippon Ganka Gakkai Zasshi 2008; 112: 777–785.
Kumar A, Prakash G, Singh RP . Transpupillary thermotherapy for idiopathic subfoveal choroidal neovascularization. Acta Ophthalmol Scand 2004; 82: 205–208.
Leu J, Schrage NF, Degenring RF . Choroidal neovascularisation secondary to Best's disease in a 13-year-old boy treated by intravitreal bevacizumab. Graefes Arch Clin Exp Ophthalmol 2007; 245: 1723–1725.
Montero JA, Ruiz-Moreno JM, De LV . Intravitreal bevacizumab for adult-onset vitelliform dystrophy: a case report. Eur J Ophthalmol 2007; 17: 983–986.
Ahmadieh H, Vafi N . Dramatic response of choroidal neovascularization associated with choroidal osteoma to the intravitreal injection of bevacizumab (Avastin). Graefes Arch Clin Exp Ophthalmol 2007; 245: 1731–1733.
Jamerson SC, Arunagiri G, Ellis BD, Leys MJ . Intravitreal bevacizumab for the treatment of choroidal neovascularization secondary to pseudotumor cerebri. Int Ophthalmol 2008.
Fung AE, Palanki R, Bakri SJ, Depperschmidt E, Gibson A . Applying the CONSORT and STROBE statements to evaluate the reporting quality of neovascular age-related macular degeneration studies. Ophthalmology 2009; 116: 286–296.
Fung AE, Lalwani GA, Rosenfeld PJ, Dubovy SR, Michels S, Feuer WJ et al. An optical coherence tomography-guided, variable dosing regimen with intravitreal ranibizumab (Lucentis) for neovascular age-related macular degeneration. Am J Ophthalmol 2007; 143: 566–583.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gupta, B., Elagouz, M. & Sivaprasad, S. Intravitreal bevacizumab for choroidal neovascularisation secondary to causes other than age-related macular degeneration. Eye 24, 203–213 (2010). https://doi.org/10.1038/eye.2009.201
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.201
Keywords
This article is cited by
-
Intravitreal anti-VEGF treatment for choroidal neovascularization secondary to traumatic choroidal rupture
BMC Ophthalmology (2019)
-
Long-term variable outcome of myopic choroidal neovascularization treated with ranibizumab
Japanese Journal of Ophthalmology (2015)
-
Successful long-term management of choroidal neovascularization secondary to angioid streaks in a patient with pseudoxanthoma elasticum: a case report
Journal of Medical Case Reports (2014)
-
Intravitreal ranibizumab for the treatment of choroidal neovascularisation secondary to angioid streaks
Eye (2012)