Abstract
Purpose
To evaluate the effect of combined intralesional and sub-Tenon's administration of corticosteroids for the treatment of refractory periocular and orbital capillary haemangioma in a retrospective, non-comparative study.
Methods
Seven infants with resistant periorbital and orbital capillary haemangioma who attended our tertiary centre from 2000 to 2005 were treated with an intralesional injection of a mixture of betamethasone 6 mg/cc and triamcinolone 10 mg/cc, by body weight, together with sub-Tenon's infusion of betamethasone 6 mg/cc and triamcinolone 40 mg/cc of a volume of 1 cc, close to the orbital lesion, in the same session. Visual axis, proptosis, pre- and post-treatment changes in four refractive parameters, and parental satisfaction were evaluated.
Results
None of the babies had proptosis or visual axis obstruction after treatment. Mean spherical power decreased by 22.7% (P=0.06). Mean spherical equivalent decreased in 34%, but the difference was not statistically significant (P=0.09). No early or late ocular side effects were observed. Mean intraocular pressure results were normal before and immediately after treatment, and during the follow-up period. Parental satisfaction score during follow-up was 9/10. Mean time to improvement was 96.43±58.3 days.
Conclusions
Combined local corticosteroid administration by posterior sub-Tenon’s infusion and intralesional injection in babies with extensive capillary haemangioma is associated with a satisfactory anatomical and functional outcome and there were no ophthalmic side effects.
Similar content being viewed by others
Introduction
Capillary haemangioma is the most common soft tissue tumour in infancy, with an incidence of 1–2.6%.1 It is more prevalent in female infants and in preterm infants, particularly those weighing less than 1500 g.1, 2, 3 The course is characterized by rapid proliferation in the first year of life, followed by a slow, gradual involution over the next 5–7 years.4, 5 The exact aetiology is not well understood, and may involve aberrant vascular dysgenesis,6 hormonal or immune-mediated processes, infections, and genetic factors. Increased levels of heparin and mast cells may be the contributing factors.7, 8, 9
Periocular haemangiomas warrant close evaluation and may require early active treatment because of their potential to compromise vision by occluding the visual axis, compressing the globe, or expanding into the retrobulbar space.10, 11 They may also induce amblyopia secondary to refractive errors or strabismus. Treatment consists of systemic, topical, or intralesional corticosteroids. Alternatively, Coats et al12 suggested that for orbital lesions, injecting corticosteroids into the posterior sub-Tenon's space may be effective. The aim of this study was to present the anatomical and functional results (pre- and post-treatment refractive data) of combined intralesional and posterior sub-Tenon's corticosteroid administration for the treatment of refractory capillary haemangioma with orbital and periorbital involvement in infants.
Materials and methods
Patients
Data were collected on seven babies treated at our major tertiary centre for extensive and resistant periorbital and orbital haemangioma between 2000 and 2005. Ophthalmologic examination (before and after treatment) was performed to identify the position of the lesion, the intraocular pressure (IOP) measured with a Tono-Pen XL instrument (Medtronic Solan, Jacksonville, FL, USA) and cup/disc ratio by an indirect ophthalmoscopy, and refraction was tested using two instillations of cyclopentolate 0.5% with phenylephrine 2.5%, with an interval of 10 min. Visual acuity was measured by monocular and binocular fixation test; Teller test was impossible owing to the young age of the patients. Treatment for amblyopia was initiated in patients over 5 months old. A dermatologic examination was followed by radiological evaluation with computed tomography (CT) or magnetic resonance imaging (MRI) with contrast material to delineate the full periorbital and orbital extent of the lesion. Only infants in whom a paediatric dermatologist and two paediatric ophthalmologists confirmed the presence of resistant, extensive combined periorbital, and orbital capillary haemangioma, including lesion pressure on the globe, significant refractive anisometropia between the involved and non-involved eye, proptosis, and partial blockage of the visual axis, were considered eligible for combined treatment. Infants with other ocular and neurological problems, as well as other periorbital vascular lesions, such as port-wine haemangioma, were excluded.
Treatment
All patients had undergone the first-phase treatment with intralesional corticosteroid injection(s) of a 1-ml (50 : 50) mixture of betamethasone sodium phosphate (Celestone Chronodose, Schering-Plough Corp., Kenilworth, NJ, USA), 6 mg/ml, and triamcinolone acetonide (Kenalog, Bristol–Myers Squibb SRL, Anagni, Italy), 40 mg/ml. Dermatological treatment with oral betamethasone (Betnesol, Devries & Co. Ltd, Tel Aviv, Israel), 0.5 mg/kg/day, was initiated together with the periorbital corticosteroid injections in all patients. The interval between the corticosteroid injections was 4–6 weeks. When there was no significant ocular improvement (only in a minority of patients), or the vascular lesions recurred after 1–3 sessions (depending on the severity of the clinical findings), or systemic complications were observed, the second-phase treatment was initiated to overcome this refractory presentation. This consisted of posterior sub-Tenon's infusion of a mixture (50 : 50) of betamethasone sodium phosphate (Celestone Chronodose), 6 mg/ml, and triamcinolone acetonide (Kenalog), 40 mg/cc, to a volume of 1 cc per infusion, administered close to the orbital vascular lesion, combined with a repeated intralesion injection, as in the first phase, without oral steroids. Recurrent post-treatment CT or MRI scans were performed to compare and evaluate the effectiveness of this modality.
Technique
A 3–4-mm incision of the conjunctiva and sub-Tenon's capsule was made in the specific quadrant, 8–10 mm from the limbus. A blunt-tipped cannula was inserted through the incision, and the tip was positioned close to the posterior part of the lesion. Up to 1 cc of corticosteroid mixture was very slowly injected into the posterior sub-Tenon's space. The incision was closed with two Vicryl 8/0 sutures (Polyglactin, Johnson and Johnson, St Stevens-Wolnue, Belgium). An intralesional injection of corticosteroids was then administered (in the same session). All treatments were administered by the same surgeon (MS). IOP and funduscopic parameters (to exclude vascular compromise) were measured before and immediately after treatment, and during the follow-up period up to 4 months after receiving steroid therapy.
Evaluation
The anatomical, IOP, and refractive responses to treatment were evaluated longitudinally, from the first day after injection, and followed once monthly for the first year of treatment. Criteria for successful outcome were significant reduction in lesion size, free visual axis, and improvement in four refractive parameters—spherical and cylinder power, axis of astigmatism, and spherical equivalent (SE). The early and late ocular and systemic side effects of the corticosteroid treatments were also carefully evaluated with the paediatric dermatologist. IOP was measured at 1, 3, and 4 months after treatment. Parental satisfaction with regard to treatment, medical staff, and their expectation was measured on a scale of 0 (total dissatisfaction) to 10 (maximal satisfaction).
Study protocol
For this study, the results of the combined method were retrieved from the medical files and analysed retrospectively. The study was approved by the Institutional Review Board of Rabin Medical Centre, Beilinson Hospital, and approval was confirmed by the directorship of Schneider Children's Medical Centre of Israel. Written consent for the corticosteroid injections was obtained from the parents of each patient.
Statistical analysis
The non-parametric Mann–Whitney test was used to compare patient age at diagnosis and at first treatment. Paired t-test was used to determine the significance of differences in ocular proptosis and visual axis before and after treatment, and Wilcoxon-matched pairs signed-rank test was used to analyse the changes in refractive parameters. A P-value of ⩽0.05 was considered significant. All analyses were performed with the Statistical Package for the Social Sciences (SPSS; Professional Statistics release 11.5/2003, Chicago, IL, USA).
Results
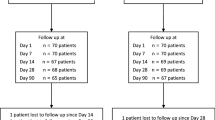
The group of refractory capillary haemangioma included two male and five female infants of mean age 3.5±1.9 months at diagnosis and 4.2±1.9 months at the first treatment (Table 1). All seven infants initially underwent periorbital intralesional corticosteroid injections (1–3 times) combined with systemic oral corticosteroids. Six of them later received the combined corticosteroid treatments because of resistant disease (two patients/two injections and four patients/one injection), and one received only a posterior sub-Tenon's corticosteroid injection in the second phase. In two cases, the second combined treatment was delivered because of an absence of anatomical improvement at 4–5 weeks after the first treatment.
The anatomical evaluation showed that 5/7 infants (71.4%) had proptosis before treatment, and all were completely symptom-free after. A free optical axis was noted in one patient (14.3%) before treatment and in all patients (100%) after treatment (Figure 1a–d). Mean time from the day of injection to the achievement of significant anatomical and functional results was 96.43±58.3 days. This was the mean total period of our seven patients, including two patients who received double injections.
(a) Before the combined steroid infusion. Significant proptosis and upper lid deformation with diffuse capillary haemangioma of right eye. (b) Two months after the first combined steroid injection. A significant reduction of proptosis with free visual axis is seen. (c) Before the combined corticosteroid infusion. Proptosis of upper lid and capillary haemangioma of right eye. (d) Four weeks after the second combined steroid infusion; the reduced proptosis and vascular lesion size with free optical axis are shown.
Evaluation of the refraction parameters (Table 2) showed a reduction of 22.7% in spherical power after treatment, which was close to our statistical criterion of significance (P=0.06) and a reduction of 53.8% in cylinder power (P=0.46). There was almost no change in cylinder axis (P=0.65; Table 2). Mean SE decreased in 33.7% of patients, but the difference was not statistically significant (P=0.09).
Mean IOP (measured by the Tono-Pen XL instrument) before and immediately after combined treatment was 12–15 and 15–18 mmHg, respectively. Additionally, mean IOP during the follow-up period, up to 4 months after treatment, was within the normal limits on repeated measurements for each patient and ranged between 13–17 mmHg. Cup/disk ratio remained unchanged during the follow-up period in all patients.
Mean score of parental satisfaction with the clinical improvement was 9/10. The main concerns for most parents were cosmetic outcome, vision of the involved eye, and the difference of the extent of the lesion before and after treatment and during the follow-up period. The two repeated IOP results taken during the follow-up period were within the normal limits.
Mean duration of follow-up after treatment was 17±5.54 months. There was no anatomical or refractive deterioration in any of the infants during follow-up, and no early or late ocular complications were observed.
Discussion
This study shows that in infants with refractory massive periorbital and orbital haemangiomas, a combination of local corticosteroid treatment to the posterior sub-Tenon's space13 in the orbital region and directly to the lesion in the periorbital area is associated with significant improvement, both anatomically and functionally without ocular complications.
In most cases, capillary haemangioma regresses spontaneously, and its management initially consists of observation only, to ensure timely diagnosis of significant refractive error. Active treatment to reduce tumour size is indicated only in the event of occlusion of the visual axis, compression of the eye globe (which induces astigmatism and amblyopia), progressive proptosis of the eyeball with evidence of optic nerve compression, or strabismus. Nowadays, local or systemic corticocorticosteroids,14, 15 or both,12 are delivered either directly to the lesion or to the sub-Tenon's space, separately.
Ranchod et al,12 in a large review of corticosteroid treatment of periorbital haemangioma, concluded that objective data are mandatory for future practice and for establishing the safety of oral, topical, and intralesional steroids in children with periorbital haemangioma requiring ophthalmological intervention.
The recommended dosage of intralesional corticosteroids is 1 ml of a 50 : 50 mixture of Kenalog 40 mg/ml and Celestone 6 mg/ml;16 the dosage of oral corticosteroids is 1.5–5 mg/kg/day prednisolone.17 The optimal corticosteroid treatment varies according to the location and extension of the haemangioma. Tumour regression should be noted within 2–4 weeks; further injections may be necessary, as determined by the clinician.
The mechanism underlying the beneficial effect of corticosteroids on haemangiomas is unknown.18 Stuttgen19 attributed the effect to vasoconstriction, and others suggested that the corticosteroids increase the sensitivity of the arterioles to other physiologically occurring vasoconstrictive agents.20 Folkman21 found that certain corticosteroids inhibit haemangiogenesis in the presence of a fragment of heparin. In this study, we infused corticosteroids periorbitally, deep into the posterior sub-Tenon's space to achieve a maximal effect proximal to the orbital lesion combined with the periorbital intralesion injection. The rationale of our treatment modality was to treat intensively the whole pathway of this extensive vascular lesion, from the deep and invisible intraorbital up to the superficial visible periorbital section. We assume that this practice accounted for most of the improvement, as previous treatment with intralesional injection combined with systemic corticosteroids failed to induce significant anatomical or functional changes in any of our patients. Of the seven patients, six received the combined corticosteroid injection, and in the remaining patient (14.3%), the second phase consisted only of posterior sub-Tenon's injection, and it also yielded improved results.
Anatomically, no patient demonstrated ocular proptosis or visual axis obstruction after treatment. Functionally, the improvement in refractive results involved mainly the spherical power (P=0.06). The exact mechanism for this phenomenon remains obscure. We assume that the shrinkage of the vascular lesion changes the orbital depth and width relative to the globe, and therefore removes the ocular distortion and the blockage of normal globe development and elongation. It is noteworthy that these changes appeared postoperatively, only in the involved eyes. Therefore, the refractions in the involved and non-involved eye were very similar during the follow-up. The decrease in SE and astigmatic power indicated an overall improvement, but these differences were not statistically significant, perhaps because of the small number of patients. Further follow-up of these patients will be conducted to prove that this treatment prevented amblyopia in the involved eye.
The involvement of the parents in the treatment decision and our strong team support may have contributed to the high satisfaction scores.
Ophthalmologists and paediatricians need to follow treated infants for the side effects of corticosteroids. Potential early complications (up to 4 months after treatment) include facial acne eruption, moon face, nocturnal irritability, increased appetite, increased IOP, and hypertension; potential late complications (18–24 months after treatment) also include cataract and increased IOP. Furthermore, the infusion of corticosteroids deep into the posterior sub-Tenon's space may be associated with elevated IOP, vascular obstruction, and haemorrhages caused by the infusion itself, or optic nerve compression caused by infusion of the medications into a very crowded orbit, or glaucoma caused by the medication itself. None of these side effects occurred in our patients, at least partly because the medication was infused slowly, and only a volume of 1 ml was injected into the sub-Tenon's space in a single session. In addition, IOP measurements and funduscopy were performed before and immediately after each corticosteroid injection, and all were within the normal limits. IOP and cup/disk ratio measurements taken during the follow-up period were also normal.
Besides the novel combined treatment protocol described here, our study differs from previous reports in the detailed anatomic and functional refractive evaluations before and after treatment, and the long clinical follow-up, including IOP and cup/disc ratio measurements, which made it possible to evaluate the stability of the results.
Conclusion
We present an improved treatment modality of combined local administration of a corticosteroid mixture in patients with refractory periorbital and orbital haemangioma where the initial therapy has been unsuccessful. This technique places the medication in proximity to the orbital haemangioma and directly into the periorbital lesion, along the pathway of this vascular lesion, which yields a maximal beneficial anatomic and functional effect.
References
Jacobs AH, Walton PG . The incidence of birthmarks in the neonate. Pediatrics 1976; 58: 218–222.
Amir J, Metzker A, Krikler R, Reisner SH . Strawberry hemangioma in preterm infants. Pediatr Dermatol 1986; 3: 331–332.
Finn MC, Glowacki J, Muliken JB . Congenital vascular lesions: clinical application of a new classification. J Pediatr Surg 1983; 18: 894–900.
Mulliken JB, Glowacki J . Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg 1982; 70: 412–420.
Mulliken J, Young AE . Vascular birthmarks: Hemangiomas and malformations. WB Saunders: Philadelphia, 1988, pp 41–46.
Folkman J, Haudenschild C . Angiogenesis in vitro. Nature 1980; 288: 551–556.
Baroni C, Scelsi R . On the relationship of mast cells to various bone, cartilaginous and synovial tumours. Pathol Eur 1967; 2: 382–393.
Kessler DA, Langer RS, Pless NA, Folkman J . Mast cells and tumor angiogenesis. Int J Cancer 1976; 18: 703–709.
Azizkhan RG, Azizkhan JC, Zetter BR, Folkman J . Mast cell heparin stimulates migration of capillary endothelial cells in vitro. J Exp Med 1980; 152: 931–944.
Flanagan J . Vascular problems of the orbit. Ophthalmology 1979; 86: 896–913.
Esterly N . Cutaneous hemangiomas, vascular stains and malformations, and associated syndromes. Curr Probl Pediatr 1996; 26: 3–39.
Coats DK, O’Neil JW, D’Elia VJ, Brady-McCreery KM, Paysse EA . Sub-Tenon's infusion of corticosteroids for treatment of orbital hemangiomas. Ophthalmology 2003; 110: 1255–1259.
Ranchod TM, Frieden IJ, Fredrick DR . Corticosteroid treatment of periorbital haemangioma of infancy: a review of the evidence. Br J Ophthalmol 2005; 89: 1134–1138.
Kushner BJ . Intralesional corticosteroid injection for infantile adnexal hemangioma. Am J Ophthalmol 1982; 92: 496–506.
Egbert JE, Schwartz GS, Walsh AW . Diagnosis and treatment of an ophthalmic artery occlusion during an intralesional injection of corticosteroid into an eyelid capillary hemangioma. Am J Ophthalmol 1996; 121: 638–642.
Ceisler EY, Santos L, Blei F . Periocular hemangiomas: what every physician should know. Pediatr Dermatol 2004; 21: 1–9.
Lyons CJ, Rootman J . Duane's clinical ophthalmology. In: Tasman W, Jaeger EA (eds). Vascular disease. Elsevier Saunders:New York, 2005, pp 385–396.
Sadan N, Wolach B . Treatment of hemangiomas of infants with high dose of prednisone. J Pediatr 1996; 128: 141–146.
Stuttgen G . Vasoconstriction in response to corticosteroids observed in human lips. Dermatologica 1976; 152 (Suppl 1): 91–100.
Droplet BA, Easterly NB, Frieden IJ . Hemangiomas in children. N Engl J Med 1999; 341: 2018–2019. (letter).
Folkman Y . Toward a new understanding of vascular proliferative disease in children. Pediatrics 1984; 74: 850–856.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no financial interest in the study and received no commercial support
Rights and permissions
About this article
Cite this article
Friling, R., Axer-Siegel, R., Ben-Amitai, D. et al. Intralesional and sub-Tenon's infusion of corticosteroids for treatment of refractory periorbital and orbital capillary haemangioma. Eye 23, 1302–1307 (2009). https://doi.org/10.1038/eye.2008.300
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2008.300