Abstract
Purpose
To examine the early differences in the thicknesses of the macula and retinal nerve fibre layer (RNFL) by Stratus optical coherence tomography in patients with diabetes mellitus.
Methods
Thirty-one normal participants without any optic nerve and retinal diseases (control), 45 diabetic patients without diabetic retinopathy (NDR), and 24 diabetic patients with preproliferative diabetic retinopathy (PPDR), who did not have clinically significant macular oedema, were used for the macular thickness measurements. Thirty control participants, 45 patients classified as NDR, and 22 patients classified as PPDR were used for the RNFL thickness measurements.
Results
In patients with NDR, macula was significantly thinner than that of control eyes. In patients with PPDR, the mean RNFL thickness was significantly thinner but the macula was thicker than that of control eyes. In women with NDR, the macula was significantly thinner than that of men with NDR and that of normal women. In men with PPDR, the RNFL thickness was significantly thinner than that of the control eyes.
Conclusions
At the early stage of diabetic retinopathy, the maculas and RNFL thicknesses are altered. The macular and RNFL thicknesses are different in men and women.
Similar content being viewed by others
Introduction
Diabetic retinopathy (DR) is one of the major complications in patients with diabetes mellitus (DM) that can lead to blindness. However, the precise mechanisms leading to the onset and the progression of the retinopathy remain unclear.1, 2, 3 Recent studies have shown that not only vascular abnormalities but also neuronal abnormalities, including retinal ganglion cell (RGC) death, accompany the pathogenic changes at the early stage of DR.4, 5, 6, 7 Thus, these two factors should be considered in investigating the pathogenesis of DR,1, 2, 3 and examination of these abnormalities at the early stage of DR may provide clues to help determine the mechanisms that lead to DR.
The Stratus optical coherence tomographic instrument (OCT Model 3000, Carl Zeiss, Meditec, CA, USA) is a third generation model that can provide B-scan images of the retina with a resolution of 8–10 μm. The thickness of the macular area and the retinal nerve fibre layer (RNFL) can be measured reliably by the installed software,8, 9 and these high-resolution images help clinicians follow patients with DR and glaucoma reliably and accurately.10, 11
Earlier studies have shown that the macular area is thicker and the RNFL is thinner in diabetic patients without diabetic retinopathy (NDR) and in those with preproliferative diabetic retinopathy (PPDR) compared to non-diabetic patients.12, 13, 14 It has been suggested that a leakage of sera because of an increase in the vascular permeability may be the cause of the thickened retina.12, 13, 14
At the early stage of DR, the RNFL thickness may be reduced because of the RGC death and axonal degeneration.1, 2, 3, 4, 5, 6, 7, 14 But this does not explain why the macular area is thicker. The reduced RNFL thickness is not detected in the macular thickness at the early stage of DR because an increased vascular permeability masks the effects of neuronal degeneration.
We hypothesized that neuronal abnormalities precede vascular abnormalities and also that the reduced macular thickness in the early stage of DM is gradually replaced by an increased thickness because of the increased vascular permeability caused by diabetes. To test this hypothesis, we measured the thicknesses of macula and RNFL in the peripapillary areas by Stratus OCT in diabetic patients at the early stage of DR. We also compared the differences of the OCT findings between men and women. We show that macula is thicker and RNFL is thinner at the early stages of DR, and these changes may be related to both the neuronal and vascular abnormalities.
Patients and methods
Participants
This research protocol was approved by the Institutional Review Board of the Sannoh Hospital, and all procedures conformed to the tenets of the World Medical Association Declaration of Helsinki. Outpatients who had visited our clinic from January 2007 to March 2007 were studied. The macular thickness was measured in 31 normal participants (control; 19 men and 12 women), 45 diabetic patients classified as NDR (25 men and 20 women), and 24 diabetic patients (17 men and 7 women) with PPDR but without macular oedema by fundus examinations. Patients with severe NPDR and very severe NPDR were excluded from the PPDR group.
The thickness of the RNFL was measured in 30 control participants (16 men and 14 women), 45 diabetic patients classified as NDR (25 men and 20 women), and 22 diabetic patients classified as PPDR (16 men and 6 women).
The mean ages of the control, NDR, and PPDR groups were 60.0±12.8, 61.6±11.2, and 65.6±8.8 years, respectively. The differences in the mean ages were not significant among the three groups.
After an explanation of the procedures to be performed, an informed consent was obtained from all the patients. All participants had routine ophthalmological examinations. Participants who had a best-corrected visual acuity <20/32 on the Early Treatment Diabetic Retinopathy Study scale, high myopia >−8.0 D, history of DM or hypertension, previous ocular surgery, ocular hypertension, optic anomaly (large or small disc), and history of retinal or optic nerve diseases were excluded from the control groups. The clinical data and demographics of the diabetic patients at the NDR and PPDR stages are shown in the Table 1. The HbA1c level, determined within three month of the OCT measurements, was used in this prospective study. We certified that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research.
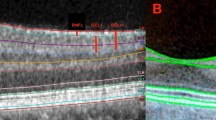
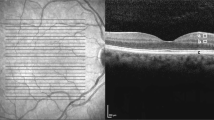
OCT measurements
OCT scans were performed through a dilated pupil while monitoring the video image of the central retina. The programs for the fast macular thickness and the fast RNFL thickness measurements were used. The fast macular thickness protocol consists of six radial scans of 6 mm length through the centre of the fovea. The retinal thickness was defined as the distance between the vitreoretinal interface and the anterior surface of the retinal pigment epithelium along each A-scan. From the retinal map analysis protocol, five sectors in the inner rings with a diameter of 3 mm, the centre, superior, nasal, temporal, and inferior sectors, were analysed. The thickness of the centre sector was defined as the average in the central 1 mm diameter ring. The outer sectors between 3 and 6 mm diameter were excluded because of lower reliability of the measurements than that of the inner sectors.
The fast RNFL thickness protocol consisted of three circular peripapillary scans of 3.4 mm diameter centred on the optic disc. Each scans consisted of 256 measurements along the circumference. The average overall peripapillary thickness and the thickness of the superior and inferior quadrants were analysed. The RNFL thickness was defined as the number of pixels between the highly reflective layer at the vitreous surface and the points on each scan whose reflectivity exceeded a specific threshold. The RNFL thickness was automatically calculated with the installed software. Poor quality scans with signal strength less than 5, error messages, and poor fixation during the scans were rejected. A total of three scans were rejected from the RNFL study due to poor quality scans.
Statistical analyses
The left eyes of all patients who fulfilled the inclusion criteria were used for statistical analyses.15 If the left eyes did not fulfil the inclusion criteria, the right eyes were used for statistical analyses. All data are expressed as the mean±standard deviation (SD), and the Stat View 5.0 program was used for all statistical analyses. Parametric comparisons were used for the analysis of variance (ANOVA). If ANOVA was significant, the significances of individual differences were evaluated by combining them with multiple tests: Fisher's PLSD, Student–Newman–Keuls, and Games–Howell multiple comparison tests. P<0.05 and P<0.01 were considered significant or highly significant. The correlations between OCT measurements and clinical parameters were analysed by Pearson's coefficient of correlation. A P<0.05 was considered significant.
Results
Macular thickness in diabetic patients
In the NDR group, the mean macular thickness at the centre sector was significantly thinner than that in the control group (Fisher's PLSD; P=0. 0229 and Student–Newman–Keuls; Table 2). In the PPDR group, the macular thickness of the centre sector was significantly thicker than that of the NDR group (Fisher's PLSD; P=0.0006, Games–Howell and Student–Newman–Keuls; Table 2). The coefficient of correlation between the duration of the DM and the macular thickness of the centre sector was significant for both diabetic groups (r=0.303, P=0.0110; n=69). Thus, the central macula was thicker in eyes with longer duration of DM.
RNFL thickness in diabetic patients
In the NDR group, the mean, superior, and inferior RNFL thicknesses were thinner than the corresponding sectors of the control group, but the differences were not significant. In the PPDR group, the mean RNFL and the superior and inferior peripapillary sectors were significantly thinner than the corresponding sectors of the control group (Fisher's PLSD; P=0.0016, 0.0134, 0.0017, respectively, Games–Howell, and Student–Newman–Keuls; Table 3). In the PPDR group, the mean RNFL and the superior and inferior sectors were significantly thinner than the corresponding sectors of the NDR group (Fisher's PLSD; P=0.0202, 0.0294, 0.0422, respectively and Student–Newman–Keuls; Table 3). The coefficient of correlation between the duration of DM and the mean RNFL thickness was weak but significant for both diabetic groups (r=−0.2378; P=0.0174; n=67). Thus, the RNFL thickness was thinner in eyes with longer duration of DM.
Comparison of differences of macular and RNFL thicknesses between men and women
In normal participants, the differences of the macular and RNFL thicknesses between men and women were not significant. In the women with NDR, however, the macular thicknesses of all sectors (centre, superior, nasal, temporal, inferior) were significantly thinner than those of men with NDR (Fisher's PLSD; P=0.0085, 0.0056, 0.0015, 0.0042, 0.0303, respectively, Games–Howell and Student–Newman–Keuls; Table 4). In addition, in women with NDR the nasal and temporal sectors of the macular thickness were significantly thinner than that of the normal women (Fisher's PLSD; P=0.0341, 0.0374, respectively and Games–Howell). Thus in the early stages, the macular thickness in women with NDR is more sensitive to the effects of diabetes than in men.
The differences in the RNFL thickness between men and women in the normal, NDR, and PPDR groups were not significant. In men with PPDR, however, the mean, superior, and inferior RNFL thicknesses were significantly thinner than those of the normal men (Fisher's PLSD; P=0.0099, 0.0411, 0.0237, respectively, Games–Howell and Student–Newman–Keuls). Thus, the RNFL thickness in men is more sensitive to the effects of diabetes than women.
Discussion
Although the resolution of Stratus OCT is improved and is better than the previous models of OCT, the fast macular and RNFL thickness protocols are known to reduce the resolution of OCT scans. The resolution of the differences in the macular and RNFL thicknesses in the different groups was around 10 μm, which is at the margin of errors for the scanning protocols. Thus, the technologies of Stratus OCT may be limited in their ability to examine the clinical significance of data such as those collected in our study. Although significant differences were detected in macular and RNFL thicknesses in out patients, other more sensitive techniques such as 3D OCT should be used to determine whether similar differences can be found.
Our OCT findings demonstrated that the macula in the NDR group was significantly thinner than that of the control group. These results are not consistent with the past reports.12, 13, 14 One possible reason for this discrepancy may be the shorter duration of the DM in our NDR group than in the other studies, eg, 4.8±4.4 vs 7.9±7.3 years in the data of Sugimoto (Table 5).14
Our findings showed that both macular and RNFL thicknesses were significantly correlated with the duration of DM. In addition, our findings showed that the macular thickness gradually increased with the duration of DM probably because of an increase in vascular permeability in the diabetic retinas.12, 13, 14 Because of the short duration of DM, early reduction of macular thickness due to neuronal degeneration was not masked by the increase in macular thickness associated with vascular leakage.
Several studies, including ours, showed that retinal neuronal abnormalities are present at the early stage of diabetes.1, 2, 3, 4, 5, 6, 7 The neuronal abnormalities may explain the thinner macular thickness if these developed before the increased vascular permeability. Neuronal abnormalities including RGC death and axonal degeneration should increase with an increase in the duration of DM, and in turn, reduce the RNFL thickness. Our findings that macula was thinner at the NDR stage but thicker in the PPDR stage would suggest that the neuronal abnormalities may precede the vascular abnormalities.
However, there was no statistical correlation between macular and RNFL thicknesses in our data. We could not determine whether the resolution of macular thickness in eyes with NDR was related to RNFL thickness reduction in the early stage diabetes. It seems that alteration of RNFL thickness should be discussed independently of changes in macular thickness. Further studies are needed to determine the cause of the reduction in macular and RNFL thicknesses at the early stage of diabetic retinas.
Wong et al reported that the macular thickness in men was significantly thicker than that of women.16 Therefore, we compared the differences of the macular and RNFL thicknesses between men and women. In the normal participants, the macula was thinner in women than in men but the difference was not significant. In women with NDR, all sectors of the macula were significantly thinner than those of men with NDR. These results indicate that the early changes of the macular thickness in women developed earlier than that in men. However, in men with PPDR, the mean, superior, and inferior RNFL were significantly thinner than those of normal men. These results indicate that the damage of the RNFL induced by diabetes in men may be more sensitive and progress faster than that in women. Further studies are needed to elucidate the effect of the differences of gender in the early changes of diabetic retinas.
As this was a prospective study, all patients who met the criteria were included. Thus, there were gender imbalances among each group. For example, the normal group had 61% men but the PPDR group had 71% men. Because the maculas of men tend to be thicker than that of women, the gender imbalance may make the PPDR maculas thicker not because of the severity of the retinopathy, but because of the gender imbalance. Likewise, the NDR group had 56% men, which would tend to make the maculas of this group thinner than that of normal group because of the higher percentage of women in the group. However, we could not detect any significant differences between men and women in the normal group and the PPDR group. Only in NDR group there was a significant difference between men and women. Furthermore, thicker maculas in the PPDR group than that in the normal group is consistent with the earlier reports (Table 5).12, 13, 14 Thus, the gender imbalance may not be so large as to negate the effects of the diabetes on the retina. Again, our results indicate that in women with NDR, the macular thickness is thinner and may be more sensitive and progress faster than in men with NDR.
In the PPDR group, an increase in serous leakage probably led to the swelling of the retina. Although our results that the maculas in the PPDR group were thicker than the normal group maculas is consistent with the past report (Table 5),12, 13, 14 our data should be considered tentative because this was a cross-sectional study. Further studies are needed to determine the effect of diabetes on macular and RNFL thicknesses in diabetic patients.
In conclusion, we have detected changes in the macular and the RNFL thicknesses by the Stratus OCT in patients with early stage DR. These changes may be related to both neuronal and vascular abnormalities that occur in the early stage of diabetic retinas. The onset and the progression of the early changes of DR are significantly different between men and women. Further studies are needed to determine the mechanism for the onset and development of the pathogenesis of DR.
References
Oshitari T . Non-viral gene therapy for diabetic retinopathy. Drug Dev Res 2006; 67: 835–841.
Oshitari T, Roy S . Common therapeutic strategies for diabetic retinopathy and glaucoma. Curr Drug Ther 2007; 2: 224–232.
Oshitari T, Hata N, Yamamoto S . Endoplasmic reticulum stress and diabetic retinopathy. Vasc Health Risk Manag 2008; 4: 115–122.
Barber AJ, Lieth E, Khin SA, Antonetti DA, Buchanan AG, Gardner TW . Neural apoptosis in the retina during experimental and human diabetes. Early onset and effect of insulin. J Clin Invest 1998; 102: 783–791.
Takano M, Sango K, Horie H, Sato M, Iijima Y, Ohno S et al. Diabetes alters neurite regeneration from mouse retinal explants in culture. Neurosci Lett 1999; 275: 175–178.
Asnaghi V, Gerhardinger C, Hoehn T, Adeboje A, Lorenzi M . A role for the polyol pathway in the early neuroretinal apoptosis and glial changes induced by diabetes in the rat. Diabetes 2003; 52: 506–511.
Oshitari T, Roy S . Diabetes: a potential enhancer of retinal injury in rat retinas. Neurosci Lett 2005; 390: 25–30.
Chan A, Duker JS, Ko TH, Fujimoto JG, Schuman JS . Normal macular thickness measurements in healthy eyes using Stratus optical coherence tomography. Arch Ophthalmol 2006; 124: 193–198.
Budenz DL, Anderson DR, Varma R, Schuman J, Cantor L, Savell J et al. Determinants of normal retinal nerve fiber layer thickness measured by stratus OCT. Ophthalmology 2007; 114: 1046–1052.
Pierre-Kahn V, Tadayoni R, Haouchine B, Massin P, Gaudric A . Comparison of optical coherence tomography models OCT1 and Stratus OCT for macular retinal thickness measurement. Br J Ophthalmol 2005; 89: 1581–1585.
Paunescu LA, Schuman JS, Price LL, Stark PC, Beaton S, Ishikawa H et al. Reproducibility of nerve fiber thickness, macular thickness, and optic nerve head measurements using StratusOCT. Invest Ophthalmol Vis Sci 2004; 45: 1716–1724.
Goebel W, Kretzchmar-Gross T . Retinal thickness in diabetic retinopathy: a study using optical coherence tomography (OCT). Retina 2002; 22: 759–767.
Lattanzio R, Brancato R, Pierro L, Bandello F, Iaccher B, Fiore T et al. Macular thickness measured by optical coherence tomography (OCT) in diabetic patients. Eur J Ophthalmol 2002; 12: 482–487.
Sugimoto M, Sasoh M, Ido M, Wakitani Y, Takahashi C, Uji Y . Detection of early diabetic change with optical coherence tomography in type 2 diabetes mellitus patients without retinopathy. Ophthalmologica 2005; 219: 379–385.
Oshitari T, Hanawa K, Adachi-Usami E . Macular and retinal nerve fiber layer thickness in Japanese measured by Stratus optical coherence tomography. Clin Ophthalmol 2007; 1: 133–140.
Wong AC, Chan CW, Hui SP . Relationship of gender, body mass index, and axial length with central retinal thickness using optical coherence tomography. Eye 2005; 19: 292–297.
Acknowledgements
This study is supported by the Grant-in-Aid from the Eye Research Foundation for the Aged in Japan. We thank Professor Duco Hamasaki for editing this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oshitari, T., Hanawa, K. & Adachi-Usami, E. Changes of macular and RNFL thicknesses measured by Stratus OCT in patients with early stage diabetes. Eye 23, 884–889 (2009). https://doi.org/10.1038/eye.2008.119
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2008.119
Keywords
This article is cited by
-
Assessment of area and structural irregularity of retinal layers in diabetic retinopathy using machine learning and image processing techniques
Scientific Reports (2024)
-
Alterations of outer retinal reflectivity in diabetic patients without clinically detectable retinopathy
Graefe's Archive for Clinical and Experimental Ophthalmology (2024)
-
Contrast sensitivity function under three light conditions in patients with type 1 diabetes mellitus without retinopathy: a cross-sectional, case–control study
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
Macular and peripapillary retinal nerve fiber layer thinning in eyes with prediabetes in the elderly population: OTASSHA study
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
Assessment of macular findings by OCT angiography in patients without clinical signs of diabetic retinopathy: radiomics features for early screening of diabetic retinopathy
BMC Ophthalmology (2022)