Abstract
Background/Objectives:
The objective of this study was to develop new equations for predicting basal metabolic rate (BMR) in Prader–Willi syndrome (PWS) subjects and to compare their accuracy with commonly used equations developed by Lazzer (2007), Livingston (2005), Huang (2004), Nelson (1992), Mifflin (1990), Owen (1987), WHO (1985), Bernstein (1983) and Harris–Benedict (1919), using the Bland–Altman method.
Subjects/Methods:
BMR was measured by indirect calorimetry and fat-free mass (FFM) and fat mass (FM) by a tetrapolar impedancemeter in 80 Caucasian PWS patients (mean body mass index: 39.1 kg/m2; 17–50 years). Equations were derived by stepwise multiple regression analysis using a calibration group (n:50) and tested against the validation group (n:30).
Results:
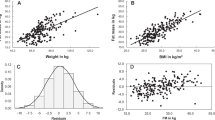
Two new equations, based on anthropometric (BMR=body mass × 0.052+sex × 0.778–age × 0.033+2.839 (R2adj=0.61, s.e.=0.89 MJ per day)) or body composition (BMR=FFMx0.074+FMx0.042+sexx0.636–agex0.037+2.515 (R2adj=0.69, s.e.=0.82 MJ per day)), were generated. Predicted BMR (PBMR) was not significantly different from the measured BMR (<3.3%), and was accurate in 59% and 62% of patients, respectively. Nevertheless, significant magnitude bias was found for both equations (P<0.001, R2=0.36). The Owen (1987), Mifflin (1990), Huang (2004) and Lazzer (2007) equations showed mean differences <5% and PBMR was accurate in ~50% of patients. The Livingston (2005), WHO (1985) and Harris–Benedict (1919) equations showed a PBMR overestimation >7% and were accurate in <50% of patients. The Nelson (1992) and Bernstein (1983) equations showed a greater PBMR underestimation in >60% of subjects.
Conclusions:
The new prediction equations showed significantly higher accuracy compared with equations tested, with exception of Lazzer (2007) and Livingston (2005) equations, and result in lower mean differences and lower limits of agreement compared with the equations tested.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Cassidy SB, Schwartz S, Miller JL, Driscoll DJ . Prader–Willi syndrome. Genet Med 2012; 14: 10–26.
Nicholls RD, Knoll JH, Butler MG, Karam S, Lalande M . Genetic imprinting suggested by maternal heterodisomy in nondeletion Prader–Willi syndrome. Nature 1989; 342: 281–285.
Butler MG . Prader–Willi syndrome: obesity due to genomic imprinting. Curr Genom 2011; 12: 204–215.
Goldstone AP, Beales PL . Genetic obesity syndromes. Front Horm Res 2008; 36: 37–60.
Butler MG, Theodoro MF, Bittel DC, Donnelly JE . Energy expenditure and physical activity in Prader–Willi syndrome: comparison with obese subjects. Am J Med Genet A 2007; 143A: 449–459.
Bedogni G, Grugni G, Tringali G, Agosti F, Sartorio A . Assessment of fat-free mass from bioelectrical impedance analysis in obese women with Prader–Willi syndrome. Ann Hum Biol 2014, e-pub ahead of print 26 December 2014.
Brambilla P, Bosio L, Manzoni P, Pietrobelli A, Beccaria L, Chiumello G . Peculiar body composition in patients with Prader–Labhart–Willi syndrome. Am J Clin Nutr 1997; 65: 1369–1374.
van Mil EA, Westerterp KR, Gerver WJ, Curfs LM, Schrander-Stumpel CT, Kester AD et al. Energy expenditure at rest and during sleep in children with Prader–Willi syndrome is explained by body composition. Am J Clin Nutr 2000; 71: 752–756.
Goldstone AP, Brynes AE, Thomas EL, Bell JD, Frost G, Holland A et al. Resting metabolic rate, plasma leptin concentrations, leptin receptor expression, and adipose tissue measured by whole-body magnetic resonance imaging in women with Prader–Willi syndrome. Am J Clin Nutr 2002; 75: 468–475.
Cataletto M, Angulo M, Hertz G, Whitman B . Prader–Willi syndrome: a primer for clinicians. Int J Pediatr Endocrinol 2011; 2011: 12.
Foster GD, McGuckin BG . Estimating resting energy expenditure in obesity. Obes Res 2001; 9: 367S–372S; discussion 373S–374S.
Harris JA, Benedict FG . A Biometric Study of Basal Metabolism in Man, Vol. 279. Carnegie Institute of Washington: Washington, DC, 1919.
Schoeller DA, Levitsky LL, Bandini LG, Dietz WW, Walczak A . Energy expenditure and body composition in Prader–Willi syndrome. Metabolism 1988; 37: 115–120.
Lazzer S, Agosti F, Resnik M, Marazzi N, Mornati D, Sartorio A . Prediction of resting energy expenditure in severely obese Italian males. J Endocrinol Invest 2007; 30: 754–761.
Lazzer S, Agosti F, Silvestri P, Derumeaux-Burel H, Sartorio A . Prediction of resting energy expenditure in severely obese Italian women. J Endocrinol Invest 2007; 30: 20–27.
Livingston EH, Kohlstadt I . Simplified resting metabolic rate-predicting formulas for normal-sized and obese individuals. Obes Res 2005; 13: 1255–1262.
Huang KC, Kormas N, Steinbeck K, Loughnan G, Caterson ID . Resting metabolic rate in severely obese diabetic and nondiabetic subjects. Obes Res 2004; 12: 840–845.
Nelson KM, Weinsier RL, Long CL, Schutz Y . Prediction of resting energy expenditure from fat-free mass and fat mass. Am J Clin Nutr 1992; 56: 848–856.
Mifflin MD St, Jeor ST, Hill LA, Scott BJ, Daugherty SA, Koh YO . A new predictive equation for resting energy expenditure in healthy individuals. Am J Clin Nutr 990; 51: 241–247.
Owen OE, Holup JL, D'Alessio DA, Craig ES, Polansky M, Smalley KJ et al. A reappraisal of the caloric requirements of men. Am J Clin Nutr 1987; 46: 875–885.
WHO Energy and Protein Requirements: Report of a Joint FAO/WHO/UNU Expert Consultation. WHO Technical Report Series No. 724. WHO: Geneva, Switzerland, 1985.
Bernstein RS, Thornton JC, Yang MU, Wang J, Redmond AM, Pierson RN Jr et al. Prediction of the resting metabolic rate in obese patients. Am J Clin Nutr 1983; 37: 595–602.
Lukaski HC, Bolonchuk WW, Hall CB, Siders WA . Validation of tetrapolar bioelectrical impedance method to assess human body composition. J Appl Physiol 1986; 60: 1327–1332.
Gray DS, Bray GA, Gemayel N, Kaplan K . Effect of obesity on bioelectrical impedance. Am J Clin Nutr 1989; 50: 255–260.
Weir JB . New methods for calculating metabolic rate with special references to protein metabolism. J Physiol (Lond) 1949; 109: 1–9.
Bland JM, Altman DG . Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; 1: 307–310.
Phang PT, Rich T, Ronco J . A validation and comparison study of two metabolic monitors. J Parenter Enteral Nutr 1990; 14: 259–261.
Sabounchi NS, Rahmandad H, Ammerman A . Best-fitting prediction equations for basal metabolic rate: informing obesity interventions in diverse populations. Int J Obes (Lond) 2013; 37: 1364–1370.
Miller AT Jr, Blyth CS . Lean body mass as a metabolic reference standard. J Appl Physiol 1953; 5: 311–316.
Gallagher D, Allen A, Wang Z, Heymsfield SB, Krasnow N . Smaller organ tissue mass in the elderly fails to explain lower resting metabolic rate. Ann NY Acad Sci 2000; 904: 449–455.
Gallagher D, Belmonte D, Deurenberg P, Wang Z, Krasnow N, Pi-Sunyer FX et al. Organ-tissue mass measurement allows modeling of REE and metabolically active tissue mass. Am J Physiol 1998; 275: E249–E258.
Wang Z, Heshka S, Wang J, Gallagher D, Deurenberg P, Chen Z et al. Metabolically active portion of fat-free mass: a cellular body composition level modeling analysis. Am J Physiol Endocrinol Metab 2007; 292: E49–E53.
Wang Z, Heshka S, Heymsfield SB, Shen W, Gallagher D . A cellular-level approach to predicting resting energy expenditure across the adult years. Am J Clin Nutr 2005; 81: 799–806.
Leibel RL, Rosenbaum M, Hirsch J . Changes in energy expenditure resulting from altered body weight. N Engl J Med 1995; 332: 621–628.
Acknowledgements
We are grateful to the patients for their kind collaboration, and the nursing staff at the Division of Auxology, Istituto Auxologico Italiano, IRCCS, Piancavallo (VB) for their qualified assistance during the clinical study. The study was supported by Progetti di Ricerca Corrente, Italian Institute for Auxology, Milan, Italy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Lazzer, S., Grugni, G., Tringali, G. et al. Prediction of basal metabolic rate in patients with Prader–Willi syndrome. Eur J Clin Nutr 70, 494–498 (2016). https://doi.org/10.1038/ejcn.2015.161
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2015.161
This article is cited by
-
Prader–Willi Syndrome in Adults: An Update On Nutritional Treatment and Pharmacological Approach
Current Obesity Reports (2022)
-
Body composition and obstructive sleep apnoea assessment in adult patients with Prader–Willi syndrome: a case control study
Journal of Endocrinological Investigation (2022)