Abstract
Purpose
To establish a scoring system to triage patients presenting with symptoms of flashes and floaters to allow safe differentiation between those with retinal tears and detachments, versus uncomplicated posterior vitreous detachments (PVDs).
Methods
Prospective and retrospective audits of 153 patients presenting to eye casualty and vitreoretinal clinics to ascertain the clinical features most likely to be associated with retinal pathology, rather than simple PVD. We then developed a scoring system, which was applied to 160 patients in a further prospective audit.
Results
The significant risk factors, symptoms and signs were identified then given a number related to their importance: male sex 1, myopia 1, blurred vision 2, shadow 2, vitreous haemorrhage 3, tobacco dust 4. The scores were summed and a total score > 3 was more likely to be a complicated PVD. Sensitivity of the scoring system was 90% (confidence interval (CI) 68.3–98.8%), specificity 80% (CI 73.2–86.9%), positive predictive value 40% (CI 25.7–55.7%), and negative predictive value 98.26% (CI 93.9–99.8%).
Conclusions
The BElfast Retinal Tear and detachment Score is an easy to apply scoring system, which has a high sensitivity and negative predictive value i.e. nearly all retinal tears or detachments are detected by the scoring system.
Similar content being viewed by others
Introduction
It is extremely common for patients to present with monocular floaters and flashing lights to primary care physicians, opticians and eye casualty. The majority of patients are diagnosed with uncomplicated posterior vitreous detachment (PVD) [1]. Indeed, the prevalence of PVD is 87% in those over the age of 80 [2]. However, some patients will also have PVD complicated by a retinal tear (RT), which if treated in a timely manner can prevent retinal detachment (RD) [3]. Hollands et al. reported that the incidence of RT in patients presenting to an ophthalmologist with an acute PVD was 14% [4]. In cases of PVD combined with vitreous haemorrhage, the incidence of RT has been reported to be as high as 70% [5]. In the 6 weeks following an initial uncomplicated PVD, the chance of developing a RT is 3.4%. A delayed RT most commonly occurs following symptoms of new floaters [4].
Many studies have reported clinical features predisposing patients to a higher risk of acute retinal pathology in the context of PVD. These include previous ocular surgery, family history of RD, previous RD/RT, myopia, ocular trauma, and male sex [1, 4, 6,7,8,9]. More recently, the symptom of ‘subjective reduction in vision’ has shown a high predictive value for acute retinal pathology [4].
A previous meta-analysis concluded that symptoms and signs most suggestive of a complicated PVD were: monocular field loss, vitreous haemorrhage, or pigment cells in the vitreous. They proposed that patients with presumed PVD associated with monocular visual field loss, subjective or objective visual reduction, vitreous haemorrhage, or pigment on examination, should be seen the same day in eye casualty. They also recommended that those without high-risk features were seen by an ophthalmologist within 1–2 weeks and also given RD warning symptom advice [4].
Triage scoring systems are commonly used in main emergency departments, and are vital to rate patients’ clinical urgency and provide safe patient care [10]. Scoring systems are known to help enable clinicians to predict outcomes, stratify risk, and triage patients appropriately [11]. To our knowledge there is no current scoring system for patients with acute PVDs. We aimed to prospectively assess symptoms and signs predictive of acute retinal pathology in the context of PVD in patients presenting to eye casualty and outpatient clinics, and to form a simple scoring system for use by referring clinicians. This should enable us to stratify patients according to risk and triage them appropriately, thereby reducing unnecessary eye casualty attendances and prioritising those with potentially sight-threatening complications.
Materials and methods
This study was conducted at the Royal Victoria Hospital, Belfast in the walk-in ophthalmic eye casualty and vitreoretinal outpatient clinics.
For this study we defined ‘complicated’ PVD as those with an acute PVD associated with a RT or a RD, or those with no fundal view secondary to vitreous haemorrhage, preventing full assessment. First, we performed a prospective audit to capture the frequency of various clinical and demographic features in patients presenting with either a complicated or uncomplicated PVD. We included 100 consecutive patients presenting to 2 individual doctors on the United Kingdom Ophthalmology Specialty Training programme within our walk-in eye casualty. Any patient presenting with uniocular floaters and/or flashing lights were included. The data was meticulously collected on pre-designed data extraction forms. To inform the choice of data to collect, we included risk factors, symptoms, and signs previously documented to be associated with higher risk of RT. We had previously completed retrospective audits of the notes of 53 patients presenting to eye casualty or vitreoretinal clinic with a RT or RD, and found the same common risk factors as mentioned in the literature.
The results were analysed, comparing the frequency of each risk factor, symptom or sign between those with complicated versus uncomplicated PVD. Percentages of the clinical features were calculated and analysed by the comparison of proportions using the N−1 Chi squared test. This determined which factors reached an appropriate p value (p < 0.05) to accept that there was a valid difference between the groups. Using these results, we developed a scoring system (as shown in Table 1) to help stratify the risk of having a complicated versus uncomplicated PVD. The score for the patient is then totalled and an overall score is recorded.
The scoring system was based on the frequency with which each of the features (reaching statistical significance) was recorded in the complicated PVD group compared with the uncomplicated PVD group. Tobacco dust and vitreous haemorrhage that were noted in most cases of complicated PVD and fewer cases of uncomplicated PVD were allocated scores of 4 and 3 respectively, while myopia and male sex that were seen to be associated with complicated PVDs (but were also noted frequently in uncomplicated PVDs) were allocated a score of 1. Symptoms of blurred vision and shadow were observed to be more representative of a complicated PVD than myopia or male sex, but less so than tobacco dust or vitreous haemorrhage, therefore were allocated scores of 2. By trialling this scoring system on a sample of the patients on whom we had collected data, we found that a total of 4 points captured most of those with a complicated PVD, and excluded many of those with an uncomplicated PVD.
The next stage involved retrospectively applying the scoring system to all patients who attended eye casualty over a 3-week period with diagnoses of PVD, RT, RD, vitreous haemorrhage, ocular migraine, and other retinal pathology. We searched the diagnoses recorded on our electronic eye casualty database to retrieve this information. We calculated the sensitivity, specificity and positive and negative predictive values of the overall score to distinguish between those with complicated and uncomplicated PVD.
Results
The demographics for the 100 patients included in the prospective audit are shown in Table 2. They were separated into two groups: PVD or other (76); and RT or RD (24).
Tobacco dust was found to be the most crucial sign when assessing patients with suspected retinal breaks, with this sign present in 94% of RTs or RDs (22/24). If this sign is present there will almost certainly be a break in the retina. Other features that reached statistical significance were vitreous haemorrhage, symptoms of shadow or blurred vision, drop in recorded visual acuity, and myopic refraction. Male sex had a higher incidence of RTs also.
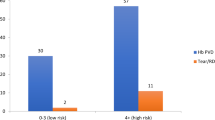
The scoring system was subsequently applied to 160 patients, with 115 of these scoring 0–3 points, and 45 scoring 4 or more points. 1 RT and 1 RD scored <4 points, and 18 RTs or RDs scored 4 or more points. Of the other 27 patients scoring 4 or more points, there were 12 PVDs combined with some degree of vitreous haemorrhage, 13 with vitreous haemorrhages preventing fundal assessment (many of these were secondary to proliferative diabetic retinopathy), and 2 operculated retinal holes. All of the simple PVDs (91) scored 0–3 points. Other diagnoses in this group included ocular migraines, post-vitreoretinal surgery flashes and floaters, macular hole, and epiretinal membrane. Sensitivity of the test in detecting a complicated PVD (i.e., with a RT or RD) was 90%, specificity 80%, positive predictive value 40%, and negative predictive value 98.26% (see Table 3 for confidence intervals; Fig. 1).
Discussion
A scoring system is helpful in the setting of the presumed diagnosis of PVD because it is a very common presentation to primary care, and the majority of patients have uncomplicated PVDs not requiring any further treatment.
Similar to other studies, the findings of tobacco dust, vitreous pigment or haemorrhage, and symptoms of a shadow or blurred vision, drop in recorded visual acuity, male sex and myopic refraction were highly predictive of an underlying diagnosis of RT, and thus these risk factors were included in our proposed scoring system [4, 9, 12].
A previous study performed in an English eye casualty department analysed the diagnoses of 170 patients presenting with flashes and floaters, to investigate whether the symptoms, demographics, and past ocular history had any correlation with the incidence of retinal breaks compared with simple PVDs and other benign diagnoses. They found no robust link between the presentation of flashes and floaters and the diagnosis of retinal break or PVD, which supports our findings. However, they concluded that gender and myopia were not relevant, although we found them to be significant enough to be included in the scoring system, but not enough to individually be a reason for urgent review [13].
An American study of 589 patients aimed to identify risk factors for RTs in patients presenting with floaters. They demonstrated that the key clinical findings were visual symptoms of “diffuse dots” (52%), non-pigmented vitreous cells (65%), and vitreous or pre-retinal blood (92%). The symptoms of diffuse dots and vitreous cells could be explained by the presence of vitreous haemorrhage, which was also found to be a very high-risk feature in our study [12].
Other studies have shown varying degrees of relevance of the risk factors for RT or RD as mentioned above, some of which support our findings, but overall show large variation. Overall, most other studies recommend prompt early evaluation of the patients with flashes and floaters, regardless of the patient’s risk factors [6,7,8, 14]. Our study demonstrates that it is possible to be more selective when assessing patients with flashes and floaters. Application of this scoring system could prevent unnecessary referrals and allow for better utilisation of eye casualty resources.
This was a real-life study, with recognisable flaws. We were relying on the history from the patient to collect information on risk factors, which may not always have been accurate, particularly for family history and trauma. There was a small sample of patients, with only 24 in the RT and RD group. Myopia was determined in our study by the refractive data provided by an optometry referral letter, by examining the patients’ glasses, or simply by asking the patient about their use of distance glasses or contact lenses. This should have captured any refractive error of more than around −0.5 dioptres, but was vulnerable to errors. Finally, the data were collected by only 2 assessors, who had designed the audit, so there was a risk of collection bias.
We conclude that the BElfast Retinal Tear and detachment Score (BERT Score) is an easy to apply test which has a high sensitivity and negative predictive value i.e. nearly all RTs or RDs are detected by the scoring system. This means that patients who do not have a tear or detachment will not be unnecessarily referred to eye casualty. This simple scoring system could potentially be used by primary care practitioners assessing patients with presumed PVD. The clinical signs of vitreous haemorrhage and tobacco dust may be challenging for an Accident and Emergency doctor to elicit, without further training, but should be easily detectable by an optometrist, and by an ophthalmic nurse practitioner. We propose that all patients with a score of 3 or greater are referred urgently to eye casualty. Those with a score of less than 3 can be safely assessed by opticians or ophthalmic nurse practitioners with a dilated fundus examination, and only referred to eye casualty if there are additional concerns. However, before this scoring system is more widely implemented, it needs to be validated.
Summary
What was known before
-
Presence of tobacco dust and vitreous haemorrhage, symptoms of blurred vision and shadow, and background of myopia and male sex are associated with higher likelihood of having a retinal tear or detachment in patients presenting with flashes and floaters.
What this study adds
-
A simple to use scoring system based on the presenting features of patients with flashes and floaters that can be applied to differentiate between those with complicated and uncomplicated PVDs.
-
The scoring system has a high sensitivity and negative predictive value.
References
Hurst J, Johnson D, Law C, Schweitzer K, Sharma S. Value of subjective visual reduction in patients with acute-onset floaters and/or flashes. Can J Ophthalmol. 2015;50:265–8.
Hikichi T, Hirokawa H, Kado M, Akiba J, Kakehashi A, Yoshida A, et al. Comparison of the prevalence of posterior vitreous detachment in whites and Japanese. Ophthalmic Surg. 1995;26:39–43.
Davis MD. Natural history of retinal breaks without detachment. Arch Ophthalmol. 1974;92:183–94.
Hollands H, Johnson D, Brox AC, Almeida D, Simel DL, Sharma S. Acute-onset floaters and flashes: is this patient at risk for retinal detachment? JAMA. 2009;302:2243–9.
Byer NE. Natural history of posterior vitreous detachment with early management as the premier line of defense against retinal detachment. Ophthalmology. 1994;101:1503–13. discussion 1513-1514
Byer NE. Prognosis of asymptomatic retinal breaks. Mod Probl Ophthalmol. 1974;12:103–8.
Rowe JA, Erie JC, Baratz KH, Hodge DO, Gray DT, Butterfield L, et al. Retinal detachment in Olmsted County, Minnesota, 1976 through 1995. Ophthalmology. 1999;106:154–9.
Tielsch JM, Legro MW, Cassard SD, Schein OD, Javitt JC, Singer AE, et al. Risk factors for retinal detachment after cataract surgery. A population-based case-control study. Ophthalmology. 1996;103:1537–45.
Mitry D, Charteris DG, Fleck BW, Campbell H, Singh J. The epidemiology of rhegmatogenous retinal detachment: geographical variation and clinical associations. Br J Ophthalmol. 2010;94:678–84.
Melot C. To score or not to score during triage in the emergency department? Intensive Care Med. 2015;41:1135–7.
Zachariasse JM, van der Hagen V, Seiger N, Mackway-Jones K, van Veen M, Moll HA. Performance of triage systems in emergency care: a systematic review and meta-analysis. BMJ Open. 2019;9:e026471.
Boldrey EE. Risk of retinal tears in patients with vitreous floaters. Am J Ophthalmol. 1983;96:783–7.
Diamond JP. When are simple flashes and floaters ocular emergencies? Eye. 1992;6(Pt 1):102–4.
Gariano RF, Kim C-H. Evaluation and management of suspected retinal detachment. Am Fam Phys. 2004;69:1691–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
McCullagh, D., Higham, A. & Best, R. The BElfast Retinal Tear and detachment Score (BERT Score). Eye 35, 1427–1430 (2021). https://doi.org/10.1038/s41433-020-1025-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-1025-7