Abstract
Background/Objectives:
This investigation evaluated 12 hydration biomarkers, to determine which represent 24-h whole-body water balance (that is, measured as water retention or clearance (WR-C) by the kidneys).
Subjects/Methods:
Healthy males (n=59; body mass, 75.1±7.9 kg; height, 178±6 cm; age, 22±3 years; body mass index, 23.9±2.4 kg/m2) met with a registered dietitian each morning (days 1–11) to optimize completeness and accuracy of food and fluid records, then went about ordinary daily activities. These men visited the laboratory for blood samples and collected all urine produced on days 1, 3, 6, 9 and 12. The reference standard (WR-C) was calculated using 24-h urine volume, 24-h urine osmolality, and serum osmolality (single morning venous sample).
Results:
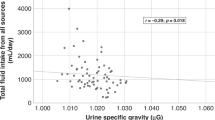
Statistical regression analyses indicated that, among the 12 hydration biomarkers, only 24-h urine osmolality (r2=0.60, P<0.0001) and 24-h urine specific gravity (r2=0.52, P<0.0001) strongly predicted WR-C. The 24-h fluid intake, 24-h body mass change, 24-h urine color and 24-h urine volume were weak (P>0.05) predictors of WR-C, similar to serum osmolality and other single measurements (range of r2 values, 0.19–0.0001).
Conclusions:
These observations of healthy, active young men demonstrate that WR-C is strongly related to the 24-h concentration of urine, which in turn reflects the excretion of total solids in the diet. Although morning urine assessments provided information about a single time point, 24-h urine osmolality and 24-h urine specific gravity were the best predictors of 24-h body water balance.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Ganio MS, Armstrong LE, Casa DJ, McDermott BP, Lee EC, Yamamoto LM et al. Mild dehydration impairs cognitive performance and mood of men. Brit J Nutr 2011; 106: 1535–1543.
Armstrong LE, Ganio MS, Casa DJ, Lee EC, McDermott BP, Klau JF et al. Mild dehydration affects mood in healthy young women. J Nutr 2012; 142: 382–388.
Armstrong LE . Assessing hydration status: the elusive gold standard. J Am Coll Nutr 2007; 26: 575S–584S.
Opplinger RA, Bartok C . Hydration testing of athletes. Sports Med 2002; 32: 959–971.
Shirreffs S, Maughan R . Urine osmolality and conductivity as indices of hydration status in athletes in the heat. Med Sci Sports Exerc 1998; 30: 1598–1602.
Shore AC, Markandu ND, Sagnella GA, Singer DR, Forsling ML, Buckley MG et al. Endocrine and renal response to water loading and water restriction in normal man. Clin Sci 1988; 75: 171–177.
Casa DJ, Armstrong LE, Hillman SK, Montain SJ, Reiff RV, Rich BS et al. National athletic trainers’ association position statement: fluid replacement for athletes. J Ath Train 2000; 35: 212–224.
Kavouras S . Assessing hydration status. Cur Opin Clin Nutr Metab Care 2000; 5: 519–524.
Manz F, Wentz A, Sichert-Hellert W . The most essential nutrient: defining the adequate intake of water. J Pediatr 2002; 141: 587–592.
Cheuvront SN, Sawka MN . Hydration assessment of athletes. In: Sports Sci Exchange. Gatorade Sports Science Institute: Barrington, IL, 2005.
Armstrong LE, Pumerantz AC, Roti MW, Judelson DA, Watson G, Dias JC et al. Fluid, electrolyte, and renal indices of hydration during 11 days of controlled caffeine consumption. Int J Sport Nutr Exerc Metab 2005; 15: 252–265.
Armstrong LE, Pumerantz AC, Fiala KA, Roti MW, Kavouras SA, Casa DJ et al. Human hydration indices: acute and longitudinal reference values. Int J Sport Nutr Exerc Metab 2010; 20: 145–153.
Armstrong LE, Johnson EC, Munoz CX, Swokla B, Le Bellego L, Jimenez L et al. Hydration biomarkers and dietary fluid consumption of women. J Acad Nutr Diet 2012; 112: 1056–1061.
Armstrong LE, Maresh CM, Castellani J, Bergeron M, Kenefick RW, LaGasse KE et al. Urinary indices of hydration status. Int J Sport Nutr Exerc Metab 1994; 4: 265–279.
Elorza MA, Garcia A, Fuster A, Muller A . Evaluation of the Auto-Stat 601" Automatic Osmometer and Its Comparison with the Digimatic-Advanced 3DII Manual Osmometer. Eur J Clin Chem Clin Biochem 1993; 31: 245–249.
Ganong WF . Regulation of extracellular fluid composition and volume. In: Review of Medical Physiology 19th edn. Appleton & Lange Co: Stamford, CT, 1999.
Guyton AC, Hall JE . Regulation of extracellular fluid osmolarity and sodium concentration. In: Textbook of Medical Physiology 9th edn. W.B. Saunders Co: Philadelphia, 1996.
Kratz A, Ferraro M, Sluss PM, Lewandrowski KB . Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Laboratory reference values. New Engl J Med 2004; 351: 1548–1563.
Greenleaf JE . Problem. Thirst, drinking behavior, and involuntary dehydration. Med Sci Sports Exerc 1992; 24: 645–656.
Tack I . Effects of water consumption on kidney function and excretion. Nutr Today 2010; 45 (Supplement 6), S1–S4.
Strippoli GFM, Craig JC, Rochtchina E, Flood VM, Wang JJ, Mitchell P . Fluid and nutrient intake and risk of chronic kidney disease. Nephrology 2011; 16: 326–334.
Sawka MN, Burke LM, Eichner ER, Maughan RJ, Montain SJ, Stachenfeld NS . American College of Sports Medicine position stand. Exercise and fluid replacement. Med Sci Sports Exerc 2007; 39: 377–390.
Manz F, Wentz A . 24-h hydration status: parameters, epidemiology and recommendations. Eur J Clin Nutr 2003; 57 (Suppl 2), S10–S18.
Institute of Medicine, National Academy of Sciences. Dietary reference intakes: water, potassium, sodium, chloride, and sulfate. National Academy Press: Washington, D.C., 2004.
de Castro JM . The relationship of spontaneous macronutrient and sodium intake with fluid ingestion and thirst in humans. Physiol Behav 1991; 49: 513–519.
Bossingham MJ, Carnell NS, Campbell W . Water balance, hydration status, and fat-free mass hydration in younger and older adults. Am J Clin Nutr 2005; 81: 1342–1350.
European Food Safety Authority. Scientific opinion on dietary reference values for water. EFSA J 2010; 8: 1459–1469.
Perrier E, Klein A, Poupin M, Pascale R, LeBellego L, Armstrong L et al. Hydration biomarkers in free-living adults with different levels of habitual fluid consumption. Brit J Nutr 2012; 31: 1–10.
Perucca J, Bouby N, Valeix P, Bankir L . Sex differences in urine concentration across differing ages, sodium intake, and level of kidney disease. Am J Physiol Regul Integr Comp Physiol 2007; 292: R700–R705.
Acknowledgements
This work was funded, in part, by the International Life Sciences Institute North America (ILSI NA), Washington, DC.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Professor Armstrong has received compensation as a consultant to ILSI NA and to Danone Research, Palaiseau France; he serves as a Scientific Advisory Board and Expert Working Group member for the Hydration for Health Initiative of Danone Research. The remaining authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Armstrong, L., Johnson, E., McKenzie, A. et al. Interpreting common hydration biomarkers on the basis of solute and water excretion. Eur J Clin Nutr 67, 249–253 (2013). https://doi.org/10.1038/ejcn.2012.214
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2012.214
Keywords
This article is cited by
-
Daily water regime and sample sampling affect blood and urine parameter value change in healthy individuals
The Journal of Basic and Applied Zoology (2021)
-
Effect of increased water intake on plasma copeptin in healthy adults
European Journal of Nutrition (2018)