Abstract
Objective
To assess the course of neurodegeneration based on retinal layer thickness and integrity analysis in diabetic patients without retinopathy and to evaluate its association with inner retinal reflectivity.
Methods
This retrospective case–control study included 80 eyes of 80 patients with DM without retinopathy and 40 eyes of 40 healthy subjects with a follow-up of ≥1 year. SD-OCT was used for assessment of retinal reflectivity and macular layer thicknesses. Optical intensity ratios (OIRs) were defined as the mean OCT reflectivity of ganglion cell and inner nuclear layer to the mean reflectivity of RPE.
Results
After Bonferroni correction, thinning in pericentral, superior and nasal sectors in total retina, superior ganglion cell, pericentral and nasal inner plexiform, and superior inner retinal layers, as well as thickening in inferior and pericentral outer plexiform layer remained significant in the study group (p < 0.0125). Ganglion cell layer OIR significantly correlated with the changes in superior retina (r = 0.278, p = 0.013), central inner retina (r = 0.247, p = 0.027), and pericentral retinal thickness (r = 0.240, p = 0.032), and no eyes had disruption of retinal layers in the study group initially or finally.
Conclusion
Ganglion cell layer reflectivity significantly correlated with the amount of pericentral retinal thinning during the time course in the diabetic group, which was more prominent in the inner retinal layers.
Similar content being viewed by others
Introduction
Diabetic retinopathy (DR) is one of the major complications of diabetes mellitus (DM) and a leading cause of visual impairment in working-age population [1]. DR is primarily a vascular disease caused by the direct and indirect effects of hyperglycemia. It is characterized by the breakdown of the blood–retina barrier and increased vascular permeability secondary to the structural changes in the retinal vessel endothelium [2]. Since the underlying pathogenesis is considered vascular, current therapeutic approaches have mostly targeted vascular remodeling. However, recent studies suggest that a neurodegenerative process also takes place in DM [3,4,5].
Experimental and histopathological studies revealed structural changes in retina, including thinning, apoptosis of ganglion cells, and glial activation suggesting neurodegeneration in the course of DM [6,7,8]. Retinal functional evaluation by electroretinogram and micro-perimetry showed that functional impairment occurred before the onset of vascular lesions in diabetic patients [9,10,11].
By the introduction of SD-OCT (Spectral domain-optical coherence tomography), detailed visualization of the retinal structure has become possible. Previously, OCT was successfully used to monitor the retinal changes related to neurodegenerative diseases including Alzheimer’s Disease and Parkinson’s Disease [12, 13]. Several studies reported retinal thinning in diabetic patients without DR or non-proliferative DR compared to healthy controls [4, 5]. By using segmentation application, which allows the measurement of all individual retinal layers, this thinning was shown to affect mainly the inner retinal layers in many studies [14, 15].
The quantification of reflectivity of retinal layers on OCT has been a subject of interest with the attempt of refining new tools for better determination of prognostic factors. Alterations in retinal reflectivity on OCT were documented as a sign of ischemia or degeneration in various conditions [16,17,18,19]. Recently, it was reported that inner retinal layer reflectivity was significantly associated with visual prognosis at 1-year-control in eyes with central retinal vein occlusion [18].
There is very limited information about the longitudinal retinal changes in terms of neurodegeneration before vascular findings appear in diabetic patients. Recent few longitudinal studies showed that peripapillary retinal nerve fiber layer (RNFL) loss occurred in diabetic eyes even in the absence of DR progression, progressive loss of RNFL, as well as the ganglion cell /inner plexiform layer, appeared in eyes with no or minimal DR and it was reported that inner retinal layers were more profoundly affected during the time course [14, 15, 20, 21]. However, little is known about the associated factors related to retinal thinning and there is a lack of information on whether the retinal reflectivity might be a prognostic factor associated with the course of retinal thinning which is accepted as a finding of diabetic neurodegeneration.
In this study, we aimed to examine the course of diabetic neurodegeneration, based on retinal layer thickness and retinal layer integrity analysis in diabetic patients without DR and to evaluate the association of inner retinal reflectivity with the change in retinal layer thicknesses. To our knowledge, this is the first study evaluating the association of retinal reflectivity and neurodegeneration in diabetic patients without DR.
Subjects and methods
This retrospective case–control study was conducted at a tertiary setting upon the approval of the institutional ethical committee and adhered to the tenets of Helsinki. The study group consisted of patients with DM without retinopathy. The control group included healthy subjects, who attended the clinics for ocular examination (spectacle prescription, etc.) and health screening check-up including blood glucose level measurements. All participants should have had a comprehensive ophthalmic examination including anterior and posterior segment examination, intraocular pressure measurement, SD-OCT scans, and at least 1 year follow-up to be eligible for the study.
Exclusion criteria were having current or previous macular oedema/DR of any stage in the study group, having ocular diseases that affect retina/optic disc (glaucoma, macular degeneration, macular oedema, epiretinal membrane, vitreomacular traction, refractive disorder greater than ±4D, etc.), the history of ocular trauma, intraocular surgery within 6 months to the beginning of the study or any time during the follow-up period, vitrectomy regardless of time, systemic disease that could affect RNFL thickness (Alzheimer’s or Parkinson’s diseases etc.), intraocular inflammation, and having poor quality SD-OCT images.
SD-OCT was used for macular segmentation and retinal reflectivity measurements (Heidelberg Spectral Domain Optical Coherence Tomography; Heidelberg Engineering, Dossenheim, Germany). SD-OCT provides 40,000 A scans per second, with an optical resolution of 7 μm axially and 14 μm laterally by using 870-nm wavelength superlunescent diode.
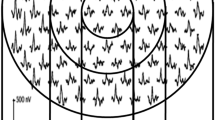
Retinal reflectivity was defined as optical intensity ratios (OIRs) and it was calculated as the mean OCT reflectivity of the certain retinal layer to the mean reflectivity of the retinal pigment epithelium (RPE). The measurement of OIRs was previously described and it is briefly as follows: [18] The SD-OCT images were extracted and imported to ImageJ (http://imagej.nih.gov/ij/) for measuring the reflectivity of retinal layers. To eliminate the effect of the output of the OCT device and pre-retinal optical transmission and variation in signal intensity, normalization of the inner retinal reflectivity to that of the RPE was carried out to create an OIR. This ratio was used for the analysis. A researcher masked to the clinical outcome (OP) manually selected rectangular areas within the ganglion cell layer, inner nuclear layer, and RPE to calculate an OIR by dividing the optical intensity of the particular layer (ganglion cell or inner nuclear layer) by the related RPE intensity. The rectangular areas selected were located at 1 mm from the foveal center, on the papillomacular bundle (Fig. 1). OIR was calculated on the initial OCT scans only to make a correlation analysis with the amount of change in the retinal layer thicknesses throughout time.
Rectangular areas were manually selected within the ganglion cell layer (a), inner nuclear layer (b), and retinal pigment epithelium (RPE) (c) on the SD-OCT images which were imported to ImageJ (http://imagej.nih.gov/ij/) for measuring the reflectivity of retinal layers. Optical intensity ratios were calculated by dividing the optical intensity of the particular layer (ganglion cell or inner nuclear layer) by the related RPE intensity. The rectangular areas selected were located at 1 mm from the foveal center, on the papillomacular bundle.
Segmentation of the macular layers was performed automatically by segmentation application in the OCT device (Segmentation Technology; Heidelberg Engineering). By this application, the thicknesses of RNFL, ganglion, inner plexiform, inner nuclear, outer plexiform, outer nuclear and photoreceptor layers, inner retina, and RPE, in temporal, superior and nasal and inferior sectors within 3 mm were calculated separately and automatically. The average thickness of all sectors within pericentral 3 mm was also manually calculated for each layer.
Only one eye of each participant was included in the study. If both eyes were eligible, the right eye was selected. If the right eye met any of the exclusion criteria, then the left eye was selected for enrolment.
Statistical analysis was performed by SPSS statistical software (SPSS 11.0.0 for MS Windows; SPSS Inc., Chicago, IL). Kolmogorov–Smirnov test was used for determination of the distribution of the data. Independent samples test was used for comparison of data between the study and the control group whereas Mann–Whitney U test for used for the same purpose for non-homogenously distributed data. Paired samples test was used for assessment of initial and final data within the same group whereas Wilcoxon related samples test was used for comparison of non-homogenously distributed data. Categorical variables were compared with the χ2-test. A p value < 0.05 was considered significant. The Bonferroni correction was applied to eliminate type 1 error due to multiple comparisons in assessing sectoral retinal segmentation data.
Results
A total of 80 eyes of 80 patients with DM without retinopathy and 40 eyes of 40 healthy subjects were included in the study. The demographics and ocular characteristics of the groups on the initial visit are shown in Table 1. The groups were compatible in terms of age and gender (p > 0.05). In the study group, three (3.8%) patients had type 1 DM, whereas 77 (96.3%) patients had type 2 DM. The mean duration of DM was 10.5 ± 6.1 (1–25) years, whereas the mean HbA1c level was 8.1 ± 2.2 (5.3–14.9). The mean follow-up was 34.0 ± 20.7 (12–74) months in the study group whereas it was 18.1 ± 7.4 (12–36) months in the control group.
In a qualitative analysis of SD-OCT scans, none of the eyes had disorganization of the retinal inner layers (DRIL), ellipsoid zone (EZ) or the external limiting membrane (ELM) disruption in the study group at the initial and the final visit. Ganglion cell layer OIR was 0.63 ± 0.12 and 0.65 ± 0.12 in the study and control groups respectively (p = 0.526), whereas the inner nuclear layer OIR was 0.49 ± 0.1 and 0.49 ± 0.1 in the study and control groups respectively (p = 0.920).
Table 2 shows the comparison of the thicknesses of the retinal layers at the initial visit and the final visit in the study and the control groups. In the study group, superior, inferior, and nasal sectors in total retinal layers; superior ganglion cell layer, superior and nasal inner plexiform layer; inferior inner nuclear layer and superior and nasal inner retinal layers showed significant thinning, whereas central inner nuclear layer, inferior, and nasal outer plexiform layer showed significant thickening when the initial and final visit values were compared (p < 0.05). After performing Bonferroni correction to avoid type 1 errors in sectoral thickness analysis, the thinning in superior and nasal sectors in total retina, superior ganglion cell layer, nasal inner plexiform layer, and superior inner retinal layers, as well as thickening in inferior outer plexiform layer remained significant (p < 0.0125).
When the average thickness of pericentral retina within 3 mm was assessed; total retina, ganglion cell layer, inner plexiform layer and inner retinal layers showed significant thinning, whereas outer plexiform layer showed significant thickening during the follow-up in the study group (p < 0.05). In the control group, none of the layers showed significant alterations in any sectors between the initial and the final visits (p > 0.05) (Table 2).
When the study and the control groups were compared at the initial visit, the layers were thinner in the study group in general, however the difference did not reach statistical significance in any sectors (p > 0.05). At the final visit, central retina and inferior inner nuclear layer were thinner in the study group than that in the control group (p = 0.028 and p = 0.045 respectively, Table 2). In order to control for the difference in the follow-up period between the groups, the patients with a follow-up range of 12–36 months were re-analyzed (47 eyes in the study group, 40 eyes in the control group). In this analysis, the differences in the central retina and inferior inner nuclear layer thicknesses lost their significance at the final visit (p = 0.134 and p = 0.079 respectively); whereas RPE in superior, temporal and inferior sectors, inferior photoreceptor layer, and pericentral RPE were significantly thinner in the study group (p = 0.020, p = 0.018, p = 0.011, p = 0.005, and p = 0.014, respectively).
The change in thicknesses of layers between the initial and the final visits was described as delta values. The correlations of ganglion cell layer OIR with delta superior retina (r = 0.278, p = 0.013), delta nasal inner retina (r = 0.227, p = 0.043), delta central inner retina (r = 0.247, p = 0.027), delta superior photoreceptor (r = 0.312, p = 0.005), and delta pericentral retina (r = 0.240, p = 0.032) were significant in the study group. The correlations of inner nuclear layer OIR with delta superior retina (r = 0.226, p = 0.044) and delta superior photoreceptor (r = 0.244, p = 0.029) were also significant. In the control group, only delta inferior ganglion cell layer significantly correlated with ganglion cell layer OIR (r = 0.330, p = 0.038) and the inner nuclear layer OIR (r = 0.359, p = 0.023) (Spearman’s correlation).
The mean age significantly correlated with delta values of superior retina (r = 0.342, p = 0.002), temporal retina (r = 0.399, p < 0.001), inferior retina (r = 0.364, p = 0.001), superior ganglion cell layer (r = 0.392, p = p < 0.001), inferior inner plexiform (r = 0.234, p = 0.036), nasal inner plexiform (r = 0.252, p = 0.024), temporal outer nuclear (r = 0.229, p = 0.041), temporal RPE (r = 0.236, p = 0.035), superior inner retina (r = 0.230, p = 0.040), temporal inner retina (r = 0.341, p = 0.002), inferior inner retina (r = 0.391, p < 0.001), nasal inner retina (r = 0.239, p = 0.033), pericentral retina (r = 0.381, p < 0.001), pericentral ganglion cell layer (r = 0.258, p = 0.021), pericentral inner retina (r = 0.355, p = 0.001) in the study group. The duration of DM and the mean HbA1c values did not show significant correlation with any of delta values when adjusted for age (p > 0.05).
In the control group, the mean age correlated with delta values of temporal RNFL (r = 0.396, p = 0.011), nasal ganglion cell layer (r = −0.500, p = 0.001), central outer plexiform (r = 0.334, p = 0.035), central outer nuclear (r = −0.353, p = 0.026) and pericentral outer plexiform (r = 0.335, p = 0.034) layers.
Discussion
The novel finding of our study is that the ganglion cell layer reflectivity significantly correlated with the amount of pericentral retinal thinning during the time course in the study group, which was more prominent in the inner retinal layers. The retinal layer thicknesses were not significantly different between the study and control groups initially; however, the central retina was thinner in the study group at the final visit. The study group showed significant thinning in various layers, particularly in the inner retinal layers; however, none of the eyes developed DRIL, the disruption of EZ or ELM throughout the follow-up period.
Several biomarkers have been proposed to predict visual outcomes and do better management decisions in various diseases. Recently, retinal reflectivity, DRIL and the integrity of outer retinal layers have become subject of interest for their potential to serve as prognostic/predictive markers [16,17,18, 22,23,24,25]. Alterations in retinal reflectivity might be seen in ischemic conditions such as retinal artery/vein occlusion and DR [16,17,18,19, 26, 27]. Hyperreflectivity of the ganglion cell layer was shown in retinal artery occlusion, an increased reflectivity at the level of the inner nuclear layer was demonstrated at the level of the inner nuclear layer in the paracentral acute middle maculopathy [16, 17]. Wanek et al. showed that DR patients demonstrated higher inner nuclear layer reflectivity compared to controls, whereas Gao et al. reported that total reflectivity was lower in DR and it showed a better discriminating power between DR and healthy eyes compared to thickness [26, 27]. Similarly, Toprak et al. documented lower photoreceptor inner segment ellipsoid layer reflectivity in eyes with DR compared to controls [19]. However, retinal reflectivity has not been evaluated as a prognostic factor until the study of Mehta et al [18]. The authors showed that increased reflectivity at 1-month was associated with a poorer visual acuity at 1-year in eyes with acute central retinal vein occlusion. Despite the retinal reflectivity was previously compared in diabetic and healthy eyes with conflicting results, there is a lack of information about its role as a marker in the progression of retinal neurodegeneration in DM [19, 26, 27] In our study, we found that the ganglion cell layer and inner nuclear layer OIR correlated with the change in retinal thickness over time, indicating that the inner retinal reflectivity shows a correlation with neurodegenerative process as documented by the amount of retinal thinning in diabetic patients without DR.
DRIL and the integrity of outer retinal layers were also used as retinal biomarkers in diabetes [24, 25]. It has been suggested that DRIL could indicate disorganization/damage of cells within inner retina and might indicate the change of transmission pathways in the retina [24]. Another hypothesis was the axonal snap secondary to excess amount of swelling [28]. Sun et al. showed that DRIL was associated with worse visual acuity and the change in DRIL predicted future change in visual acuity [24]. In another study, Das et al. showed that that central DRIL correlated with visual acuity in eyes with central DME and they also documented that DRIL was strongly associated with the disruption of EZ and ELM [25]. DRIL might also be seen in eyes without DR [29]. Joltikov et al. assessed DRIL in DM patients without and with DR and identified DRIL in one diabetic patient without DR, in eight patients with NPDR [29]. The authors reported that having DRIL was associated with decreased visual acuity, contrast sensitivity, and perimetry scores as well as inner retinal thinning. In our study, we assessed the integrity of retinal layers to make a qualitative analysis of neurodegeneration throughout the follow-up, however, none of the patients with DM had DRIL, the disruption of EZ or ELM at the initial or final visit. Our findings suggest that the impairment of retinal layer integrity might be occurring at a later stage, after DR appears.
There is very limited information related to the course of retinal thinning in DM.
Lim et al. longitudinally observed neuroretinal alterations in healthy subjects and diabetic patients with and without retinopathy and found progressive peripapillary RNFL thinning in both groups, which was greater in the DM group, after 3 years of observation [20]. The authors also suggested that ischemic and metabolic damage might be more accumulated in DM patients with DR. In another longitudinal study, Sohn et al. reported significant, progressive loss of RNFL and the ganglion cell /inner plexiform layer in DM patients over 4 years [21]. Van de Kreeke et al. documented significant thinning in RNFL and ganglion cell layer, whereas significant thickening in the inner plexiform layer during 6 years in patients with type 1 DM without DR or minimal DR, with more pronounced alterations in eyes with DR [14]. Kim et al. reported that ganglion cell-inner plexiform layer was thinner in eyes which show a progression in DR during a follow-up of ≥4 years and concluded that progressive loss of ganglion cell-inner plexiform layer was an independent risk factor for progression of DR [30]. Pinilla et al. revealed that, during 8 years, diabetic patients showed a significant thinning in total retinal thickness, secondary to the thinning of the inner retinal layers, except the outer temporal zone; whereas the control group showed a thinning only in the inferior zone [15]. Similarly, in our study, DM patients without DR showed significant thinning in multiple layers, which was more prominent in the inner layers, supporting the suggestion that neuroretinal alterations could occur early in DM and precede diabetic vascular changes. In our control group, there wasn’t significant thinning in any layer at the final visit compared to the initial values, however, the results might differ with longer follow-up.
The limitations of our study are the retrospective nature of the study, the small sample size, and the limited follow-up period.
In conclusion, we found that the diabetic patients without DR showed significant retinal thinning in various layers, particularly in the inner retinal layers, however, none of the eyes developed DRIL, the disruption of EZ or ELM throughout the follow-up period. The ganglion cell layer reflectivity significantly correlated with the amount of pericentral retinal thinning during the time course in the study group, which was more remarkable in the inner retinal layers. Future studies with larger cohort and a longitudinal analysis are needed to determine the potential utility of retinal reflectivity for the prediction of neuroretinal degeneration in DM.
Summary table
What was known before
-
Retinal thinning appeared in eyes with no or minimal diabetic retinopathy during the time course.
What this study adds
-
Ganglion cell layer reflectivity significantly correlated with the amount of pericentral retinal thinning in time course in diabetic patients without retinopathy.
References
Zhang X, Saaddine JB, Chou CF, Cotch MF, Cheng YJ, Geiss LS, et al. Prevalence of diabetic retinopathy in the United States, 2005–2008. JAMA. 2010;304:649–56.
Antcliff RJ, Marshall J. The pathogenesis of edema in diabetic maculopathy. Semin Ophthalmol. 1999;14:223–32.
Kim K, Kim ES, Kim DG, Yu SY. Progressive retinal neurodegeneration and microvascular change in diabetic retinopathy: longitudinal study using OCT angiography. Acta Diabetol. 2019;56:1275–82.
De Clerck EEB, Schouten JSAG, Berendschot TTJM, Goezinne F, Dagnelie PC, Schaper NC, et al. Macular thinning in prediabetes or type 2 diabetes without diabetic retinopathy: the Maastricht Study. Acta Ophthalmol. 2018;96:174–82.
Chhablani J, Sharma A, Goud A, Peguda HK, Rao HL, Begum VU, et al. Neurodegeneration in Type 2 diabetes: evidence from spectral-domain optical coherence tomography. Invest Ophthalmol Vis Sci. 2015;56:6333–8.
Barber AJ, Gardner TW, Abcouwer SF. The significance of vascular and neural apoptosis to the pathology of diabetic retinopathy. Invest Ophthalmol Vis Sci. 2011;52:1156–63. 28
Gastinger MJ, Kunselman AR, Conboy EE, Bronson SK, Barber AJ. Dendrite remodeling and other abnormalities in the retinal ganglion cells of Ins2 Akita diabetic mice. Invest Ophthalmol Vis Sci. 2008;49:2635–42.
Carrasco E, Hernández C, de Torres I, Farrés J, Simó R. Lowered cortistatin expression is an early event in the human diabetic retina and is associated with apoptosis and glial activation. Mol Vis. 2008;15:1496–502. 14
Verma A, Rani PK, Raman R, Pal SS, Laxmi G, Gupta M, et al. Is neuronal dysfunction an early sign of diabetic retinopathy? Microperimetry and spectral domain optical coherence tomography (SD-OCT) study in individuals with diabetes, but no diabetic retinopathy. Eye (Lond). 2009;23:1824–30.
Laron M, Bearse MA Jr, Bronson-Castain K, Jonasdottir S, King-Hooper B, Barez S, et al. Interocular symmetry of abnormal multifocal electroretinograms in adolescents with diabetes and no retinopathy. Invest Ophthalmol Vis Sci. 2012;53:316–21. 25
Tyrberg M, Lindblad U, Melander A, Lövestam-Adrian M, Ponjavic V, Andréasson S. Electrophysiological studies in newly onset type 2 diabetes without visible vascular retinopathy. Doc Ophthalmol. 2011;123:193–8.
Garcia-Martin E, Bambo MP, Marques ML, Satue M, Otin S, Larrosa JM, et al. Ganglion cell layer measurements correlate with disease severity in patients with Alzheimer’s disease. Acta Ophthalmol. 2016;94:e454–9.
Bittersohl D, Stemplewitz B, Keserü M, Buhmann C, Richard G, Hassenstein A. Detection of retinal changes in idiopathic Parkinson’s disease using high-resolution optical coherence tomography and heidelberg retina tomography. Acta Ophthalmol. 2015;93:e578–84.
van de Kreeke JA, Darma S, Chan Pin Yin JMPL, Tan HS, Abramoff MD, JWR Twisk, et al. The spatial relation of diabetic retinal neurodegeneration with diabetic retinopathy. PLoS One. 2020;15:e0231552. 16
Pinilla I, Idoipe M, Perdices L, Sanchez-Cano A, Acha J, Lopez-Galvez MI, et al. Changes in total and inner retinal thicknesses in type 1 diabetes with no retinopathy after 8 years of follow-up. Retina. 2020;40:1379–86.
Furashova O, Matthé E. Retinal changes in different grades of retinal artery occlusion: an optical coherence tomography study. Invest Ophthalmol Vis Sci. 2017;58:5209–16. 1
Browning DJ, Punjabi OS, Lee C. Assessment of ischemia in acute central retinal vein occlusion from inner retinal reflectivity on spectral domain optical coherence tomography. Clin Ophthalmol. 2016;22:71–79.
Mehta N, Lavinsky F, Gattoussi S, Seiler M, Wald KJ, Ishikawa H, et al. Increased inner retinal layer reflectivity in eyes with acute crvo correlates with worse visual outcomes at 12 months. Invest Ophthalmol Vis Sci. 2018;59:3503–10. 2
Toprak I, Yildirim C, Yaylali V. Impaired photoreceptor inner segment ellipsoid layer reflectivity in mild diabetic retinopathy. Can J Ophthalmol. 2015;50:438–41.
Lim HB, Shin YI, Lee MW, Park GS, Kim JY. Longitudinal changes in the peripapillary retinal nerve fiber layer thickness of patients with type 2 diabetes. JAMA Ophthalmol. 2019;137:1125–32.
Sohn EH, van Dijk HW, Jiao C, Kok PH, Jeong W, Demirkaya N, et al. Retinal neurodegeneration may precede microvascular changes characteristic of diabetic retinopathy in diabetes mellitus. Proc Natl Acad Sci USA. 2016;113:E2655–64. 10
Eliwa TF, Hussein MA, Zaki MA, Raslan OA. Outer retinal layer thickness as good visual predictor in patients with diabetic macular edema. Retina. 2018;38:805–11.
Campos A, Campos EJ, do Carmo A, Caramelo F, Martins J, Sousa JP, et al. Evaluation of markers of outcome in real-world treatment of diabetic macular edema. Eye Vis (Lond). 2018;5:27. 11
Sun JK, Lin MM, Lammer J, Prager S, Sarangi R, Silva PS, et al. Disorganization of the retinal inner layers as a predictor of visual acuity in eyes with center-involved diabetic macular edema. JAMA Ophthalmol. 2014;132:1309–16.
Das R, Spence G, Hogg RE, Stevenson M, Chakravarthy U. Disorganization of inner retina and outer retinal morphology in diabetic macular edema. JAMA Ophthalmol. 2018;136:202–8. 1
Wanek J, Blair NP, Chau FY, Lim JI, Leiderman YI, Shahidi M. Alterations in retinal layer thickness and reflectance at different stages of diabetic retinopathy by en face optical coherence tomography. Invest Ophthalmol Vis Sci. 2016;57:OCT341–7. 1
Gao W, Tátrai E, Ölvedy V, Varga B, Laurik L, Somogyi A, et al. Investigation of changes in thickness and reflectivity from layered retinal structures of healthy and diabetic eyes with optical coherence tomography. J Biomed Sci Eng. 2011;4:657–65.
Pelosini L, Hull CC, Boyce JF, McHugh D, Stanford MR, Marshall J. Optical coherence tomography may be used to predict visual acuity in patients with macular edema. Invest Ophthalmol Vis Sci. 2011;52:2741–8. 25
Joltikov KA, Sesi CA, de Castro VM, Davila JR, Anand R, Khan SM, et al. Disorganization of retinal inner layers (DRIL) and neuroretinal dysfunction in early diabetic retinopathy. Invest Ophthalmol Vis Sci. 2018;59:5481–6. 1
Kim K, Kim ES, Yu SY. Longitudinal relationship between retinal diabetic neurodegeneration and progression of diabetic retinopathy in patients with type 2 diabetes. Am J Ophthalmol. 2018;196:165–72.
Acknowledgements
This study was presented in part (poster presentation) at the 20th EURETINA (Virtual Congress, October 2020).
Author information
Authors and Affiliations
Contributions
ENC was responsible for the conception and design of the study, and was a major contributor in data analysis, interpretation and drafting of the manuscript. OP, HSA and GP collected and interpreted the data and contributed in writing the manuscript. All authors approved the final version and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cetin, E.N., Parca, O., Akkaya, H.S. et al. Association of inner retinal reflectivity with qualitative and quantitative changes in retinal layers over time in diabetic eyes without retinopathy. Eye 36, 1253–1260 (2022). https://doi.org/10.1038/s41433-021-01607-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01607-w