Abstract
Pigment cells in the anterior vitreous (Shafer's sign) are known to be associated with retinal breaks. We sought to identify the reproducibility of Shafer's sign between different grades of ophthalmic staff. In all 47 patients were examined by a consultant vitreo-retinal surgeon, a senior house officer (SHO) and optician for Shafer's sign.
Cohen's kappa for consultant vs SHO assessment of Shafer's sign was 0.55 while for consultant vs optician assessment, kappa was 0.28.
Retinal tears were present in 63.8% of our series. Consultant assessment of Shafer's sign with fundoscopy findings, we found specificity to be 93.5% while sensitivity was 93.8%. Kappa for consultant assessment of Shafer's sign vs break presence was 0.86.
Consultant and SHO assessment of Shafer's sign is of moderate agreement while optician assessment is fair. These results suggest a relationship between training and the assessment of Shafer's sign. We feel this study suggests caution in undue reliance on Shafer's sign particularly for inexperienced members of staff.
Similar content being viewed by others
Main
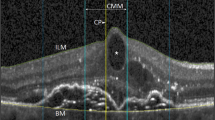
Pigment cells in the anterior vitreous (Shafer's sign)1 are known to be associated with retinal breaks. We sought to identify the reproducibility of Shafer's sign between different grades of ophthalmic staff.
The anterior vitreous of 47 patients was examined for pigment cells. Each patient was examined by a consultant vitreo-retinal surgeon (RRG), a senior house officer, and optician. Junior staff were of mixed experience levels. None had had any specific vitreo-retinal training.
Dilated binocular indirect funduscopy with indentation was then performed (by RRG). The presence of Shafer's sign was classed as positive or negative and was recorded prior to fundal examination to minimise the risk of selection bias.
Agreement was found between consultant and senior house officer (SHO) assessment in 78.2% (36/46 cases) (Table 1). Cohen's kappa for consultant vs SHO assessment was 0.55 (95% confidence interval 0.32–0.80).
Agreement between consultant and optician assessment was found in 61.7% (29/46 cases) (Table 2). Cohen's kappa for consultant vs optician assessment was 0.28 (95% CI 0.02–0.54).
Retinal tears were present in 63.8% (30/47 cases) of our series (Table 3). Comparing the consultant assessment of Shafer's sign with funduscopy findings, we found specificity to be 93.5% (95% CI 84.7–100%) while sensitivity was 93.8% (95% CI 81.6–100%). Kappa for consultant assessment of Shafer's sign vs break presence was 0.86 (95% CI 0.70–1.00).
A history of severe blunt trauma was present in two cases.
Our series compare well with previously published data.2, 3, 4, 5, 7
The agreement between consultant assessment of Shafer's sign and break presence is good.6 Our series contained two false positives, one presumably due to severe blunt trauma, the other misread due to clumps of vitreous haemorrhage. The false negative had an atrophic hole. The vitreous haemorrhage was excluded from SHO and optometrist assessment.
Our Kappa indices indicate that the agreement between SHO assessments of Shafer's sign is of moderate agreement with the consultant's, while optician assessment is fair.6 It can be seen from Tables 1 and 2 that it was the junior ‘false-negatives’ that were the largest source of disagreement suggesting that difficulties lay in detecting a positive Shafer's sign. These results suggest a relationship between training and the assessment of Shafer's sign. We feel this study suggests caution in undue reliance on Shafer's sign particularly for inexperienced members of staff.
References
Shafer DM, Stratford DP . Binocular indirect ophthalmoscopy. In: Schepens CL, Regan CDJ, (eds). Controversial Aspect of the Management of Retinal Detachment. J & A Churchill: London, 1965, p 51.
Tanner V, Harle D, Tan J, Foote B, Williamson T, Chignell A . Acute posterior vitreous detachment: the predictive value of vitreous pigment and symptomatology. Br J Ophthalmol 2000; 84: 1264–1268.
Brod R, Lightman D, Packer A, Saras H . Correlation between vitreous pigment granules and retinal breaks in eyes with acute posterior vitreous detachment. Ophthalmology 1991; 98: 1366–1369.
Hamilton A, Taylor W . Significance of pigment granules in the vitreous. Brit J Ophthal 1972; 56: 700–702.
Hikichi T, Trempe C . Relationship between floaters, light flashes, or both, and complications of posterior vitreous detachment. Am J Ophthalmol 1994; 117: 593–598.
Altman DG . Practical Statistics for Medical Research. CRC: Chapman and Hall, 1991, p 404.
Lightman D . Relationship between floaters, light flashes, or both, and complications of posterior vitreous detachment. Am J Ophthalmol 1994; 118 (5): 683–684.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Qureshi, F., Goble, R. The inter-observer reproducibility of Shafer's sign. Eye 23, 661–662 (2009). https://doi.org/10.1038/eye.2008.9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2008.9