Abstract
Purpose
The first aim (I.) was to measure the change of macular thickness in diabetic (DM group) and nondiabetic patients (NORMAL group), the values of operated eye (OP) were compared I.A.) to the fellow, non-operated eye (CONTROL) and I.B.) to preoperative baseline value of the operated eye (PRE). The second aim (II.) was to compare postoperative macular thickening of DM group to NORMAL group eyes.
Methods
Retinal thickness values of the foveal and perifoveal (fovea+3.0 mm, fovea+6.0 mm) sectors and the minimum values were measured in a prospective study using optical coherence tomography (OCT) in 18 eyes of 18 diabetic patients and 53 eyes of 53 nondiabetic patients who underwent uneventful cataract surgery. Data were collected on the preoperative day and on postoperative 1, 7, 30, and 60 days. Student's t-test was used for statistical analysis.
Results
No significant change of the thickness values could be measured one day after surgery. However, a significant increase could be detected on the postoperative 7, 30, and 60 days in the perifoveal 3.0 mm and 6.0 mm sectors either calculated alone or averaged together with the foveal values. The initial (preoperative) average value of 232.7±3.5 μm (mean±SEM, n=144) in the 6.0 mm perifoveal region increased to 246.0±8.2 μm (mean±SEM, n=120, P=0.032) one week, to 249.9±5.1 μm (n=112, P=0.017) one month, and to 249.5±6.2 μm (n=104, P=0.009) 2 months after surgery.
Discussion
Our results indicate that diabetes did not influence significantly the thickening of the macular regions after uncomplicated cataract surgery.
Similar content being viewed by others
Introduction
The aim of this prospective study was to assess the effect of diabetes on the thickening of the macular regions following cataract surgery. We have already demonstrated in our previous paper1 that a significant increase can be detected on the postoperative 7–60 days period in the perifoveal 3.0 mm and 6.0 mm sectors either calculated alone or averaged together with the foveal value after uncomplicated cataract surgery. Optical coherence tomography (OCT) was employed to determine the thickness of macular regions in the first 60 days after uneventful phacoemulsification and foldable posterior chamber intraocular lens (PC-IOL) implantation in diabetic patients. OCT is an objective, non-contact, non-invasive, well tolerated and highly reproducible method for quantitative retinal thickness measurements, with good reproducibility and with approximately 10 μm resolution.2
Materials and methods
In a prospective study 18 eyes of 18 diabetic patients (DM group) were analyzed and compared to 53 eyes of 53 nondiabetic patients (NORMAL group). Sixteen diabetic patients were treated by oral antidiabetic agents, two people by insulin. The diabetic group was established by the diagnosis of internist, all patients required oral antidiabetic or insuline treatment. Moreover, relevant laboratory data were also available. Since all parameters (preoperative and postoperative thickness of macular regions in the operated and non-operated contralateral eyes, blood sugar levels) of the insulin-dependent patients were in the range of the noninsulin-dependent ones, all data were enrolled into one single diabetic group.
Cataract surgery was performed under topical anaesthesia using the standard technique by one experienced surgeon. After clear corneal incision, capsulorhexis was performed by forceps under Amvisc Plus (sodium hyaluronate, Bausch and Lomb Inc, Rochester, NY, USA) followed by the ‘divide and conquer’ phacoemulsification method. Hydrophobic acrylic PC-IOL was implanted ‘in the bag’ in all patients, the viscoelastic material was removed carefully from anterior chamber and from behind PC-IOL according to the two ‘two-compartment technique’ by Tetz.3
Any intraoperative, postoperative complication, macular disease (eg age-related macular degeneration), medication for glaucoma, uveitis and other diseases that might cause macular oedema were excluded. Patients with severe non-proliferative and proliferative diabetic retinopathy according to the international clinical diabetic retinopathy and diabetic macular oedema disease severity scale, as well as patients with any previous intraocular surgery, were also excluded from the study. The perioperative and postoperative treatment was the same in all patients.
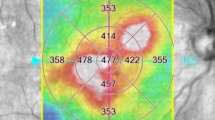
Before OCT examination pupils were dilated in all cases with 1% tropicamide (Mydrum, Chauvin ankerpharm GmbH, Berlin, Germany) or phenylephrine 2.5%, measurements were done on both eyes with the fellow eye serving as control (CONTROL). OCT examinations were performed in the fovea and perifoveal zones (fovea+3.0 mm, fovea+6.0 mm ring quadrants) according to the regions determined in ETDRS study on the preoperative day (PRE) and on postoperative days 1 (P1), 7 (P7), 30 (P30) and 60 (P60). Thickness values of the following macular regions were calculated: the minimal, central value (C), foveal value (F), the average of fovea+3 mm perifoveal ring (F+3 mm, incl. 5 zones), average of 3 mm perifoveal ring (3 mm, incl. 4 zones), fovea+6 mm perifoveal ring (F+6 mm, incl. 9 zones), average of 6 mm perifoveal ring (6 mm, incl. 8 zones) (Figure 1). OCT measurement was implemented along six radial scans of 6.0 mm length centered on foveola. The macular thickness map was derived from data of the 6 radial scans. The thickness map represents the average thickness of the foveolar (1.0 mm diameter central circle area) and 3.0 mm perifoveal (ring area between 1 mm and 3 mm in diameter resulting in a 2.5 mm wide perifoveal ring, inner macular region) and 6.0 mm perifoveal (ring area between 1 mm and 6 mm in diameter resulting in a 5.5 mm wide perifoveal ring, inner+outer macular region) regions divided into superior (S, 46–135°), nasal (N, 136–225°), inferior (I, 226–315°) and temporal (T, 316–45°) quadrants (Figure 1). Only macular maps calculated from high-quality radial scans were included. Therefore, in the DM group one eye and in the NORMAL group two eyes were rejected on the postoperative 1 day due to moderate corneal oedema preventing good quality image acquisition. Later on, patients were lost from follow-up due to non-compliance or attendance on inappropriate postoperative day. This resulted in decreasing the number of eyes measured in the case of the DM group to: 17 on P1, 15 on P7, 14 on P30 and 13 on P60 day; in the NORMAL group: 51 eyes on P1 and P7, 49 on P30 and 47 on P60 day. Accordingly, the number of the averaged macular zones as calculated by our naming convention mentioned above decreased as follows: n × 1 of C and F, n × 5 of C+3 mm, n × 4 of 3 mm, n × 9 of F+6 mm and n × 8 of 6 mm region (n=number of eyes). The result of CONTROL eye was only included when the value of the corresponding OP eye could be calculated.
Left eye data were converted into the right eye form to preserve the corresponding sector positions.
For statistical analysis Student's t-test was used, P<0.05 value was considered as significant.
Results
The DM group of 18 patients included 10 females and 8 males; mean age of group: 64.3±6.4 years (mean±SD). The NORMAL nondiabetic group consisted of 53 patients, 26 females and 26 males; mean age of group: 70.3±8.8 years. No statistical difference could be found concerning age between DM and NORMAL groups (P=0.12).
The mean duration of diabetic anamnesis showed 49.9±23.4 months (mean±SD, 3–120 months), in females 53±22.4 months (24–96 months), while in male patients 46.1±24.4 months (3–120 months).
Aim I: To measure the change of macular thickness in diabetic (DM group) and nondiabetic patients (NORMAL group), the values of operated eye (OP) are compared I.A.) to the fellow, non-operated eye (CONTROL) and I.B.) to preoperative baseline value of the operated eye (PRE). Values were calculated on PRE, P1, P7, P30 and P60 days on the C, F, F+3 mm, 3 mm, F+6 mm and 6 mm regions of macula.
Study design:

AIM I.A.: The thickness values increased significantly both in DM OP and NORMAL OP groups as compared to corresponding CONTROL on P7, P30 and P60 days in the F+3 mm, 3 mm, F+6 mm and 6 mm regions. Moreover, the change was significant also in the F region on P30 day in both groups (Table 1).
AIM I.B.: Similarly, macular thickness values increased significantly both in DM OP and NORMAL OP groups as compared to the corresponding PRE groups on P7, P30 and P60 days in the F+3 mm, 3 mm, F+6 mm and 6 mm regions, and the change proved to be significant also in the F region on P30 day in DM group (Table 2).
AIM II.A., AIM II.B.

No significant difference could be found between the corresponding regions of DM and NORMAL groups either in the initial or in the postoperative values in the case of the OP (AIM II.A., Table 3) and CONTROL eyes (AIM II.B., Table 4).
The preoperative thickness of regions in the DM groups was slightly higher with only 0.1 % (F+6.0 mm region)—3 % (F region) as compared to NORMAL groups. Although the relative change of macular thickness was moderate postoperatively, it was not significantly, but unequivocally higher in the DM group as compared to the NORMAL on the postoperative first week (5.7 vs 3.5%), first month (7.4 vs 5.6%), and second month (7.2 vs 5.3%) eg in the perifoveal 6.0 mm zone (Figure 2).
The preoperative value of macular thickness did not correlate to the duration of diabetic anamnesis either in the operated or in the control eyes.
Discussion
OCT is a new diagnostic tool, which gives a high-resolution, cross-sectional image about the change of the retina (and chorioidea) in the living structure in vivo. The eye is illuminated with a near-infrared light and the technique is non invasive. Since it is a so-called ‘non-contact’ method, it is well tolerated by the patients. Dilation of the pupil helps to perform the examination, but it is not absolutely necessary. Reproducibility of the method is very good, its accuracy is around 10 μm.4 It is mainly useful in the examination of the changes of the anatomical structures of the macular area (oedema, chorioideal neovascularisation, retinal pigmentepithel detachment, detachment of the neurosensory retina), and in the examination of the disorders of the vitreo-retinal surface such as vitreo-macular traction, epiretinal membrane.2, 5
The results of ophthalmoscopy, fluorescein angiography and ultrasound examination is supplemented by the possibility of the anatomic examination of the retina, which may facilitate diagnosis and therapy. OCT provides a quantitative measurement and changes in the parameters may allow us to quantitatively assess the progression of diseases and the success of therapy4, 5, 6, 7, 8, 9, 10
Similarly to our previous study1 on nondiabetic patients, no significant thickness change in any sectors of the foveal and perifoveal retina were found in the diabetic group on the first postoperative day as compared to the corresponding preoperative values. A significant increase could be detected however on the postoperative first week, first and second months in the diabetic group, similarly to the nondiabetic one.
On the other hand, no significant difference could be detected in the thickness value in any macular regions between the corresponding diabetic and nondiabetic groups on the preoperative and postoperative 1, 7, 30 and 60 days either in the operated or in the control eyes.
The thickness change was found to be nonsignificantly higher in the diabetic group compared to the nondiabetic group, which might be attributed on the one hand to the high sensitivity of the OCT method. On the other hand, presumably, the affected microvasculature in diabetic patients could cause the higher increase of perifoveal retinal thickness. Although the vascular laesion caused by diabetes could not be detected by significant preoperative differences of the macular region thickness, the postoperative fallibility of the perifoveal microvasculature might be indicated by the slightly higher preoperative thickness and the enhanced postoperative thickening of perifoveal regions.
Chinese authors performed OCT examinations 1 week after uneventful cataract surgery on 80 eyes, and although the average preoperative foveal thickness increased, the difference proved to be non significant (P>0.05). On the other hand, they proved that there was a significant correlation (P<0.05) between the amount of phaco energy used and the postoperative macular thickness.11
In another study the change of retinal thickness was measured in 15 different points of the posterior part of the retina half an hour after cataract extraction in a small number of patients (10 eyes), and there was no significant change (P=0.8) compared to the preoperative values.12
Sourdille found macular thickening and decreased visual acuity in 11 eyes out of 41 after uncomplicated cataract extraction.13
A recent study interestingly showed decreased pericentral retinal thickness in diabetic patients with minimal or no diabetic retinopathy compared to healthy controls, which might be explained by the loss of intraretinal neural tissue in the earliest stage of diabetic retinopathy.14
Kim found 22% incidence of macular edema on fifty diabetic eyes by OCT, and he demonstrated that both duration of diabetes and insulin dependence were associated with reduced visual improvement.15
Lang also found that with the OCT, structural changes and quantitative assessment of macular edema have become feasible as determined with retinal thickness and volume, and OCT is more sensitive to small changes than slit-lamp biomicroscopy.16
Postoperative macular oedema is explained by the damage of the blood-retinal barrier.17, 18 On the other hand, no correlation was found between the inflammatory signs in the anterior chamber (‘flare’) and macular thickness. According to their opinion, damage to the blood-retinal barrier and consequent thickening of the macular area may happen without the damage of the blood/aqueous barrier.
Increase in the retinal thickness of the perifoveal 6.0 mm diameter area can be demonstrated by OCT in the 7–60 days postoperative period in diabetic patients after uncomplicated phacoemulsification and IOL implantation. The minimum values measured in the fovea by themselves are not suitable to evaluate the postoperative macular oedema. Changes of the perifoveal 3.0 or 6.0 mm diameter areas themselves or measured together with the foveal (minimum) values, are much more suitable to characterize the postoperative macular oedema.
Our results indicate that diabetes did not influence significantly the thickening of the macular regions after uncomplicated cataract surgery. However, the postoperative perifoveal macular thickness change was found to be nonsignificantly higher in the diabetic group compared to the nondiabetic group, which might be attributed to the high sensitivity of the OCT method.
With the help of the objective, non invasive, good reproducible OCT measurements, anatomical changes of the retina in the postoperative period can be well followed. Due to its high sensitivity, OCT is suitable to demonstrate the minimal increase of the perifoveal retinal thickness even 2 months after surgery.
References
Biro Z, Balla Z, Kovacs B . Change of foveal and perifoveal thickness measured by OCT after phacoemulsification and IOL implantation. Eye 2008; 22 (1): 8–12.
Hee MR, Izatt JA, Swanson EA, Huang D, Schuman JS, Lin CP et al. Optical coherence tomography of the human retina. Arch Ophthalmol 1995; 113: 325–332.
Tetz MR, Holzer MP . Two compartment technique to remove ophthalmic viscosurgical devices. J Cataract Refract Surg 2000; 26: 641–643.
Voo I, Mavrofrides EC, Puliafito CA . Clinical applications of optical coherence tomography for the diagnosis and management of macular diseases. Ophthalmol Clin North Am 2004; 17 (1): 21–31.
Puliafito CA, Hee MR, Lin CP, Reichel E, Schuman JS, Duker JS et al. Imaging of macular diseases with optical coherence tomography. Ophthalmology 1995; 102: 217–229.
Sandhu SS, Birch MK, Griffiths PG, Talks SJ . Short term effects of focal argon laser treatment in diabetic maculopathy as demonstrated by optical coherence tomography. Retina 2007; 27 (1): 13–20.
Alkuraya H, Kangave D, Abu El-Asar AM . The correlation between optical coherence tomographic features and severity of retinopathy, macular thickness and visual acuity in diabetic macular edema. Int Ophthalmol 2005; 26 (3): 93–99.
Gibran SK, Khan K, Jungkim S, Cleary PE . Optical coherence tomographic pattern may predict visual outcome after intravitreal triamcinolone for diabetic macular edema. Ophthalmology 2007; 114 (5): 890–894.
Sachdev N, Gupta V, Abhiramamurthy V, Singh R, Gupta A . Correlation between microaneurysm closure rate and reduction in macular thickness following laser photocoagulation of diabetic macular edema. Eye 2008; 22 (7): 975–977.
Arevalo JF, Fromow-Guerra J, Quiroz-Mercado H, Sanchez JG, Wu L, Maia M Berrocal MH, et al. Pan-American Collaborative Retina Study Group. Primary intravitreal bevacizumab (Avastin) for diabetic macular edema: Results from the Pan-American Collaborative Retina Study Group at 6-month follow-up. Ophthalmology 2007; 114 (4): 743–750.
Cheng B, Liu Y, Liu X, Ge J, Ling Y, Zheng X . Macular image changes of optical coherence tomography after phacoemulsification. Zhonghua Yan Ke Za Zhi 2002; 38 (5): 265–267.
Grewing R, Besker H . Retinal thickness immediately after cataract surgery measured by optical coherence tomography. Ophthalmic Surg Lasers 2000; 31 (3): 215–217.
Sourdille P, Santiago PY . Optical coherence tomography of macular thickness after cataract surgery. J Cataract Refract Surg 1999; 25 (2): 256–261.
Biallosterski C, van Velthoven ME, Michels RP, Schlingemann RO, Devries JH, Verbraak FD . Deacreased OCT-measured pericentral retinal thickness in patients with diabetes mellitus type 1 with minimal diabetic retinopathy. Br J Ophthalmol 2007; 91 (9): 1135–1138.
Kim SJ, Equi R, Bressler NM . Analysis of macular edema after cataract surgery in patients with diabetes using optical coherence tomography. Ophthalmology 2007; 114: 881–889.
Lang GE . Optical coherence tomography findings in diabtic retinopathy. Dev Ophthalmol 2007; 39: 31–47.
Konari K, Sawada Z, Zhong Y, Isomura H, Nakagawa T, Mori M . Development of the blood-retinal barrier in vitro: Formation of tight junctions as revealed by occludin and ZO-1 correlates with the barrier function of chick retinal pigment epithelial cells. Exp Eye Res 1995; 61: 99–108.
Vinores SA, Amin A, Derevjanik NL, Green WR, Campochiaro PA . Immunohistochemical localisation of blood-retinal breakdown sites associated with post-surgical macular edema. Histochem J 1994; 26: 655–665.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Biró, Z., Balla, Z. OCT measurements on the foveal and perifoveal retinal thickness on diabetic patients after phacoemulsification and IOL implantation. Eye 24, 639–647 (2010). https://doi.org/10.1038/eye.2009.164
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.164
Keywords
This article is cited by
-
Retinal thickness changes due to phacoemulsification in patients with diabetes
Spektrum der Augenheilkunde (2024)
-
Evaluation of changes in choroidal thickness after implantable collamer lens surgery in high myopia patients with graves’ Ophthalmopathy (inactive phase)
BMC Ophthalmology (2020)
-
Influence of cataract surgery on macular thickness: a 6-month follow-up
Wiener klinische Wochenschrift (2015)