Abstract
Background/Objectives:
Enterocutaneous fistula (ECF) is a serious complication of Crohn’s disease (CD). Enteral nutrition (EN) is believed as one of therapeutic strategies of CD. This study is dedicated to identify predictors of response to EN in CD, which may lead to a better selection of fistula patients for this therapy.
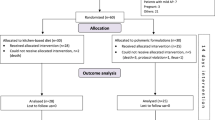
Subjects/Methods:
Forty-eight CD patients with ECF treated with short-peptide-based EN for 3 months were included in this study. All patients were followed up for at least 6 months. Logistic regression was performed to investigate the potential predictors of response to EN in these patients.
Results:
In total, 30 out of 48 patients were confirmed with a successful closure of fistula after 3 months’ EN therapy. The average closure time was 32.4±8.85 days. Inflammatory parameters (erythrocyte sedimentation rate, C-reactive protein (CRP) and platelet count) improved significantly after EN therapy in all enrolled patients. Specifically, the improvement of CRP after therapy in closed group was more important compared with that in unclosed group (P=0.035). Nutrition status (body weight, body mass index (BMI), hemoglobin, serum albumin (ALB), serum prealbumin and total protein (TP)) improved as well (P<0.05). Similarly, after treatment, the improvement of serum albumin (P=0.046) and prealbumin (P=0.006) in closed group was much more important than those in unclosed group. Logistic regression analysis discovered that a decreased CRP level and an elevated BMI level would be beneficial to the response to EN in CD patients with ECF.
Conclusions:
In CD patients with ECF, lower CRP and higher BMI are associated with higher possibility of closure after EN treatment. EN therapy can lead to a closure of ECF in a certain proportion of patients. EN therapy could also ameliorate inflammatory condition and improve nutrition status.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Vavricka SR, Rogler G . Fistula treatment: the unresolved challenge. Dig Dis 2010; 28: 556–564.
Schwartz DA, Loftus EV, Tremaine WJ, Panaccione R, Scott Harmsen W, Zinsmeister AR et al. The natural history of fistulizing Crohn's disease in Olmsted County, Minnesota. Gastroenterology 2002; 122: 875–880.
Judge TA, Lichtenstein GR . Treatment of fistulizing Crohn's disease. Gastroenterol Clin North Am 2004; 33: 421–454.
Norman K, Kirchner H, Lochs H, Pirlich M . Malnutrition affects quality of life in gastroenterology patients. World J Gastroenterol 2006; 12: 3380–3385.
Dupont B, Dupont C, Justum AM, Piquet MA, Reimund JM . Enteral nutrition in adult Crohn's disease: present status and perspectives. Mol Nutr Food Res 2008; 52: 875–884.
Filippi J, Al-Jaouni R, Wiroth JB, Hebuterne X, Schneider SM . Nutritional deficiencies in patients with Crohn's disease in remission. Inflamm Bowel Dis 2006; 12: 185–191.
Lochs H . Enteral nutrition-the new maintenance therapy in Crohn's disease? Inflamm Bowel Dis 2007; 13: 1581–1582.
Yamamoto T, Nakahigashi M, Umegae S, Matsumoto K . Enteral nutrition for the maintenance of remission in Crohn's disease: a systematic review. Eur J Gastroen Hepat 2010; 22: 1–8.
Stephens RV, Randall HT . Use of a concentrated, balanced, liquid elemental diet for nutritional management of catabolic states. Ann Surg 1969; 170: 642–668.
Issa M, Binion DG . Bowel rest and nutrition therapy in the management of active Crohn's disease. Nutr Clin Pract 2008; 23: 299–308.
Meister D, Bode J, Shand A, Ghosh S . Anti-inflammatory effects of enteral diet components on Crohn's disease-affected tissues in vitro. Dig Liver Dis 2002; 34: 430–438.
Iesalnieks I, Dederichs F, Kilger A, Schlitt HJ, Agha A . Postoperative morbidity after bowel resections in patients with Crohn's disease: risk, management strategies, prevention. Z Gastroenterol 2012; 50: 595–600.
Llop JM, Cobo S, Padulles A, Farran L, Jodar R, Badia MB . Nutritional support and risk factors of appearance of enterocutaneous fistulas. Nutr Hosp 2012; 27: 213–218.
Lionetti P, Callegari ML, Ferrari S, Cavicchi MC, Pozzi E, de Martino M et al. Enteral nutrition and microflora in pediatric Crohn's disease. JPEN-Parenter Enteral Nutr 2005; 29: S173–S178.
Nguyen DL, Sandborn WJ, Loftus EV Jr., Larson DW, Fletcher JG, Becker B et al. Similar outcomes of surgical and medical treatment of intra-abdominal abscesses in patients with Crohn's disease. Clin Gastroenterol Hepatol 2012; 10: 400–404.
Yamazaki Y, Fukushima T, Sugita A, Takemura H, Tsuchiya S . The medical, nutritional and surgical treatment of fistulae in Crohn's disease. Surg Today 1990; 20: 376–383.
Riordan AM, Hunter JO, Cowan RE, Crampton JR, Davidson AR, Dickinson RJ et al. Treatment of active Crohn's disease by exclusion diet: East Anglian multicentre controlled trial. Lancet 1993; 342: 1131–1134.
Sartor RB . Mechanisms of disease: pathogenesis of Crohn's disease and ulcerative colitis. Nat Clin Pract Gastroenterol Hepatol 2006; 3: 390.
Scholz D . The role of nutrition in the etiology of inflammatory bowel disease. Curr Probl Pediatr Adolesc Health Care 2011; 41: 248–253.
Lochs H . Basics in clinical nutrition: nutritional support in inflammatory bowel disease. e-SPENJ 2010; 5: e100–e103.
de Jong NSH, Leach ST, Day AS . Polymeric formula has direct anti-inflammatory effects on enterocytes in an in vitro model of intestinal inflammation. Diges Dis Sci 2007; 52: 2029–2036.
Leach ST, Mitchell HM, Eng WR, Zhang L, Day AS . Sustained modulation of intestinal bacteria by exclusive enteral nutrition used to treat children with Crohn's disease. Aliment Pharmacol Ther 2008; 28: 724–733.
Fell JM, Paintin M, Arnaud-Battandier F, Beattie RM, Hollis A, Kitching P et al. Mucosal healing and a fall in mucosal pro-inflammatory cytokine mRNA induced by a specific oral polymeric diet in paediatric Crohn's disease. Aliment Pharmacol Ther 2000; 14: 281–289.
Kudsk KA, Wu Y, Fukatsu K, Zarzaur BL, Johnson CD, Wang R et al. Glutamine-enriched total parenteral nutrition maintains intestinal interleukin-4 and mucosal immunoglobulin A levels. JPEN J Parenter Enteral Nutr 2000; 24: 270–274. discussion 274-5.
Guerreiro CS, Ferreira P, Tavares L, Santos PM, Neves M, Brito M et al. Fatty acids, IL6, and TNF alpha polymorphisms: an example of nutrigenetics in Crohn's Disease. Am J Gastroenterol 2009; 104: 2241–2249.
Danese S, de la Motte C, Fiocchi C . Platelets in inflammatory bowel disease: clinical, pathogenic, and therapeutic implications. Am J Gastroenterol 2004; 99: 938–945.
Ford AC, Kane SV, Khan KJ, Achkar JP, Talley NJ, Marshall JK et al. Efficacy of 5-aminosalicylates in Crohn's disease: systematic review and meta-analysis. Am J Gastroenterol 2011; 106: 617–629.
Khan KJ, Dubinsky MC, Ford AC, Ullman TA, Talley NJ, Moayyedi P . Efficacy of immunosuppressive therapy for inflammatory bowel disease: a systematic review and meta-analysis. Am J Gastroenterol 2011; 106: 630–642.
Lochs H, Dejong C, Hammarqvist F, Hebuterne X, Leon-Sanz M, Schutz T et al. ESPEN guidelines on enteral nutrition: gastroenterology. Clin Nutr 2006; 25: 260–274.
Vagianos K, Bector S, McConnell J, Bernstein CN . Nutrition assessment of patients with inflammatory bowel disease. JPEN J Parenter Enteral Nutr 2007; 31: 311–319.
Schreiber S, Wedel S . Diagnosis and treatment of anemia in inflammatory bowel disease. Inflamm Bowel Dis 1997; 3: 204–216.
Ganz T . Hepcidin, a key regulator of iron metabolism and mediator of anemia of inflammation. Blood 2003; 102: 783–788.
Stein J, Hartmann F, Dignass AU . Diagnosis and management of iron deficiency anemia in patients with IBD. Nat Rev Gastro Hepat 2010; 7: 599–610.
Yamamoto T, Nakahigashi M, Umegae S, Kitagawa T, Matsumoto K . Impact of elemental diet on mucosal inflammation in patients with active Crohn's disease: cytokine production and endoscopic and histological findings. Inflamm Bowel Dis 2005; 11: 580–588.
Lynch AC, Delaney CP, Senagore AJ, Connor JT, Remzi FH, Fazio VW . Clinical outcome and factors predictive of recurrence after enterocutaneous fistulasurgery. Ann Surg 2004; 240: 825–831.
Acknowledgements
This work was supported by grants from Advanced Training Program for Research Talents of Jiangsu Province, China (BRA2011232) and National Science Foundation of China (81270478).
DISCLAIMER
The study design and procedures were approved by the Institutional Review Board (IRB) Ethics Committee at Jinling Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Yan, D., Ren, J., Wang, G. et al. Predictors of response to enteral nutrition in abdominal enterocutaneous fistula patients with Crohn's disease. Eur J Clin Nutr 68, 959–963 (2014). https://doi.org/10.1038/ejcn.2014.31
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2014.31
This article is cited by
-
Dietary management of adults with IBD — the emerging role of dietary therapy
Nature Reviews Gastroenterology & Hepatology (2022)
-
Treatment of enterocutaneous fistula: a systematic review and meta-analysis
Techniques in Coloproctology (2022)
-
Diet as Adjunctive Treatment for Inflammatory Bowel Disease: Review and Update of the Latest Literature
Current Treatment Options in Gastroenterology (2019)
-
Diet and inflammatory bowel disease: The Asian Working Group guidelines
Indian Journal of Gastroenterology (2019)