Abstract
Purpose
To assess the long-term effects of fractionated stereotactic radiotherapy (fSRT) for the treatment of (presumed) benign intraorbital tumours on visual acuity, visual fields, globe and eyelid position, and complications including radiation retinopathy and deviations of retinal nerve fibre layer (RNFL) on OCT.
Methods
Multi-centre retrospective follow-up study of a consecutive series of 25 patients treated in the Rotterdam Orbital Center (collaboration between Erasmus Medical Center and Rotterdam Eye Hospital) between 2002 and 2018. Data on the dose of fSRT, visual acuity, Humphrey field analyser (HFA) perimetry, globe and eyelid position were obtained from the medical records.
Results
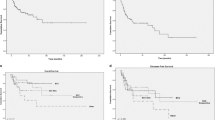
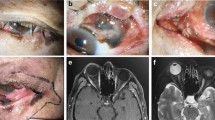
In this retrospective consecutive series of 25 patients with a median follow-up of 104 months (range 48–215 months), 80.0% of the patients had presumed optic nerve sheath meningioma and 20.0 % presumed cavernous haemangioma with signs suggestive of recent growth. In most patients, a better visual acuity and RNFL thickness were observed after stereotactic radiotherapy. Improvement of the visual field defects was observed after treatment, with a mean deviation of −14.98 dB (12.9 SD) before treatment versus −4.56 dB (10.8 SD) after treatment, respectively. Significant, but small changes in exophthalmometry values were observed with a mean of 14.92 mm (7.9 SD) versus 13.79 mm (7.3 SD) after treatment, respectively. Only 3 patients (15.0%) developed radiation retinopathy after stereotactic radiotherapy. All patients with radiation retinopathy had presumed optic nerve sheath meningioma.
Conclusions
Based on our results, fSRT is an effective treatment modality for this subset of orbital tumours with few complications and good long-term visual and cosmetic outcomes. FSRT is non-invasive and safer than surgery for lesions in the posterior orbit or around the optic nerve.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Terrier LM, Bernard F, Fournier HD, Morandi X, Velut S, Henaux PL, et al. Spheno-orbital meningiomas surgery: multicenter management study for complex extensive tumors. World Neurosurg. 2018;112:e145–e56.
Scarone P, Leclerq D, Heran F, Robert G. Long-term results with exophthalmos in a surgical series of 30 sphenoorbital meningiomas. Clin Artic J Neurosurg. 2009;111:1069–77.
Nagahama A, Goto T, Nagm A, Tanoue Y, Watanabe Y, Arima H, et al. Spheno-orbital meningioma: surgical outcomes and management of recurrence. World Neurosurg. 2019;126:e679–e87.
Kondziolka D, Mathieu D, Lunsford LD, Martin JJ, Madhok R, Niranjan A, et al. Radiosurgery as definitive management of intracranial meningiomas. Neurosurgery. 2008;62:53–8.
Guyer DR, Miller NR, Long DM, Allen GS. Visual function following optic canal decompression via craniotomy. J Neurosurg. 1985;62:631–8.
Stafford SL, Pollock BE, Foote RL, Link MJ, Gorman DA, Schomberg PJ, et al. Meningioma radiosurgery: tumor control, outcomes, and complications among 190 consecutive patients. Neurosurgery. 2001;49:1029–37.
Khan AA, Niranjan A, Kano H, Kondziolka D, Flickinger JC, Lunsford LD. Stereotactic radiosurgery for cavernous sinus or orbital hemangiomas. Neurosurgery. 2009;65:914–8.
Thompson TP, Lunsford LD, Flickinger JC. Radiosurgery for hemangiomas of the cavernous sinus and orbit: technical case report. Neurosurgery. 2000;47:778–83.
Liu JK, Forman S, Hershewe GL, Moorthy CR, Benzil DL. Optic nerve sheath meningiomas: visual improvement after stereotactic radiotherapy. Neurosurgery. 2002;50:950–5.
Klingenstein A, Mueller-Lisse GU, Haug AR, Garip-Kuebler A, Miller CV, Hintschich CR. Combined positron emission tomography/computed tomography (PET/CT) for imaging of orbital tumours and tumours extending into the orbit. Br J Ophthalmol. 2016;100:1403–8.
Fawaz SA, Ezzat WF, Salman MI. Sensitivity and specificity of computed tomography and magnetic resonance imaging in the diagnosis of isolated sphenoid sinus diseases. Laryngoscope. 2011;121:1584–9.
Rokohl AC, Koch KR, Kabbasch C, Kreppel M, Luers JC, Grau S, et al. [Importance of interdisciplinary collaboration for optimal treatment of orbital tumors] Bedeutung der interdisziplinaren Zusammenarbeit fur eine optimale Behandlung orbitaler Tumoren. HNO. 2019;67:528–33.
Rose GE. The “devil’s touch”; visual loss and orbital surgery. A synopsis of the Mustarde Lecture, 2006. Orbit. 2007;26:147–58.
Kiratli H, Yildiz S, Soylemezoglu F. Neurofibromatosis type 2: optic nerve sheath meningioma in one orbit, intramuscular schwannoma in the other. Orbit. 2008;27:451–4.
Moon CH, Hwang SC, Ohn YH, Park TK. The time course of visual field recovery and changes of retinal ganglion cells after optic chiasmal decompression. Invest Ophthalmol Vis Sci. 2011;52:7966–73.
Danesh-Meyer HV, Carroll SC, Foroozan R, Savino PJ, Fan J, Jiang Y, et al. Relationship between retinal nerve fiber layer and visual field sensitivity as measured by optical coherence tomography in chiasmal compression. Invest Ophthalmol Vis Sci. 2006;47:4827–35.
Narayan S, Cornblath WT, Sandler HM, Elner V, Hayman JA. Preliminary visual outcomes after three-dimensional conformal radiation therapy for optic nerve sheath meningioma. Int J Radiat Oncol Biol Phys. 2003;56:537–43.
Maaijwee K, Nowak PJ, van den Bosch WA, Paridaens D. Fractionated stereotactic radiotherapy for cavernous haemangioma of the orbital apex. Acta Ophthalmol. 2012;90:e655–7.
Rootman DB, Rootman J, Gregory S, Feldman KA, Ma R. Stereotactic fractionated radiotherapy for cavernous venous malformations (hemangioma) of the orbit. Ophthalmic Plast Reconstr Surg. 2012;28:96–102.
Subramanian PS, Bressler NM, Miller NR. Radiation retinopathy after fractionated stereotactic radiotherapy for optic nerve sheath meningioma. Ophthalmology. 2004;111:565–7.
Krishnan R, Kumar I, Kyle G, John Husband D. Radiation retinopathy after fractionated stereotactic conformal radiotherapy for primary intraorbital optic nerve sheath meningioma. J Neuroophthalmol. 2007;27:143–4.
Klink DF, Miller NR, Williams J. Preservation of residual vision 2 years after stereotactic radiosurgery for a presumed optic nerve sheath meningioma. J Neuroophthalmol. 1998;18:117–20.
Ratnayake G, Oh T, Mehta R, Hardy T, Woodford K, Haward R, et al. Long-term treatment outcomes of patients with primary optic nerve sheath meningioma treated with stereotactic radiotherapy. J Clin Neurosci. 2019;68:162–7.
Wolf A, Naylor K, Tam M, Habibi A, Novotny J, Liscak R, et al. Risk of radiation-associated intracranial malignancy after stereotactic radiosurgery: a retrospective, multicentre, cohort study. Lancet Oncol. 2019;20:159–64.
Author information
Authors and Affiliations
Contributions
OG and DP designed the study. OG and ROBK performed the analyses. OG and SED wrote the manuscript. ROBK, SED, CvR, CS and DP advised and reviewed the manuscript. All authors confirm that neither this manuscript nor any part of it has been published and is not under consideration for publication elsewhere.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gishti, O., de Keizer, R.O.B., Detiger, S.E. et al. Radiation optic neuropathy and retinopathy in patients with presumed benign intraorbital tumours treated with fractionated stereotactic radiotherapy. Eye 37, 2470–2474 (2023). https://doi.org/10.1038/s41433-022-02356-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02356-0