Abstract
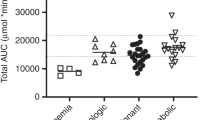
Busulfan, the corner stone of hematopoietic stem cell transplantation regimens, has a narrow therapeutic window. Therapeutic drug monitoring (TDM)-guided dosing to reach the conventional area under the concentration–time curve (AUC) target range of 900–1500 μmol min/L is associated with better outcomes. We report our experience with busulfan TDM in a large cohort of children. The aims were to investigate the relevance of using a more restricted therapeutic range and investigate the association between busulfan therapeutic range and clinical outcome. This study includes 138 children receiving 16 doses of intravenous busulfan, with the first dose assigned based on weight and doses adjusted to a local AUC target range of 980–1250 μmol min/L. Busulfan TDM combined with model-based dose adjustment was associated with an increased probability of AUC target attainment, for both target range: 90.8% versus 74.8% for the conventional target range and 66.2% versus 43.9% for the local target range (P<0.001). The median follow-up was 56.2 months. Event-free survival was 88.5%, overall survival was 91.5% and veno-occlusive disease occurred in 18.3% of patients. No difference was observed for clinical outcomes depending on the selected target range. Pharmacokinetic monitoring and individualization of busulfan dosage regimen are useful in improving target attainment, but using a restricted target range has no impact on clinical outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Santos GW, Tutschka PJ, Brookmeyer R, Saral R, Beschorner WE, Bias WB et al. Marrow transplantation for acute nonlymphocytic leukemia after treatment with busulfan and cyclophosphamide. N Engl J Med 1983; 309: 1347–1353.
Schuler US, Renner UD, Kroschinsky F, Johne C, Jenke A, Naumann R et al. Intravenous busulphan for conditioning before autologous or allogeneic human blood stem cell transplantation. Br J Haematol 2001; 114: 944–950.
Cohen A, Békássy AN, Gaiero A, Faraci M, Zecca S, Tichelli A et al. Endocrinological late complications after hematopoietic SCT in children. Bone Marrow Transplant 2008; 41: S43–S48.
Faraci M, Barra S, Cohen A, Lanino E, Grisolia F, Miano M et al. Very late nonfatal consequences of fractionated TBI in children undergoing bone marrow transplant. Int J Radiat Oncol Biol Phys 2005; 63: 1568–1575.
Faraci M, Békássy AN, De Fazio V, Tichelli A, Dini G, EBMT Paediatric and Late Effects Working Parties. Non-endocrine late complications in children after allogeneic haematopoietic SCT. Bone Marrow Transplant 2008; 41: S49–S57.
McCune JS, Gooley T, Gibbs JP, Sanders JE, Petersdorf EW, Appelbaum FR et al. Busulfan concentration and graft rejection in pediatric patients undergoing hematopoietic stem cell transplantation. Bone Marrow Transplant 2002; 30: 167–173.
Slattery JT, Sanders JE, Buckner CD, Schaffer RL, Lambert KW, Langer FP et al. Graft-rejection and toxicity following bone marrow transplantation in relation to busulfan pharmacokinetics. Bone Marrow Transplant 1995; 16: 31–42.
Copelan EA, Bechtel TP, Avalos BR, Elder PJ, Ezzone SA, Scholl MD et al. Busulfan levels are influenced by prior treatment and are associated with hepatic veno-occlusive disease and early mortality but not with delayed complications following marrow transplantation. Bone Marrow Transplant 2001; 27: 1121–1124.
Grochow LB, Jones RJ, Brundrett RB, Braine HG, Chen TL, Saral R et al. Pharmacokinetics of busulfan: correlation with veno-occlusive disease in patients undergoing bone marrow transplantation. Cancer Chemother Pharmacol 1989; 25: 55–61.
Dix SP, Wingard JR, Mullins RE, Jerkunica I, Davidson TG, Gilmore CE et al. Association of busulfan area under the curve with veno-occlusive disease following BMT. Bone Marrow Transplant 1996; 17: 225–230.
Bleyzac N, Souillet G, Magron P, Janoly A, Martin P, Bertrand Y et al. Improved clinical outcome of paediatric bone marrow recipients using a test dose and Bayesian pharmacokinetic individualization of busulfan dosage regimens. Bone Marrow Transplant 2001; 28: 743–751.
De Lima M, Couriel D, Thall PF, Wang X, Madden T, Jones R et al. Once-daily intravenous busulfan and fludarabine: clinical and pharmacokinetic results of a myeloablative, reduced-toxicity conditioning regimen for allogeneic stem cell transplantation in AML and MDS. Blood 2004; 104: 857–864.
Geddes M, Kangarloo SB, Naveed F, Quinlan D, Chaudhry MA, Stewart D et al. High busulfan exposure is associated with worse outcomes in a daily i.v. busulfan and fludarabine allogeneic transplant regimen. Biol Blood Marrow Transplant 2008; 14: 220–228.
Hassan M, Ljungman P, Bolme P, Ringdén O, Syrůcková Z, Békàssy A et al. Busulfan bioavailability. Blood 1994; 84: 2144–2150.
Andersson BS, Thall PF, Madden T, Couriel D, Wang X, Tran HT et al. Busulfan systemic exposure relative to regimen-related toxicity and acute graft-versus-host disease: defining a therapeutic window for i.v. BuCy2 in chronic myelogenous leukemia. Biol Blood Marrow Transplant 2002; 8: 477–485.
Cremers S, Schoemaker R, Bredius R, den Hartigh J, Ball L, Twiss I et al. Pharmacokinetics of intravenous busulfan in children prior to stem cell transplantation. Br J Clin Pharmacol 2002; 53: 386–389.
Tran H, Petropoulos D, Worth L, Mullen CA, Madden T, Andersson B et al. Pharmacokinetics and individualized dose adjustment of intravenous busulfan in children with advanced hematologic malignancies undergoing allogeneic stem cell transplantation. Biol Blood Marrow Transplant 2004; 10: 805–812.
Nguyen L, Fuller D, Lennon S, Leger F, Puozzo C . I.V.busulfan in pediatrics: a novel dosing to improve safety/efficacy for hematopoietic progenitor cell transplantation recipients. Bone Marrow Transplant 2004; 33: 979–987.
Vassal G, Michel G, Espérou H, Gentet JC, Valteau-Couanet D, Doz F et al. Prospective validation of a novel IV busulfan fixed dosing for paediatric patients to improve therapeutic AUC targeting without drug monitoring. Cancer Chemother Pharmacol 2008; 61: 113–123.
Zwaveling J, Bredius RGM, Cremers SCLM, Ball LM, Lankester AC, Teepe-Twiss IM et al. Intravenous busulfan in children prior to stem cell transplantation: study of pharmacokinetics in association with early clinical outcome and toxicity. Bone Marrow Transplant 2005; 35: 17–23.
Malär R, Sjöö F, Rentsch K, Hassan M, Güngör T . Therapeutic drug monitoring is essential for intravenous busulfan therapy in pediatric hematopoietic stem cell recipients. Pediatr Transplant 2011; 15: 580–588.
Michel G, Valteau-Couanet D, Gentet J-C, Esperou H, Socié G, Méchinaud F et al. Weight-based strategy of dose administration in children using intravenous busulfan: Clinical and pharmacokinetic results. Pediatr Blood Cancer 2012; 58: 90–97.
Tesfaye H, Branova R, Klapkova E, Prusa R, Janeckova D, Riha P et al. The importance of therapeutic drug monitoring (TDM) for parenteral busulfan dosing in conditioning regimen for hematopoietic stem cell transplantation (HSCT) in children. Ann Transplant 2014; 19: 214–224.
Dignan FL, Wynn RF, Hadzic N, Karani J, Quaglia A, Pagliuca A et al. BCSH/BSBMT guideline: diagnosis and management of veno-occlusive disease (sinusoidal obstruction syndrome) following haematopoietic stem cell transplantation. Br J Haematol 2013; 163: 444–457.
Bleyzac N, Barou P, Aulagner G . Rapid and sensitive high-performance liquid chromatographic method for busulfan assay in plasma. J Chromatogr B Biomed Sci Appl 2000; 742: 427–432.
Dos Reis EO, Vianna-Jorge R, Suarez-Kurtz G, Lima EL, da S, Azevedo D de A . Development of a rapid and specific assay for detection of busulfan in human plasma by high-performance liquid chromatography/electrospray ionization tandem mass spectrometry. Rapid Commun Mass Spectrom 2005; 19: 1666–1674.
D’Argenio DZ . Optimal sampling times for pharmacokinetic experiments. J Pharmacokinet Biopharm 1981; 9: 739–756.
Bertholle-Bonnet V, Bleyzac N, Galambrun C, Mialou V, Bertrand Y, Souillet G et al. Influence of underlying disease on busulfan disposition in pediatric bone marrow transplant recipients: a nonparametric population pharmacokinetic study. Ther Drug Monit 2007; 29: 177–184.
Jelliffe RW . The USC*PACK PC programs for population pharmacokinetic modeling, modeling of large kinetic/dynamic systems, and adaptive control of drug dosage regimens. Proc Annu Symp Comput Appl Med Care 1991: 922–924.
Tran HT, Madden T, Petropoulos D, Worth LL, Felix EA, Sprigg-Saenz HA et al. Individualizing high-dose oral busulfan: prospective dose adjustment in a pediatric population undergoing allogeneic stem cell transplantation for advanced hematologic malignancies. Bone Marrow Transplant 2000; 26: 463–470.
Galambrun C, Pondarré C, Bertrand Y, Loundou A, Bordigoni P, Frange P et al. French multicenter 22-year experience in stem cell transplantation for beta-thalassemia major: lessons and future directions. Biol Blood Marrow Transplant 2013; 19: 62–68.
McDonald GB, Hinds MS, Fisher LD, Schoch HG, Wolford JL, Banaji M et al. Veno-occlusive disease of the liver and multiorgan failure after bone marrow transplantation: a cohort study of 355 patients. Ann Intern Med 1993; 118: 255–267.
Bearman SI . The syndrome of hepatic veno-occlusive disease after marrow transplantation. Blood 1995; 85: 3005–3020.
Nath CE, Shaw PJ . Busulphan in blood and marrow transplantation: dose, route, frequency and role of therapeutic drug monitoring. Curr Clin Pharmacol 2007; 2: 75–91.
Schechter T, Finkelstein Y, Doyle J, Verjee Z, Moretti M, Koren G et al. Pharmacokinetic disposition and clinical outcomes in infants and children receiving intravenous busulfan for allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 2007; 13: 307–314.
Zwaveling J, den Hartigh J, Lankester AC, Guchelaar H-J, Egeler RM, Bredius RG et al. Once-daily intravenous busulfan in children prior to stem cell transplantation: study of pharmacokinetics and early clinical outcomes. Anticancer Drugs 2006; 17: 1099–1105.
Ljungman P, Hassan M, Békássy AN, Ringdén O, Oberg G . High busulfan concentrations are associated with increased transplant-related mortality in allogeneic bone marrow transplant patients. Bone Marrow Transplant 1997; 20: 909–913.
Paci A, Vassal G, Moshous D, Dalle J-H, Bleyzac N, Neven B et al. Pharmacokinetic behavior and appraisal of intravenous busulfan dosing in infants and older children: the results of a population pharmacokinetic study from a large pediatric cohort undergoing hematopoietic stem-cell transplantation. Ther Drug Monit 2012; 34: 198–208.
Okamoto Y, Nagatoshi Y, Kosaka Y, Kikuchi A, Kato S, Kigasawa H et al. Prospective pharmacokinetic study of intravenous busulfan in hematopoietic stem cell transplantation in 25 children. Pediatr Transplant 2014; 18: 294–301.
Bartelink IH, Bredius RGM, Belitser SV, Suttorp MM, Bierings M, Knibbe CAJ et al. Association between busulfan exposure and outcome in children receiving intravenous busulfan before hematologic stem cell transplantation. Biol Blood Marrow Transplant 2009; 15: 231–241.
Buffery PJ, Allen KM, Chin PKL, Moore GA, Barclay ML, Begg EJ . Thirteen years’ experience of pharmacokinetic monitoring and dosing of busulfan: can the strategy be improved? Ther Drug Monit 2014; 36: 86–92.
Ansari M, Théoret Y, Rezgui MA, Peters C, Mezziani S, Desjean C et al. Association between busulfan exposure and outcome in children receiving intravenous busulfan before hematopoietic stem cell transplantation. Ther Drug Monit 2014; 36: 93–99.
Wall DA, Chan KW, Nieder ML, Hayashi RJ, Yeager AM, Kadota R et al. Safety, efficacy, and pharmacokinetics of intravenous busulfan in children undergoing allogeneic hematopoietic stem cell transplantation. Pediatr Blood Cancer 2010; 54: 291–298.
Cesaro S, Pillon M, Talenti E, Toffolutti T, Calore E, Tridello G et al. A prospective survey on incidence, risk factors and therapy of hepatic veno-occlusive disease in children after hematopoietic stem cell transplantation. Haematologica 2005; 90: 1396–1404.
Cheuk DKL, Wang P, Lee TL, Chiang AKS, Ha SY, Lau YL et al. Risk factors and mortality predictors of hepatic veno-occlusive disease after pediatric hematopoietic stem cell transplantation. Bone Marrow Transplant 2007; 40: 935–944.
Kearns GL, Abdel-Rahman SM, Alander SW, Blowey DL, Leeder JS, Kauffman RE . Developmental pharmacology—drug disposition, action, and therapy in infants and children. N Engl J Med 2003; 349: 1157–1167.
Hines RN . The ontogeny of drug metabolism enzymes and implications for adverse drug events. Pharmacol Ther 2008; 118: 250–267.
Kim AH, Tse JC, Ikeda A, Moore TB . Evaluating pharmacokinetics and pharmacodynamics of intravenous busulfan in pediatric patients receiving bone marrow transplantation. Pediatr Transplant 2009; 13: 971–976.
Gibbs JP, Murray G, Risler L, Chien JY, Dev R, Slattery JT . Age-dependent tetrahydrothiophenium ion formation in young children and adults receiving high-dose busulfan. Cancer Res 1997; 57: 5509–5516.
Savic RM, Cowan MJ, Dvorak CC, Pai S-Y, Pereira L, Bartelink IH et al. Effect of weight and maturation on busulfan clearance in infants and small children undergoing hematopoietic cell transplantation. Biol Blood Marrow Transplant 2013; 19: 1608–1614.
Gibbs JP, Liacouras CA, Baldassano RN, Slattery JT . Up-regulation of glutathione S-transferase activity in enterocytes of young children. Drug Metab Dispos Biol Fate Chem 1999; 27: 1466–1469.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Philippe, M., Goutelle, S., Guitton, J. et al. Should busulfan therapeutic range be narrowed in pediatrics? Experience from a large cohort of hematopoietic stem cell transplant children. Bone Marrow Transplant 51, 72–78 (2016). https://doi.org/10.1038/bmt.2015.218
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2015.218
This article is cited by
-
Clinical outcomes of individualized busulfan-dosing in hematopoietic stem cell transplantation in Chinese children undergoing with therapeutic drug monitoring
Bone Marrow Transplantation (2022)
-
GSTM1 and GSTT1 double null genotypes determining cell fate and proliferation as potential risk factors of relapse in children with hematological malignancies after hematopoietic stem cell transplantation
Journal of Cancer Research and Clinical Oncology (2022)
-
Evaluation of two software using Bayesian methods for monitoring exposure and dosing once-daily intravenous busulfan in paediatric patients receiving haematopoietic stem cell transplantation
Cancer Chemotherapy and Pharmacology (2021)
-
Review of the Pharmacokinetics and Pharmacodynamics of Intravenous Busulfan in Paediatric Patients
Clinical Pharmacokinetics (2021)
-
Busulfan systemic exposure and its relationship with efficacy and safety in hematopoietic stem cell transplantation in children: a meta-analysis
BMC Pediatrics (2020)