Abstract
Purpose
Severe cases of blepharospasm resistant to botulinum toxin represent a challenging clinical problem. Over the last 10 years, we have adopted a staged surgical management of these cases with an initial upper lid orbicularis myectomy (combined with myectomy of procerus and corrugator supercilius as appropriate) and then 4–6 months later a brow suspension with autologous fascia lata. The aim of this study was to assess the outcome of this staged surgical approach.
Materials and methods
A questionnaire was sent to all patients who had undergone the procedure and the clinical records reviewed.
Results
Fourteen patients had undergone the procedure of which 13 were alive. They were sent a questionnaire and 10 of them responded. All had both procedures. Eight of the 10 reported great benefit from the surgery, one some benefit, and one was worse off. All patients still required botulinum toxin injections after the surgery.
Conclusions
Majority, but not all, of the patients in our series greatly benefitted from this staged surgical approach.
Similar content being viewed by others
Introduction
Patients with severe blepharospasm, whose symptoms are not controlled by botulinum toxin injections, are a difficult management problem for whom a number of surgical options have been tried.
Two operations, in particular, have been tried; the orbicularis myectomy (or strip) and brow suspension. The choice of the procedure classically depends upon the clinical presentation, with all types being offered the orbicularis myectomy except for the apraxic (also called the pre-tarsal) type. The proposed aetiology of the apraxic type is considered to differ and to represent a failure of eyelid opening and is clinically characterized by the eyebrows going up and not down with the spasms. The suggestion is that the severe apraxic type should be treated by brow suspension instead.1, 2
It is not clear whether the recognition of the apraxic subtype is helpful in the determination of management. Upper lid orbicularis myectomy has been reported to be of benefit in patients with the apraxic type,3 whereas, conversely, frontalis suspension procedure has been reported to be effective in essential blepharospasm, with the response rate being independent of the subtype.4
Alternative surgical procedures include facial nerve evulsions, but the complications are such that they are considered second-line surgical procedures,5, 6, 7 whereas more recent procedures such as the stimulation of the globus pallidus following electrode insertion are having mixed results.8
The observations, made by one of us (AF), were that the benefit of either myectomy or the brow suspension procedure was small. With the upper lid myectomy, the standard advice is to leave 2 mm rim of muscle behind to ensure eyelid closure and to prevent exposure. This was thought to be quite sufficient to ensure that the symptoms persisted. Equally, the brow or frontalis suspension procedures were also witnessed to do poorly with the patients complaining of severe symptoms and ‘tension’ and could observe the two antagonistic muscles (orbicularis and frontalis) directly competing against each other.
This led to the idea of sequential surgery of first operating to weaken the agonist, the orbicularis oculi muscle, and then to strengthen the antagonist (the frontalis muscle). By doing the surgery sequentially, it gave the opportunity of stopping if the first procedure gave good symptomatic relief.
Materials and methods
Questionnaire
A questionnaire was devised to assess the outcome of surgery and was a combination of Likert scales and free text boxes. In questioning, responses can be affected by ‘framing’. Accordingly, an attempt was made to address each issue twice, once framed positively and once framed negatively.
The questions were
-
1)
What were the best things about the treatment? A free text box was provided.
-
2)
What were the worst things about the treatment? A free text box was provided.
-
3)
Are there things that you can do now, which you could not do before the treatment? ((1) None, (2) a few things, (3) many things, and (4) I can do all the things that I could not do before).
-
4)
Are there things that you cannot do now, which you could do before the treatment? ((1) No more things, (2) a few things, (3) many things, and (4) I have become greatly restricted since my treatment).
-
5)
How much of the time do you find that you regret having the operation? ((1) None of the time, (2) the occasional moment, (3) some of the time, (4) half of the time, (5) most of the time, and (6) all of the time).
-
6)
How has the treatment affected your quality of life? ((1) It has made it much worse, (2) it has made it a little worse, (3) it has made no difference to my quality of life, (4) it has made it a bit better, and (5) it has made it a lot better). Can you give some examples on how it has affected your general quality of life? Free text box was provided.
-
7)
Are you pleased with the outcome of your treatment? ((1) I am always displeased when I think about the outcome, (2) I am often displeased when I think about the outcome, (3) I am occasionally displeased when I think about the outcome, (4) I am neither pleased nor displeased about the outcome, (5) I am occasionally pleased when I think about the outcome, (6) I am often pleased when I think about the outcome, and (7) I am always pleased when I think about the outcome). What do you find most pleasing about the outcome? Free text box was provided.
-
8)
Would you recommend the same treatment to another person suffering from a similar condition to yours? ((1) I would never recommend the operation, (2) I would strongly advise against the operation, (3) I would advise them to make their own decision, (4) I would recommend the operation, and (5) I would strongly recommend the operation). What factors guide your advice? Free text box was provided.
-
9)
If you had known what you know now, would you still have gone ahead with it? ((1) Definitely not, (2) probably not, (3) not sure, (4) probably, and (5) certainly). Why? Free text box was provided.
-
10)
Have you benefitted from the treatment? ((1) No, I am a lot worse off, (2) no, I am a little worse off, (3) I have neither gained nor lost from the treatment, (4) yes, I have benefitted a little from the treatment, and (5) yes, I have benefitted a lot from the treatment). In what ways have you benefitted from the treatment? Free text box was provided.
-
11)
If you could change any aspects of the treatment, what would it be? Free text box was provided.
-
12)
Is there any way that the management could be improved? Free text box was provided.
-
13)
Is there anything else that you would like to add that you think is important about the treatment and its outcome that has not been covered? Free text box was provided.
Patients and surgery
Fourteen patients had undergone surgery between June 1997 and May 2006, and of these, one had died. The questionnaires were sent out to 13 patients and there were 10 responses (77%) comprising eight women and two men, all Caucasian and aged between 56 and 75 years (mean 67 years). The length of follow-up ranged from 2 to 10 years.
The surgery was performed in two stages, and all cases in this series were performed by a single surgeon (AF). All patients had an orbicularis oculi strip from the upper lid through a superior skin crease incision. The apraxic or pre-tarsal subgroup (eyebrows go up with the spasms) had no further procedures at this stage, whereas those with essential blepharospasm with the eyebrows going down with their spasms had their corrugator supercilli and procerus muscles removed as well through the same incision. Excess upper lid skin was not removed.
The second operation was performed a minimum of 4 months after the first operation. Autologous fascia lata (AFL) was harvested using a fascia lata stripper through a 4 cm incision and used to perform an upper lid suspension procedure using the Crawford technique (see Collin9 for description). As a technical note, the upper lid skin contracts after the first procedure (this is the rationale for not performing a blepharoplasty procedure) and the skin crease reforms at the site of the stab incisions in the upper lid, which were therefore placed 5–7 mm from the lid margin.
After the surgery, some patients had a ‘honeymoon period’ whereby they did not require dysport injections, but this was transient and by 6 months all patients had resumed injections. When they resumed injections, the standard injection pattern used was very different from that used before surgery. There was no need for injections into the upper lid. Twenty mU of dysport was used 1 cm lateral to the lateral canthus and 20 mU, 1 cm below the first. Additional injections at the site of insertion of the corrugator supercilii muscles (located at the junction of the medial quarter and lateral three quarters of the eyebrow) and in the mid-point of the lower lid were added in as required.
Data analysis
The scores and the free text were analysed separately.
Scores
The aim of the questionnaire was to assess whether the patients were pleased with the outcome of the surgery.
Numerical analysis on such a small sample is limited and should be interpreted with caution. However, it was felt appropriate to check some of the basic features of the instrument. First, two of the items, 4 (Are there things that you cannot do now, which you could do before the treatment?) and 5 (How much of the time do you find that you regret having the operation?), had their scores reversed (by subtracting from 4 and 6, respectively) so that a good outcome was associated with a high score for all the variables.
Principle component analysis was performed extracting factors greater than one and then performing varimax rotation. A scree plot suggested a natural break after the first factor had been extracted that carried an eigenvalue of 6.3. The second factor extracted had an eigenvalue of 1.0. This supported the questionnaire measuring a single dimension.
Accordingly, all the items were combined to generate a single score by combining all the items by addition. The scale then ran from 6 to 41.
All the item totals correlations were greater than 0.7, except for item 4, which was less than 0.2. The Cronbach's α was checked and was 0.94 and did not alter greatly if any one item was deleted from the scale, and this is acceptable.10 For such a limited sample, it was elected to leave item 4 in the scale. The analysis and the conclusions drawn do not differ significantly if it is excluded.
These analyses were performed using SPSS windows version 6.
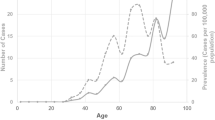
A histogram of the scores is displayed in Figure 1. Nine out of the 10 patients clustered at the top end of the scale. There was one who scored at the bottom end of the scale. The scores give the impression that most of the patients had benefitted greatly from the surgery but that one clearly had not.
Free text analysis
The free text analysis supported the numeric results and also highlighted further features. The free text suggested that eight had greatly benefitted (scoring 33–39). The benefits that they described were an ability to do their hobbies (six), being able to go out alone and to cross roads (four), be able to do housework and chores (three), to read (three), to drive, (three) and to watch television (two).
Seven of these eight used the free text box, for the question as what were the best things about the treatment (one left it blank). The seven comments were
-
Can do anything.
-
Has changed my life.
-
It has made my life so much better.
-
To regain my independence.
-
It has given my confidence back, enhancing the quality of my life.
-
My quality of life is now much improved.
-
Eyes stay open now. More than a million pounds to me.
Among this group, one patient stated that there were many things she could not do but the only example given was that she was ‘unable to put make up on.’ A second also observed that she could not wear make up but considered it a minor problem.
The person who gained equivocal or uncertain benefit, who stated that he was no worse off, was the patient with hemifacial spasm who had had left-sided surgery only. The view expressed was that it was worth a go and that though he had not greatly benefitted, he did not regret the surgery.
The person who was worse off was angry about the operation and considered that he was used as a guinea-pig and did not like the scars on the forehead. He scored the procedure with the lowest attainable marks, with the exception of the question as to whether there were things that he could not do now compared to before, which he scored as one (there were no things that he could not do now, which he could do before).
Under the worse features of the operation, the comments made were (the numbers in parentheses refer to the number of times mentioned)
-
Foreign body feeling in my eye (1);
-
unable to close eyes at night (1);
-
leg problems and difficulty in walking (3);
-
scars above the eyes (2).
The other free text boxes added little and were mostly left blank in keeping with the numerical analyses that suggested that the questions were all tapping the same dimension and were repetitive.
Discussion
There is a clear problem on how to assess the outcome of a new treatment. The first patient, who underwent this, after lengthy discussion and counselling spread over several visits, had had severe pre-operative blepharospasm to the point that she had been house bound for 6 years. She had no benefit from the myectomy but when she came for her 1-month review after the second operation, she was wearing a brand new suit. She had gone shopping on her own. The second case was the same. In addition to being unable to go out, she had also been unable to read and she too regained the ability to go out unaccompanied and could read limited amounts after the surgery.
These results were encouraging but anecdotal. It is difficult to report this in a convincing manner, and numbers are too few to be able to do a randomized control trial and there are no truly robust measurements of disease severity, given its unpredictable and variable nature. This explains the methodology here of a structured questionnaire and adopting a qualitative methodology.11
The aim of this study was to assess simply whether the patients thought that they had benefitted from the surgery. There were only 10 cases, and full instrument validation requires a much larger number. This limitation needs to be born in mind when assessing these analyses. Despite the small numbers, the results were encouraging. The principle component analysis did support a single dimension being measured. The Cronbach α for the scale was 0.94, showing internal consistency.
The questions not only had good face validity but also good construct validity. Those who gave positive comments in the free text box scored high, whereas equivocal or negative comments went with scores in the mid or low range, respectively.
Accordingly, it was gratifying to note that 9 out of 10 clustered at the top of the scale, suggesting that most had received very significant benefit from this surgical approach. These patients represent the subgroup of patients with severe blepharospasm who are unhelped by botulinum toxin injection. The results accord with the clinical impression that this procedure has greatly helped most, but importantly, not all. In the 8 out of 10 who benefitted, the degree of benefit appears to have been large, with restoration of a near normal life style. This applies particularly to those who were unable to go out alone or were unable to cross roads safely, and these in particular regained that ability.
The experience gained here supported the concept that the distinction between essential and apraxic blepharospasm is one of degree rather than type. Patients who underwent procerus and corrugator supercilli weakening converted from the essential to the apraxic type. Blepharospasm can involve more than just the muscles around the eye and can include the muscles around the mouth as well. Thus, the apraxic subtype would fit with the concept of simply representing a more localized disease. Recently, published results show that the apraxic type can also benefit for upper lid orbicularis myectomy.12
A superficially similar operation has been reported by Gillum and Anderson.13 They describe a procedure involving extirpation of all accessible orbicularis, procerus and corrugator superciliaris, along with facial nerve expiration in the postorbicular fascia and combined with browplasty with fixation to frontalis and reinforcement of the levator aponeurosis with ‘gratifying results’. The rationale for the browplasty was to counteract the brow droop that follows facial nerve expirtation and not, as here, a brow suspension to use to the power of frontalis to overcome the residual orbicularis oculi muscle.
The complications of the procedure are as much as one would expect. One patient described sleeping with her eyes open and another of a foreign body sensation probably related to dry eyes and greatly weakened blinking. Three commented on leg problems related to harvesting the fascia lata. Many of these complications refer specifically to the brow suspension and particularly to the donor site. However, the advantages of using AFL are considerable. In particular, compared with an artificial material such as mersilene mesh, any exposure can be treated with systemic antibiotics and will not require removal. Exposure is a particular potential problem for two reasons. First, the spasms mean that the wounds will be under some tension and second, the orbicularis strip will mean that the tissue covering the implanted material will be particularly thin (and that is the explanation for the reported high exposure rate for gold weights in the upper lid as treatment for long-standing seventh nerve palsies where the orbicularis oculi is atrophic).
However, it is clear that this approach is not a panacea for blepharospasm. One patient with (left) hemifacial spasm did not benefit from the surgery. There was also one patient who was not pleased by the results of the surgery. Although he stated that he lost no function as a result of the surgery, he was very dissatisfied with the process, the surgical scars and the leg pain following it. Although several of the patients commented on the good counselling they had received, two thought it could have been better.
In conclusion, the staged procedure of superior orbicularis oculi (combined where appropriate with removal of corrugator supercilii and procerus) followed by a second operation 4–6 months later of brow suspension with AFL is beneficial for a subgroup of patients with severe essential blepharospasm. Careful patient selection and counselling are important, but there is a subgroup who appears to have benefitted greatly from this approach.
References
Elston JS . Idiopathic Blepharospasm and therapeutic ptosis induction. In: Moore P (ed). Handbook of Botulinum Toxin Treatment. Chapter 6. Blackwell Sciences Ltd: Oxford, 1995, pp 71–89.
De Groot V, De Wilde F, Smet L, Tassignon MJ . Frontalis suspension combined with blepharoplasty as an effective treatment for blepharospasm associated with apraxia of eyelid opening. Ophthal Plast Reconstr Surg 2000; 16: 34–38.
Chapman KL, Bartley GB, Waller RR, Hodge DO . Follow-up of patients with essential blepharospasm who underwent eyelid protractor myectomy at the Mayo Clinic from 1980 through 1995. Ophthal Plast Reconstr Surg 1999; 15: 106–110.
Wabbels B, Roggenkamper P . Long-term follow-up of patients with frontalis sling operation in the treatment of essential blepharospasm unresponsive to botulinum toxin therapy. Graefe's Arch Clin Exp Ophthalmol 2007; 245: 45–50.
Waller RR, Kennedy RH, Henderson JW, Kesty KR . Management of blepharospasm. Trans Am Ophthalmol Soc 1985; 83: 367–386.
Frueh BR, Musch DC, Bersani TA . Effects of eyelid protractor excision for the treatment of benign essential blepharospasm. Am J Ophthalmol 1992; 113: 681–686.
Bates AK, Halliday BL, Bailey CS, Collin JR, Bird AC . Surgical management of essential blepharospasm. Br J Ophthalmol 1991; 75: 487–490.
Vagefi MR, Lin CC, McCann JD, Anderson RL . Exacerbation of blepharospasm associated with craniocervical dystonia after placement of bilateral globus pallidus internus deep brain stimulator. Mov Disord 2008; 23: 454–456.
Collin JRO . A Manual of Systematic Eyelid Surgery, 2nd edn. Churchill Livingstone: Edinburgh, London, Melbourne and New York, 1989.
Streiner DL, Norman GL . Health Measurement Scales: A Practical Guide to Their Development and Use, 2nd edn. Oxford University Press: Oxford, 1995.
Hatch JA . Doing Qualitative Research in Education Settings. State University of New York Press: Albany, 2002.
Georgescu D, Vagefi MR, McMullan TFW, McCann JD, Anderson RL . Upper eyelid myectomy in blepharospasm with associated apraxia of lid opening. Am J Ophthalmol 2008; 145: 541–547.
Gillum WN, Anderson RL . Blepharospasm surgery. An anatomical approach. Arch Ophthalmol 1981; 99: 1056–1062.
Author information
Authors and Affiliations
Corresponding author
Additional information
Financial interests: None
Rights and permissions
About this article
Cite this article
Patil, B., Foss, A. Upper lid orbicularis oculi muscle strip and sequential brow suspension with autologous fascia lata is beneficial for selected patients with essential blepharospasm. Eye 23, 1549–1553 (2009). https://doi.org/10.1038/eye.2008.314
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2008.314