Abstract
Background/Objectives:
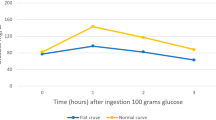
The objective of this study was to examine the relationship between upper distribution levels of glucose values in the 75 -g oral glucose tolerance test (OGTT) and recommended diagnostic criteria for gestational diabetes mellitus (GDM) and adverse pregnancy outcomes.
Subjects/Methods:
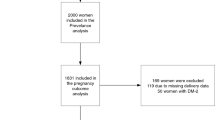
The distribution of the OGTT 2-h values of 13 501 pregnant women, which were below the World Health Organization (WHO) threshold for overt diabetes mellitus (DM), and managed in one teaching hospital in China, was reviewed and related to maternal characteristics and pregnancy outcomes.
Results:
For the entire group, the 90th and 95th percentile values of the OGTT 2-h glucose level, respectively, were close to the diagnostic cutoff values of the WHO and International Association of Diabetes and Pregnancy Study Groups (IADPSG) criteria. For adverse maternal outcomes, glucose level above the 90th percentile value was associated with increased hypertensive disorders, whereas no difference was seen with cutoff using the 95th percentile value. For perinatal outcomes, the 90th percentile was associated with increased neonatal intensive care unit admission and hypoglycemia, whereas the 95th percentile showed in addition association with phototherapy for jaundice and 5th-minute Apgar score <7. Although no differences in the incidence of adverse pregnancy outcomes were found using the different cutoffs, the >95th percentile cutoff value would have missed out 33.3–56.7% of the cases of adverse outcomes that would otherwise have been attributed to GDM.
Conclusions:
Further studies are warranted to clarify which diagnostic criterion is most appropriate universally to identify adverse pregnancy outcomes attributed to GDM, and which could be mitigated with treatment specific for GDM.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
HAPO Study Cooperative Research Group. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 2008; 358: 1991–2002.
International Association of Diabetes and Pregnancy Study Groups Consensus Panel. International association of diabetes and pregnancy study groups recommendations on the diagnostic and classification of hyperglycemia in pregnancy. Diabetes Care 2010; 33: 676–682.
Morikawa M, Yamada T, Yamada T, Akaishi R, Nishida R, Cho K et al. Change in the number of patients after the adoption of IADPSG criteria for hyperglycemia during pregnancy in Japanese women. Diabetes Res Clin Pract 2010; 90: 339–342.
Ohno MS, Sparks TN, Cheng YW, Caughey AB . Treating mild gestational diabetes mellitus: a cost-effectiveness analysis. Am J Obstet Gynecol 2011; 205: e1–e7.
Diagnostic criteria and classification of hyperglycaemia first detected in pregnancy. World Health Organization: Geneva, 2013.
Langer O, Umans JG, Miodovnik M . The proposed GDM diagnostic criteria: a difference, to be a difference, must make a difference. J Matern Fetal Neonatal Med 2013; 26: 111–115.
Huynh J, Ratnaike S, Bartalotta C . Challenging the glucose challenge test. Aust NZ J ObstetGynaecol 2011; 51: 22–25.
O'Sullivan EP, Avalos G, O'Reilly M, Dennedy MC, Gaffney G, Dunne F . Atlantic DIP collaborators. Atlantic Diabetes in Pregnancy (DIP): the prevalence and outcomes of gestational diabetes mellitus using new diagnostic criteria. Diabetologia 2011; 54: 1670–1675.
American College of Obstetrics and Gynecology. Committee opinion number 504: screening and diagnosis of gestational diabetes mellitus. Obstet Gynecol 2011; 118: 751–753.
Vandorsten JP, Dodson WC, Espeland MA, Grobman WA, Guise JM, Mercer BM et al. NIH Consensus Development Conference: Diagnosing gestational diabetes mellitus. NIH Consens State Sci Statements 2013 6 29: 1–31.
Mcintyre HD . Diagnosing gestational diabetes mellitus: rationed or rationally related to risk? Diabetes Care 2013; 36: 2879–2880.
Reece EA, Moore T . The diagnostic criteria for gestational diabetes: to change or not to change? Am J Obstet Gynecol 2013; 208: 255–259.
The WHO Consultation The WHO Consultation, Alberti KGMM, Zimmet PZ . Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus. Report of a WHO consultation. Diabetic Med 1999; 15: 539–553.
WHO study group. Diabetes mellitus: report of a WHO study group. World Health Organ Tech Rep Ser 1985; 727: 1–113.
Deerochanawong C, Putiyanun C, Wongsuryrat M, Serirat S, Jinayon P . Comparison of national diabetes data group and World Health Organization criteria for detecting gestational diabetes mellitus. Diabetologia 1996; 39: 1070–1073.
Li DFH, Wong VCW O, Hoy RM, Ma HK . Evaluation of the WHO criteria for 75 g oral glucose tolerance test in pregnancy. Br J Obstet Gynecol 1987; 94: 847–850.
de Sereday MS, González CD, Bennett PH . Diagnostic criteria for gestational diabetes in relation to pregnancy outcome. J Diabetes Complications 2003; 17: 115–119.
Gayle C, Germain S, Marsh MS, Rajasingham D, Brackenridge A, Carroll P et al. Comparing pregnancy outcomes for intensive versus routine antenatal treatment of GDM based on a 75gm OGTT 2-h blood glucose(>140 mg/dl). Diabetologia 2010; 53: S435.
Wahi P, Dogra V, Jandial K, Bhagat R, Gupta S, Gupta S et al. Prevalence of gestational diabetes mellitus (GDM) and its outcomes in Jammu Region. J Assoc Physicians India 2011; 59: 227–230.
Lao TT, Lee CP . Gestational 'impaired glucose tolerance': should the cut-off be raised to 9 mmoll(−1)? Diabet Med 1998; 15: 25–29.
Wendland EM, Torloni MR, Falavigna M, Trujillo J, Dode MA, Campos MA et al. Gestational diabetes and pregnancy outcomes– a systematic review of the World Health Organization (WHO) and the International Association of Diabetes in Pregnancy Study Groups (IADPSG) diagnostic criteria. BMC Pregnancy and Childbirth 2012; 12: 23–35.
Nallaperumal S, Bhavadharini B, Mahalakshmi MM, Maheswari K, Jalaja R, Moses A et al. Comparison of the World Health Organization and the International Association of Diabetes and Pregnancy Study Groups criteria in diagnosing gestational diabetes mellitus in South Indians. Indian J Endocrinol Metab 2013; 17: 906–909.
Ma RM, Lao TT, Sun YH, Du MY, Yuqin T, Bailuan L et al. Practice audits to reduce caesareans in a tertiary referral hospital in south-western China. Bull World Health Organ 2012; 90: 488–494.
Ma RM, Lao TT, Ma CL, Liao SJ, Lu YF, Du MY et al. Relationship between leg length and gestational diabetes mellitus in Chinese pregnant women. Diabetes Care 2007; 30: 2960–2961.
National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy. Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy. Am J Obstet Gynecol 2000; 183: S1–S22.
Zhang Y, Ma RM, Wang J, Yin R, Sun Q, Sun YH et al. Birth weight percentile in normal singleton pregnancy in Kunming City. Prog Obstet Gynecol (Chinese) 2010; 19: 99–103.
Landon MB, Spong CY, Thom E, Carpenter MW, Ramin SM, Casey B et al. A multicenter, randomized trial of treatment for mild gestational diabetes. N Engl J Med. MFMU study–a large randomized controlled trial of the treatment of mild GDM 2009; V361N14: 1339–1348.
Crowther CA, Hiller JE, Moss JR, Mcphee AJ, Jeffries WS, Robinson JS . Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med. ACHOIS—a large randomized controlled trial of the treatment of mild GDM 2005; 352: 2477–2486.
Capenter MW . Gestational diabetes, pregnancy hypertention, and late vascular disease. Diabetes Care 2007; 30: S246–S250.
Zhu WW, Yang HX, Wei YM, Yan J, Wang ZL, Li XL et al. Evaluation of the value of fasting plasma glucose in the first prenatal visit to diagnose gestational diabetes mellitus in china. Diabetes Care 2013; 36: 586–590.
Acknowledgements
This project was financially supported by three research grants from the China National Natural Science Funds (No. 81160082), the Yunnan Science and Technology Committee (No. 2009CA006) and National Major Specialty Developmental Program.
Author Contributions
MYD researched the data and wrote the manuscript; RMM researched the data, and wrote and reviewed the manuscript; TTL researched the data and reviewed/edited the manuscript; ZC, HX, YQT, BLL, KL, LZ, MHY, JL, HL, RY, LG, WJQ, HYL, JX, SQH, GHL and JHY researched the data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Du, M., Ma, R., Lao, TH. et al. Early third trimester maternal response to glucose challenge and pregnancy outcome in Chinese women—relationship between upper distribution level and recommended diagnostic criteria. Eur J Clin Nutr 69, 1133–1139 (2015). https://doi.org/10.1038/ejcn.2014.293
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2014.293
This article is cited by
-
Gestational weight gain targets during the second and third trimesters of pregnancy for women with gestational diabetes mellitus in China
European Journal of Clinical Nutrition (2019)
-
Factors associated with recovery from 1 minute Apgar score <4 in live, singleton, term births: an analysis of Malaysian National Obstetrics Registry data 2010–2012
BMC Pregnancy and Childbirth (2017)