Abstract
Background/Objectives
Type 1 diabetes (T1D) is associated with an increase in resting metabolic rate (RMR), but the impact of T1D on other components of 24-h energy expenditure (24-h EE) is not known. Also, there is a lack of equations to estimate 24-h EE in patients with T1D. The aims of this analysis were to compare 24-h EE and its components in young adults with T1D and healthy controls across the spectrum of body mass index (BMI) and derive T1D-specific equations from clinical variables.
Subjects/Methods
Thirty-three young adults with T1D diagnosed ≥1 year prior and 33 healthy controls matched for sex, age and BMI were included in this analysis. We measured 24-h EE inside a whole room indirect calorimeter (WRIC) and body composition with dual x-ray absorptiometry.
Results
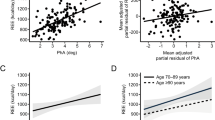
Participants with T1D had significantly higher 24-h EE than healthy controls (T1D = 2047 ± 23 kcal/day vs control= 1908 ± 23 kcal/day; P < 0.01). We derived equations to estimate 24-h EE with both body composition (fat free mass + fat mass) and anthropometric (weight + height) models, which provided high coefficients of determination (R2 = 0.912 for both). A clinical model that did not incorporate spontaneous physical activity yielded high coefficients of determination as well (R2 = 0.897 and R2 = 0.880 for body composition and anthropometric models, respectively).
Conclusion
These results confirm that young adults with established T1D have increased 24-h EE relative to controls without T1D. The derived equations from clinically available variables can assist clinicians with energy prescriptions for weight management in patients with T1D.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Data can be available upon reasonable request and approval of the principal investigator of each study involved in this publication.
References
Baskaran C, Volkening LK, Diaz M, Laffel LM. A decade of temporal trends in overweight/obesity in youth with type 1 diabetes after the diabetes control and complications trial. Pediatr Diabetes. 2015;16:263–70. https://doi.org/10.1111/pedi.12166.
Conway B, Miller RG, Costacou T, Fried L, Kelsey S, Evans RW, et al. Temporal patterns in overweight and obesity in Type 1 diabetes. Diabet Med. 2010;27:398–404. https://doi.org/10.1111/j.1464-5491.2010.02956.x.
Minges KE, Whittemore R, Weinzimer SA, Irwin ML, Redeker NS, Grey M. Correlates of overweight and obesity in 5529 adolescents with type 1 diabetes: The T1D Exchange Clinic Registry. Diabetes Res Clin Pr. 2017;126:68–78. https://doi.org/10.1016/j.diabres.2017.01.012.
Vilarrasa N, San Jose P, Rubio MA, Lecube A. Obesity in patients with type 1 diabetes: links, risks and management challenges. Diabetes Metab Syndr Obes. 2021;14:2807–27. https://doi.org/10.2147/DMSO.S223618.
Woods SC, Seeley RJ, Porte D, Schwartz MW. Signals that regulate food intake and energy homeostasis. Science. 1998;280:1378–83. https://doi.org/10.1126/science.280.5368.1378.
Corbin KD, Driscoll KA, Pratley RE, Smith SR, Maahs DM, Mayer-Davis EJ, et al. Obesity in type 1 diabetes: pathophysiology, clinical impact, and mechanisms. Endocr Rev. 2018;39:629–63. https://doi.org/10.1210/er.2017-00191.
Carlson MG, Campbell PJ. Intensive insulin therapy and weight gain in IDDM. Diabetes. 1993;42:1700–7. https://doi.org/10.2337/diab.42.12.1700.
Greco AV, Tataranni PA, Mingrone G, De Gaetano A, Manto A, Cotroneo P, et al. Daily energy metabolism in patients with type 1 diabetes mellitus. J Am Coll Nutr. 1995;14:286–91.
Jacob AN, Salinas K, Adams-Huet B, Raskin P. Potential causes of weight gain in type 1 diabetes mellitus. Diabetes Obes Metab. 2006;8:404–11. https://doi.org/10.1111/j.1463-1326.2005.00515.x.
Nair KS, Halliday D, Garrow JS. Increased energy expenditure in poorly controlled Type 1 (insulin-dependent) diabetic patients. Diabetologia. 1984;27:13–16. https://doi.org/10.1007/BF00253494.
Rigalleau V, Lasseur C, Pecheur S, Chauveau P, Combe C, Perlemoine C, et al. Resting energy expenditure in uremic, diabetic, and uremic diabetic subjects. J Diabetes Complicat. 2004;18:237–41. https://doi.org/10.1016/S1056-8727(03)00077-1.
Leslie P, Jung RT, Isles TE, Baty J, Newton RW, Illingworth P. Effect of optimal glycaemic control with continuous subcutaneous insulin infusion on energy expenditure in type I diabetes mellitus. Br Med J (Clin Res Ed. 1986;293:1121–6. https://doi.org/10.1136/bmj.293.6555.
Molnar D, Decsi T, Soltesz G. Resting energy expenditure and food-induced thermogenesis in diabetic children receiving continuous subcutaneous insulin infusion. Diabetes Res. 1988;7:117–21.
Chen KY, Smith S, Ravussin E, Krakoff J, Plasqui G, Tanaka S, et al. Room indirect calorimetry operating and reporting standards (RICORS 1.0): a guide to conducting and reporting human whole-room calorimeter studies. Obes (Silver Spring). 2020;28:1613–25. https://doi.org/10.1002/oby.22928.
Carnero EA, Bock CP, Distefano G, Corbin KD, Stephens NA, Pratley RE, et al. Twenty-four hour assessments of substrate oxidation reveal differences in metabolic flexibility in type 2 diabetes that are improved with aerobic training. Diabetologia. 2021;64:2322–33. https://doi.org/10.1007/s00125-021-05535-y.
Ethical Principles for Medical Research Involving Human Subjects. In: The World Medical Association I, (ed.) 64th WMA General Assembly. Fortaleza, Brazil, (2013).
Hall KD, Chen KY, Guo J, Lam YY, Leibel RL, Mayer LE, et al. Energy expenditure and body composition changes after an isocaloric ketogenic diet in overweight and obese men. Am J Clin Nutr. 2016;104:324–33. https://doi.org/10.3945/ajcn.116.133561.
Schutz Y, Bessard T, Jequier E. Diet-induced thermogenesis measured over a whole day in obese and nonobese women. Am J Clin Nutr. 1984;40:542–52. https://doi.org/10.1093/ajcn/40.3.542.
Lam YY, Redman LM, Smith SR, Bray GA, Greenway FL, Johannsen D, et al. Determinants of sedentary 24-h energy expenditure: equations for energy prescription and adjustment in a respiratory chamber. Am J Clin Nutr. 2014;99:834–42. https://doi.org/10.3945/ajcn.113.079566.
Ravussin E, Lillioja S, Anderson TE, Christin L, Bogardus C. Determinants of 24-hour energy expenditure in man. Methods and results using a respiratory chamber. J Clin Invest. 1986;78:1568–78. https://doi.org/10.1172/JCI112749.
Lin LI. A concordance correlation coefficient to evaluate reproducibility. Biometrics. 1989;45:255–68.
Holiday DB, Ballard JE, McKeown BC. PRESS-related statistics: regression tools for cross-validation and case diagnostics. Med Sci Sports Exerc. 1995;27:612–20.
Byrne NM, Weinsier RL, Hunter GR, Desmond R, Patterson MA, Darnell BE, et al. Influence of distribution of lean body mass on resting metabolic rate after weight loss and weight regain: comparison of responses in white and black women. Am J Clin Nutr. 2003;77:1368–73. https://doi.org/10.1093/ajcn/77.6.1368.
Heymsfield SB, Gallagher D, Kotler DP, Wang Z, Allison DB, Heshka S. Body-size dependence of resting energy expenditure can be attributed to nonenergetic homogeneity of fat-free mass. Am J Physiol Endocrinol Metab. 2002;282:E132–138. https://doi.org/10.1152/ajpendo.2002.282.1.E132.
Wang Z, Heshka S, Wang J, Gallagher D, Deurenberg P, Chen Z, et al. Metabolically active portion of fat-free mass: a cellular body composition level modeling analysis. Am J Physiol Endocrinol Metab. 2007;292:E49–53. https://doi.org/10.1152/ajpendo.00485.2005.
Habib SL. Kidney atrophy vs hypertrophy in diabetes: which cells are involved? Cell Cycle. 2018;17:1683–7. https://doi.org/10.1080/15384101.2018.1496744.
Starzl TE, Porter KA, Kashiwagi N. Portal hepatotrophic factors, diabetes mellitus and acute liver atrophy, hypertrophy and regeneration. Surg Gynecol Obstet. 1975;141:843–58.
Monaco CMF, Perry CGR, Hawke TJ. Alterations in mitochondrial functions and morphology in muscle and non-muscle tissues in type 1 diabetes: implications for metabolic health. Exp Physiol. 2020;105:565–70. https://doi.org/10.1113/EP088096.
Caron N, Peyrot N, Caderby T, Verkindt C, Dalleau G. Energy expenditure in people with diabetes mellitus: a review. Front Nutr. 2016;3:56. https://doi.org/10.3389/fnut.2016.00056. e-pub ahead of print 20161222
Boden G, Cheung P, Homko C. Effects of acute insulin excess and deficiency on gluconeogenesis and glycogenolysis in type 1 diabetes. Diabetes. 2003;52:133–7. https://doi.org/10.2337/diabetes.52.1.133.
Boden G, Chen X, Stein TP. Gluconeogenesis in moderately and severely hyperglycemic patients with type 2 diabetes mellitus. Am J Physiol Endocrinol Metab. 2001;280:E23–30. https://doi.org/10.1152/ajpendo.2001.280.1.E23.
Bray GA, Smith SR, DeJonge L, de Souza R, Rood J, Champagne CM, et al. Effect of diet composition on energy expenditure during weight loss: the POUNDS LOST Study. Int J Obes (2005). 2012;36:448–55. https://doi.org/10.1038/ijo.2011.173.
Bosy-Westphal A, Muller MJ, Boschmann M, Klaus S, Kreymann G, Luhrmann PM, et al. Grade of adiposity affects the impact of fat mass on resting energy expenditure in women. Br J Nutr. 2009;101:474–7. https://doi.org/10.1017/s0007114508020357.
Levine JA, Eberhardt NL, Jensen MD. Role of nonexercise activity thermogenesis in resistance to fat gain in humans. Science. 1999;283:212–4. https://doi.org/10.1126/science.283.5399.212.
Garland T Jr., Schutz H, Chappell MA, Keeney BK, Meek TH, Copes LE, et al. The biological control of voluntary exercise, spontaneous physical activity and daily energy expenditure in relation to obesity: human and rodent perspectives. J Exp Biol. 2011;214:206–29. https://doi.org/10.1242/jeb.048397.
Aydin BN, Stinson EJ, Cabeza De Baca T, Ando T, Travis KT, Piaggi P, et al. Investigation of seasonality of human spontaneous physical activity and energy expenditure in respiratory chamber in Phoenix, Arizona. Eur J Clin Nutr. 2024;78:27–33. https://doi.org/10.1038/s41430-023-01347-y. e-pub ahead of print 20231013.
Jeran S, Steinbrecher A, Haas V, Mahler A, Boschmann M, Westerterp KR, et al. Prediction of activity-related energy expenditure under free-living conditions using accelerometer-derived physical activity. Sci Rep. 2022;12:16578. https://doi.org/10.1038/s41598-022-20639-0.
Liguori G, American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription, 11th edn Lippincott®, (2021).
Borsheim E, Bahr R. Effect of exercise intensity, duration and mode on post-exercise oxygen consumption. Sports Med. 2003;33:1037–60. https://doi.org/10.2165/00007256-200333140-00002.
LaForgia J, Withers RT, Gore CJ. Effects of exercise intensity and duration on the excess post-exercise oxygen consumption. J Sports Sci. 2006;24:1247–64. https://doi.org/10.1080/02640410600552064.
Acknowledgements
We sincerely thank to Christopher P. Bock for his help running the WRIC studies.
Funding
The main dataset of this analysis was funded by the National Institute of Diabetes and Digestive and Kidney Diseases (DP3DK113358). Additionally, a data subset was funded by Eli Lilly and Company (NCT02211586), NIDDK (R01DK105829) and Nutrition Sciences Initiative (NCT01967563).
Author information
Authors and Affiliations
Contributions
EAC and REP were involved in the conception, design and the analysis and interpretation of the results. EAC wrote the first draft of the manuscript, and all authors edited, reviewed, and approved the final version of the manuscript. REP is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
All procedures were approved by AdventHealth Institutional Review Board which follows the Declaration of Helsinki for medical research involving human subjects.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Carnero, E.A., Corbin, K.D., Casu, A. et al. 24-h energy expenditure in people with type 1 diabetes: impact on equations for clinical estimation of energy expenditure. Eur J Clin Nutr (2024). https://doi.org/10.1038/s41430-024-01446-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41430-024-01446-4