Abstract
Background:
Epidemiological studies evaluating the association of vitamin B6, vitamin B12 and methionine with breast cancer risk have produced inconsistent results.
Methods:
Pertinent studies were identified by a search in PubMed and Web of Knowledge. Random-effect model was used. Dose–response relationship was assessed by restricted cubic spline.
Results:
The combined relative risk (95% confidence interval) of breast cancer for the highest vs lowest category of serum pyridoxal 5′-phosphate (PLP, active form of vitamin B6) levels and dietary methionine intake was 0.80 (0.66–0.98, P=0.03) and 0.94 (0.89–0.99, P=0.03), respectively, and the associations of breast cancer with higher serum PLP levels and dietary methionine intake were significant among post-menopausal women, but not among pre-menopausal women. The inverse association between breast cancer risk and dietary vitamin B6 intake, serum vitamin B12 levels and dietary vitamin B12 intake was not significant overall. Linear dose–response relationship was found, and the risk of breast cancer decreased by 23% (P<0.00) for every 100 pmol ml−1 increment in PLP levels and 4% (P=0.05) for every 1 g per day increment in dietary methionine intake, respectively.
Conclusion:
Serum PLP levels and methionine intake might be inversely associated with breast cancer risk, especially among postmenopausal women, which need to be confirmed.
Similar content being viewed by others
Main
Breast cancer is the most frequently diagnosed types of cancer and the leading cause of cancer death among women worldwide, accounting for 23% of the total cancer cases and 14% of the cancer deaths, and about half the breast cancer cases and 60% of the deaths are estimated to occur in economically developing countries (Jemal et al, 2011). Although incidence rates of breast cancer in some western countries decreased since the beginning of 2000, the incidence rates have been rising in many African and Asian countries (Jemal et al, 2011). According to the American Cancer Society Guidelines, the nutrition- and physical activity-related advice (Wu et al, 2013) is necessary to reduce the risk of breast cancer (Kushi et al, 2012). One-carbon metabolism nutrients, such as folate, vitamin B6, vitamin B12 and methionine, may protect against cancer through DNA synthesis and methylation, upholding DNA integrity and regulating gene expression (Ames, 2001; Selhub, 2002), and pyridoxal 5′-phosphate (PLP; the active form of vitamin B6) is involved in almost 100 enzymatic reactions (Bairoch, 2000). Although no significant effect of folate on breast cancer was found in the previous meta-analysis overall (Larsson et al, 2007), high alcohol (the known antagonist for these B-vitamins) consumption was shown to be associated with increased risk of breast cancer (Suzuki et al, 2008). However, results from observational studies on vitamin B6, vitamin B12 and methionine and breast cancer risk are not consistent, and no meta-analysis is available. In addition, folate, vitamin B6 and vitamin B12 act in concert to affect the pathways of one-carbon metabolism (Kim, 2007), and these nutrient interactions were also proposed (Davis and Uthus, 2004). Therefore, we conducted a meta-analysis to (1) first assess the breast cancer risk for the highest vs lowest categories of vitamin B6, vitamin B12 and methionine; (2) then evaluate the possible dose–response relationship of vitamin B6, vitamin B12 and methionine with breast cancer risk; (3) investigate the joint association between folate intake with vitamin B6, vitamin B12 and methionine intake, and the risk of breast cancer; (4) evaluate the modification of key covariates to the association of vitamin B6, vitamin B12 and methionine with breast cancer risk; (5) and assess the heterogeneity among studies and publication bias.
Materials and methods
Literature search and selection
We performed a literature search up to 18 June 2013 using the databases of Pubmed and Web of Knowledge, using the following search terms vitamin B6 or pyridoxal 5'-phosphate (PLP; the active form of vitamin B6), or vitamin B12 or methionine, and breast cancer without restrictions. Moreover, we reviewed the reference lists from retrieved articles to search for further relevant studies.
Two investigators independently reviewed all identified studies, and studies were included if they met the following criteria: (1) the exposure of interest was vitamin B6 or PLP, or vitamin B12 or methionine; (2) the outcome of interest was breast cancer; (3) relative risk (RR) or odds ratio with 95% confidence interval (CI) was provided (we presented all results with RR for simplicity); (4) for dose–response analysis, the number of cases and participants or person-years for each category of vitamin B6 or PLP, or vitamin B12 or methionine, must also be provided (or data available to calculate them). If data were duplicated in more than one study, we included the study with the largest number of cases.
Data extraction
The following data were extracted from each study by two investigators: the design type (case–control or prospective study), the first author’s last name, publication year, location where the study was performed, sample size and number of cases, variables adjusted for in the analysis, RR estimates with corresponding 95% CI for the highest versus lowest categories of vitamin B6, vitamin B12 and methionine, respectively. The result for dietary intake of these nutrients was extracted if the result for both dietary intake and total intake (dietary intake plus supplement) were provided. To investigate the joint association between folate intake with vitamin B6, vitamin B12 and methionine intake, and risk of breast cancer, RR was extracted from the group with both the highest folate intake and highest vitamin B6, vitamin B12 or methionine intake group versus the group with both the lowest folate intake and lowest vitamin B6, vitamin B12 or methionine intake.
For dose–response analysis, the number of cases and participants (person-years), and RR (95% CI) for each category of vitamin B6, vitamin B12 and methionine were also extracted. The median or mean level of vitamin B6, vitamin B12 and methionine for each category was assigned to the corresponding RR for every study. If the upper boundary of the highest category was not provided, we assumed that the boundary had the same amplitude as the adjacent category (Larsson et al, 2010; Hong et al, 2012). We extracted the RRs that reflected the greatest degree of control for potential confounders.
Statistical analysis
Pooled measure was calculated as the inverse variance-weighted mean of the logarithm of RR with 95% CI, to assess the strength of association between vitamin B6, vitamin B12 and methionine and the risk of breast cancer. Random-effects model was used to combine study-specific RR (95%CI), which considers both within-study and between-study variation (DerSimonian and Laird, 1986). The I2 was used to assess heterogeneity, and I2 values of 0, 25, 50 and 75% represent no, low, moderate and high heterogeneity (Higgins et al, 2003), respectively. Meta-regression with restricted maximum likelihood estimation was performed to assess the potentially important covariates that might exert substantial impact on between-study heterogeneity (Higgins and Thompson, 2004). A sensitivity analysis was performed with one study removed at a time to assess whether the results could have been affected markedly by a single study. Publication bias was evaluated using the Egger regression asymmetry test (Egger et al, 1997).
For dose–response analysis, a two-stage random-effects dose–response meta-analysis (Orsini et al, 2012) was performed to compute the trend from the correlated log RR estimates across levels of vitamin B6, vitamin B12 and methionine, respectively, taking into account the between-study heterogeneity. In the first stage, a restricted cubic spline model with three knots at the 25th, 50th and 75th percentiles (Harrell et al, 1988) of the levels of vitamin B6, vitamin B12 and methionine was estimated using generalised least-square regression, taking into account the correlation within each set of published RRs (Orsini and Bellocco, 2006). Then the study-specific estimates were combined using the restricted maximum likelihood method in a multivariate random-effects meta-analysis (Jackson et al, 2010). A P-value for non-linearity was calculated by testing the null hypothesis that the coefficient of the second spline is equal to 0. All statistical analyses were performed with STATA version 12.0 (Stata Corporation, College Station, TX, USA). All reported probabilities (P-values) were two-sided with P<0.05 considered statistically significant.
Results
Literature search and study characteristics
The search strategy identified 552 articles from Pubmed and 1144 articles from the Web of Knowledge, and 28 articles were reviewed in full after reviewing the abstract. Two studies that assessed the MTHFR C677T (Maruti et al, 2009a), MTR and MTRR (Shrubsole et al, 2006) polymorphisms and breast cancer by intakes of one-carbon metabolism nutrients were further excluded because of duplicate reports from the same study population. Three studies that did not report the risk estimate were also excluded (Potera et al, 1977; Goodman et al, 2001; Schroecksnadel et al, 2003). Finally, 23 articles (Thorand et al, 1998; Wu et al, 1999a; Levi et al, 2001; Shrubsole et al, 2001; Feigelson et al, 2003; Zhang et al, 2003; Zhu et al, 2003; Lajous et al, 2006a; Lajous et al, 2006b; Cho et al, 2007; Kabat et al, 2008; Lin et al, 2008; Xu et al, 2008; Ma et al, 2009a; Ma et al, 2009b; Maruti et al, 2009a; Stevens et al, 2010; Chou et al, 2011; Shrubsole et al, 2011; Zhang et al, 2011; Lurie et al, 2012; Bassett et al, 2013; Yang et al, 2013) were included in this meta-analysis. The detailed steps of our literature search are shown in Supplementary Material.
For PLP levels, data from four nested case–control articles with five studies were used, including 2509 breast cancer cases, and all studies were carried out in the United States. For vitamin B6 intake, data from 14 articles (6 prospective studies and 8 case–control studies) were used, including 14 260 breast cancer cases. Five studies were carried out in the United States, four in China, one in Japan, one in Mexico, one in Switzerland, one in Brazilia and one in Australia. For serum vitamin B12 levels, data from three nested case–control articles with four studies were used, including 1803 breast cancer cases, and all studies were carried out in the United States. For vitamin B12 intake, data from 14 articles (7 prospective studies and 7 case–control studies) were used, including 15 783 breast cancer cases. Five studies were carried out in the United States, four in China, one in Japan, one in Mexico, one in France, one in Brazilia and one in Australia. For methionine, data from 13 articles (7 prospective studies and 6 case–control studies) were used, including 17 060 breast cancer cases. Seven studies were carried out in the United States, three China, one in Canada, one in Germany and one in Australia. The detailed characteristics of the studies are shown in Tables 1, 2, 3.
Quantitative synthesis
The main results are summarised in Table 4 (the result by adjustment of selected covariates is not included).
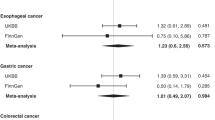
Serum PLP levels and risk of breast cancer
High serum PLP levels vs low levels were significantly associated with the risk of breast cancer (0.80 (0.66–0.98), P=0.03, I2=0.30%, Figure 1). The association was significant for post-menopausal women (0.71 (0.57–0.88), P<0.00, I2=0.00%) but not for pre-menopausal women; however, the difference between the two groups was not significant (P=0.26). No significant association was found by oestrogen receptor (ER) and progesterone receptor (PR) status. Among the five nested case–control studies, two studies in one article (Wu et al, 1999a) only adjusted for age, menopausal status and year of blood donation, and a positive but not significant association of serum PLP levels with the risk of breast cancer was found. Three studies (Zhang et al, 2003; Lin et al, 2008; Lurie et al, 2012) adjusted for the most known risk factors of breast cancer, and a significantly combined effect (Zhang et al, 2003; Lin et al, 2008; Lurie et al, 2012) was found (0.76 (0.62–0.94), P=0.01, I2=0.00%).
The multivariate-adjusted risk of breast cancer for the highest vs lowest categories of serum PLP levels and dietary vitamin B6 intake in random-effects model. The size of the grey box is positively proportional to the weight assigned to each study, which is inversely proportional to the s.e. of the RR, and horizontal lines represent the 95% CIs.
For dose–response analysis, data from three studies (Zhang et al, 2003; Lin et al, 2008; Lurie et al, 2012) were used, including 2266 breast cancer cases. We found no evidence of statistically significant departure from linearity (P=0.85). A 100 pmol ml−1 increment in serum PLP level conferred an RR of 0.77 (95% CI=0.69–0.86, P<0.00, Figure 2).
Vitamin B6 intake and risk of breast cancer
High vitamin B6 intake vs low intake was not significantly associated with the risk of breast cancer (0.95 (0.83–1.08), P=0.45, I2=56.2%, Figure 1). And no significant association was found in subgroup analysis by study design (prospective and case–control), menopausal status (pre-menopausal and post-menopausal), geographic region where the study was conducted (America and Asia), ER status and PR status. No significant association was found in the subgroup analysis by adjustment (yes or no) of the known risk factors of breast cancer, including alcohol, smoking, BMI, FHBC, reproductive factors (⩾3), physical activity, energy intake and use of exogenous hormones.
For dose–response analysis, data from eight studies (Lajous et al, 2006a; Lin et al, 2008; Ma et al, 2009a; Ma et al, 2009b; Stevens et al, 2010; Zhang et al, 2011; Bassett et al, 2013; Yang et al, 2013) were used, including 9429 breast cancer cases. We found no evidence of statistically significant departure from linearity (P=0.08). A 1 mg per day increment in vitamin B6 intake conferred an RR of 0.96 (0.89–1.02, P=0.19).
Serum vitamin B12 levels and risk of breast cancer
High serum vitamin B12 levels vs low levels were not significantly associated with the risk of breast cancer (0.73 (0.44–1.22), P=0.23, I2=72.5%, Figure 3), and no significant association was found in the subgroup analysis by menopausal status. Only one study (Lin et al, 2008) provided the association of serum vitamin B12 levels with the risk of breast cancer by ER status and PR status; thus, the subgroup analysis by ER status and PR status was not conducted. Among the four studies included, one study (Lin et al, 2008) adjusted for the most known risk factors of breast cancer, and women in the highest quintile relative to those in the lowest quintile had multivariate RR of 1.29 (0.92–1.82). The result from the other three studies indicated an obvious protection of serum vitamin B12 levels on risk of breast cancer (0.61 (0.41–0.92), P=0.02, I2=22.3%).
The multivariate-adjusted risk of breast cancer for the highest vs lowest categories of serum vitamin B12 levels and dietary vitamin B12 intake in random-effects model. The size of the grey box is positively proportional to the weight assigned to each study, which is inversely proportional to the s.e. of the RR, and horizontal lines represent the 95% CIs.
For the dose–response analysis, data from two studies (Zhang et al, 2003; Lin et al, 2008) were used, including 1560 breast cancer cases. We found no evidence of statistically significant departure from linearity (P=0.51). A 100 pmol ml−1 increment in serum vitamin B12 levels conferred an RR of 0.99 (0.92–1.08, P=0.88).
Vitamin B12 intake and risk of breast cancer
High vitamin B12 intake vs low intake was not significantly associated with the risk of breast cancer (0.88 (0.77–1.00), P=0.05, I2=68.9%, Figure 3). However, significant association was found in case–control studies (0.74 (0.56–0.98), P=0.04, I2=74.5%) but not in prospective studies. No significant association was found in other subgroup analysis.
For dose–response analysis, data from nine studies (Lajous et al, 2006a; Lin et al, 2008; Ma et al, 2009a; Ma et al, 2009b; Stevens et al, 2010; Chou et al, 2011; Zhang et al, 2011; Bassett et al, 2013; Yang et al, 2013) were used, including 9832 breast cancer cases. We found no evidence of statistically significant departure from linearity (P=0.14). A 1-μg per day increment in vitamin B12 intake conferred an RR of 0.98 (0.95–1.00, P=0.12).
Methionine intake and risk of breast cancer
High methionine intake vs low intake was significantly associated with the risk of breast cancer (0.94 (0.89–0.99), P=0.03, I2=0.00%, Figure 4). Marginally significant association was found in prospective studies (0.94 (0.87–1.00), P=0.06, I2=0.00%) but not in case–control studies (Figure 4). Significant association was found for post-menopausal women (0.89 (0.82–0.97), P=0.01, I2=0.01%) but not for pre-menopausal women; however, the difference between the two groups was not significant (P=0.24). No significant association was found by ER status and PR status. Marginally significant association was found for studies that adjusted for alcohol and use of exogenous hormones, and significant association was also found for studies that adjusted for physical activity, energy intake, BMI, FHBC and reproductive factors (⩾3).
The multivariate-adjusted risk of breast cancer for the highest vs lowest categories of dietary methionine intake in random-effects model. The size of the grey box is positively proportional to the weight assigned to each study, which is inversely proportional to the s.e. of the RR, and horizontal lines represent the 95% CIs.
For dose–response analysis, data from six studies (Feigelson et al, 2003; Xu et al, 2008; Stevens et al, 2010; Zhang et al, 2011; Bassett et al, 2013; Yang et al, 2013) were used, including 10316 breast cancer cases. We found no evidence of statistically significant departure from linearity (P=0.82). A 1-g per day increment in methionine intake conferred an RR of 0.96 (0.92–1.00, P=0.05).
Effect of combining folate with vitamin B6, vitamin B12 and methionine on risk of breast cancer
For the joint association between breast cancer risk and folate intake with vitamin B6 intake, data from four studies (Maruti et al, 2009a; Stevens et al, 2010; Chou et al, 2011; Shrubsole et al, 2011) were used, and the risk of breast cancer for the subjects with both highest intake of folate and vitamin B6 was 0.91 (0.79–1.04), P=0.17, I2=0.00%. For the joint association between breast cancer risk and folate intake with vitamin B12 intake, data from three studies (Maruti et al, 2009a; Stevens et al, 2010; Shrubsole et al, 2011) were used, and the risk of breast cancer for the subjects with both highest intake of folate and vitamin B12 was 0.99 (0.77–1.29), P=0.97, I2=54.2%. For the joint association between breast cancer risk and folate intake with methionine intake, data from four studies (Thorand et al, 1998; Maruti et al, 2009a; Stevens et al, 2010; Shrubsole et al, 2011) were used, and the risk of breast cancer for the subjects with both highest intake of folate and methionine was 0.81(0.62–1.05), P=0.11, I2=49.2%.
Sources of heterogeneity and meta-regression
In order to explore the moderate to high between-study heterogeneity found in several analysis, univariate meta-regression with the covariates of publication year, location where the study was conducted, study design (case–control or prospective), number of cases and degree of adjustments of covariates was performed. Degree of adjustments of covariates ranged from 0 to 9 based on adjustment (yes: 1, no: 0) of the following covariates: alcohol, smoking, BMI, FHBC, reproductive factors (⩾3), physical activity, energy intake, dietary factors (⩾2) and use of exogenous hormones. For the analysis between breast cancer risk and dietary vitamin B12 intake, study design was found contributing significantly to the between-study heterogeneity overall (P=0.02) and among post-menopausal women (P=0.02). No significant findings were found in the other analysis.
Sensitivity analysis and publication bias
Sensitivity analysis showed that no individual study had excessive influence on the above mentioned pooled effect. Egger test showed no evidence of significant publication bias for the analysis between breast cancer risk and serum PLP levels (P=0.10), vitamin B6 intake (P=0.14), serum vitamin B12 levels (P=0.18), vitamin B12 intake (P=0.12) and methionine (P=0.49). The funnel plots were provided in the Supplementary Material.
Discussion
The findings from this meta-analysis indicated that increased serum PLP levels and dietary methionine intake might be significantly associated with reduced risk of breast cancer, especially for post-menopausal women. No significant association was found between dietary vitamin B6 intake, serum vitamin B12 and dietary vitamin B12 intake and risk of breast cancer.
Several biological mechanisms for the inverse relationship of vitamin B6, vitamin B12 and methionine with the development of breast cancer have been proposed. First, vitamin B6, B12 and methionine participate in one-carbon metabolism, which is essential for DNA synthesis, repair and methylation (Ames, 2001), and vitamins B6 and B12 deficiencies also cause high uracil and chromosome breaks (Blount et al, 1997). Thus, deficiency in these nutrients may interfere with DNA methylation and synthesis, leading to aberrant gene expression and DNA instability, and eventually the development of cancer (Davis and Uthus, 2004). In addition, low B-group vitamin concentrations are associated with inflammation and higher oxidative stress (Shen et al, 2010), and antioxidants supplementation with B-group vitamins could enhance antioxidant capacity. Although the mechanism for the stronger association found for post-menopausal women remains unclear, previous meta-analysis also suggested that post-menopausal women are more susceptible to a wide range of dietary factors, including dietary fibre, vitamin A, β-carotene, retinol, vitamin C, calories, fat (Howe et al, 1990; Wu et al, 1999a), folate acid (Larsson et al, 2007), fatty acids (Saadatian-Elahi et al, 2004), and coffee and caffeine (Jiang et al, 2013), regarding their association with breast cancer risk. In addition, although these nutrient interactions were also proposed, no apparent joint association with high folate intake was found in this meta-analysis, which is consistent with the previous study (Zhang et al, 2008).
As a meta-analysis of published observational studies, our findings have several limitations. First, disparate results were found on dietary vitamin B6 intake and PLP with the risk of breast cancer. The multivariable Pearson’s correlation coefficients between plasma levels of vitamin B6 and vitamin B12, and the average intakes of vitamin B6 and vitamin B12 from food was 0.25 and 0.08, respectively (Zhang et al, 2003). In this respect, the serum biomarker of vitamin B6 (PLP) and vitamin B12 was able to examine these associations with higher precision. Disparate results between serum biomarkers of vitamins and dietary intake of vitamins and breast cancer risk were also found in other meta-analysis, such as vitamin B6 (Larsson et al, 2007) and vitamin D (Chen et al, 2010). Second, a meta-analysis of observational studies is susceptible to potential bias inherent in the original studies, especially for case–control studies. Stronger association was found in the combined results from case–control studies in this meta-analysis. Overstated association could be expected from the case–control studies because of recall or selection bias, and early symptoms in patients may have resulted in a change in dietary habits. Thus, the results from prospective studies might provide a more robust estimation of the associations.
Third, although we extracted the RRs that reflected the greatest degree of control for potential confounders, the extent to which they were adjusted and the possibility that the observed association was due to unmeasured or residual confounding should be considered. Furthermore, vitamin B6 intake tends to be associated with healthy behaviours that may be protective against breast cancer (Larsson et al, 2010). However, significant association was also found (0.76 (0.62–0.94)) on serum PLP levels and breast cancer risk for the three studies that adjusted for the most known risk factors of breast cancer. In addition, no significant interactions were found between MTHFR and MTR polymorphisms and B vitamins (Ma et al, 2009a; Ma et al, 2009b), and result from the study by Lin et al (2008) suggested a much stronger and significant association of serum PLP and vitamin B12 levels with breast cancer risk for never user of post-menopausal hormones. However, the limited data in the reported articles precluded a more robust assessment of the association by the above-mentioned risk factors.
Fourth, although significant association of PLP levels and methionine intake with risk of breast cancer was found among post-menopausal women, while not among pre-menopausal women, the difference between the two groups was not significant, and the apparent differences could simply be by chance, considering relatively small number of studies included, especially for pre-menopausal women. And subgroup analysis by tumour stage (in situ or invasive) were not conducted because of limited data availability (Zhang et al, 2003; Chou et al, 2011). Fifth, between-study heterogeneity was found in some analysis in this meta-analysis, but the between-study heterogeneity was not successfully explained by the subgroup analysis and meta-regression. However, other genetic and environment variables, as well as their possible interaction, non-comparable measurement of nutrients and variation of the covariates and so on, may well be potential contributors to this disease–effect unconformity (Higgins et al, 2003). In this respect, the lack of relevant study-level covariates in the reported articles precluded a more robust assessment of sources of this heterogeneity. Finally, although no significant publication bias was detected in this meta-analysis, validity of publication bias test should be questioned because of small number of studies included (Sterne et al, 2000), especially for PLP and serum vitamin B12.
In summary, results from this meta-analysis suggested that serum PLP levels and dietary methionine intake might be significantly associated with reduced risk of breast cancer, especially for post-menopausal women. The finding needs to be confirmed further by a well-conducted randomised trial.
Change history
01 October 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Ames BN (2001) DNA damage from micronutrient deficiencies is likely to be a major cause of cancer. Mutat Res 475: 7–20.
Bairoch A (2000) The ENZYME database in 2000. Nucleic Acids Res 28: 304–305.
Bassett JK, Baglietto L, Hodge AM, Severi G, Hopper JL, English DR, Giles GG (2013) Dietary intake of B vitamins and methionine and breast cancer risk. Cancer Causes Control 24 (8): 1555–1563.
Blount BC, Mack MM, Wehr CM, MacGregor JT, Hiatt RA, Wang G, Wickramasinghe SN, Everson RB, Ames BN (1997) Folate deficiency causes uracil misincorporation into human DNA and chromosome breakage: implications for cancer and neuronal damage. Proc Natl Acad Sci USA 94: 3290–3295.
Chen P, Hu P, Xie D, Qin Y, Wang F, Wang H (2010) Meta-analysis of vitamin D, calcium and the prevention of breast cancer. Breast Cancer Res Treat 121: 469–477.
Cho E, Holmes M, Hankinson SE, Willett WC (2007) Nutrients involved in one-carbon metabolism and risk of breast cancer among premenopausal women. Cancer Epidemiol Biomarkers Prev 16: 2787–2790.
Chou YC, Chu CH, Wu MH, Hsu GC, Yang T, Chou WY, Huang HP, Lee MS, Yu CP, Yu JC, Sun CA (2011) Dietary intake of vitamin B(6) and risk of breast cancer in Taiwanese women. J Epidemiol 21: 329–336.
Davis CD, Uthus EO (2004) DNA methylation, cancer susceptibility, and nutrient interactions. Exp Biol Med (Maywood) 229: 988–995.
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7: 177–188.
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315: 629–634.
Feigelson HS, Jonas CR, Robertson AS, McCullough ML, Thun MJ, Calle EE (2003) Alcohol, folate, methionine, and risk of incident breast cancer in the American Cancer Society Cancer Prevention Study II Nutrition Cohort. Cancer Epidemiol Biomarkers Prev 12: 161–164.
Goodman JE, Lavigne JA, Wu K, Helzlsouer KJ, Strickland PT, Selhub J, Yager JD (2001) COMT genotype, micronutrients in the folate metabolic pathway and breast cancer risk. Carcinogenesis 22: 1661–1665.
Harrell FE Jr, Lee KL, Pollock BG (1988) Regression models in clinical studies: determining relationships between predictors and response. J Natl Cancer Inst 80: 1198–1202.
Higgins JP, Thompson SG (2004) Controlling the risk of spurious findings from meta-regression. Stat Med 23: 1663–1682.
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327: 557–560.
Hong Z, Tian C, Zhang X (2012) Dietary calcium intake, vitamin D levels, and breast cancer risk: a dose-response analysis of observational studies. Breast Cancer Res Treat 136: 309–312.
Howe GR, Hirohata T, Hislop TG, Iscovich JM, Yuan JM, Katsouyanni K, Lubin F, Marubini E, Modan B, Rohan T et al (1990) Dietary factors and risk of breast cancer: combined analysis of 12 case-control studies. J Natl Cancer Inst 82: 561–569.
Jackson D, White IR, Thompson SG (2010) Extending DerSimonian and Laird’s methodology to perform multivariate random effects meta-analyses. Stat Med 29: 1282–1297.
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA Cancer J Clin 61: 69–90.
Jiang W, Wu Y, Jiang X (2013) Coffee and caffeine intake and breast cancer risk: an updated dose-response meta-analysis of 37 published studies. Gynecol Oncol 129 (3): 620–629.
Kabat GC, Miller AB, Jain M, Rohan TE (2008) Dietary intake of selected B vitamins in relation to risk of major cancers in women. Br J Cancer 99: 816–821.
Kim YI (2007) Folate and colorectal cancer: an evidence-based critical review. Mol Nutr Food Res 51: 267–292.
Kushi LH, Doyle C, McCullough M, Rock CL, Demark-Wahnefried W, Bandera EV, Gapstur S, Patel AV, Andrews K, Gansler T (2012) American Cancer Society Guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin 62: 30–67.
Lajous M, Lazcano-Ponce E, Hernandez-Avila M, Willett W, Romieu I (2006a) Folate, vitamin B(6), and vitamin B(12) intake and the risk of breast cancer among Mexican women. Cancer Epidemiol Biomarkers Prev 15: 443–448.
Lajous M, Romieu I, Sabia S, Boutron-Ruault MC, Clavel-Chapelon F (2006b) Folate, vitamin B12 and postmenopausal breast cancer in a prospective study of French women. Cancer Causes Control 17: 1209–1213.
Larsson SC, Giovannucci E, Wolk A (2007) Folate and risk of breast cancer: a meta-analysis. J Natl Cancer Inst 99: 64–76.
Larsson SC, Orsini N, Wolk A (2010) Vitamin B6 and risk of colorectal cancer: a meta-analysis of prospective studies. JAMA 303: 1077–1083.
Levi F, Pasche C, Lucchini F, La Vecchia C (2001) Dietary intake of selected micronutrients and breast-cancer risk. Int J Cancer 91: 260–263.
Lin J, Lee IM, Cook NR, Selhub J, Manson JE, Buring JE, Zhang SM (2008) Plasma folate, vitamin B-6, vitamin B-12, and risk of breast cancer in women. Am J Clin Nutr 87: 734–743.
Lurie G, Wilkens LR, Shvetsov YB, Ollberding NJ, Franke AA, Henderson BE, Kolonel LN, Goodman MT (2012) Prediagnostic plasma pyridoxal 5′-phosphate (vitamin b6) levels and invasive breast carcinoma risk: the multiethnic cohort. Cancer Epidemiol Biomarkers Prev 21: 1942–1948.
Ma E, Iwasaki M, Junko I, Hamada GS, Nishimoto IN, Carvalho SM, Motola J Jr, Laginha FM, Tsugane S (2009a) Dietary intake of folate, vitamin B6, and vitamin B12, genetic polymorphism of related enzymes, and risk of breast cancer: a case-control study in Brazilian women. BMC Cancer 9: 122.
Ma E, Iwasaki M, Kobayashi M, Kasuga Y, Yokoyama S, Onuma H, Nishimura H, Kusama R, Tsugane S (2009b) Dietary intake of folate, vitamin B2, vitamin B6, vitamin B12, genetic polymorphism of related enzymes, and risk of breast cancer: a case-control study in Japan. Nutr Cancer 61: 447–456.
Maruti SS, Ulrich CM, Jupe ER, White E (2009a) MTHFR C677T and postmenopausal breast cancer risk by intakes of one-carbon metabolism nutrients: a nested case-control study. Breast Cancer Res 11: R91.
Maruti SS, Ulrich CM, White E (2009b) Folate and one-carbon metabolism nutrients from supplements and diet in relation to breast cancer risk. Am J Clin Nutr 89: 624–633.
Orsini N, Bellocco R (2006) Generalized least squares for trend estimation of summarized dose–response data. Stata J 6: 40–57.
Orsini N, Li R, Wolk A, Khudyakov P, Spiegelman D (2012) Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol 175: 66–73.
Potera C, Rose DP, Brown RR (1977) Vitamin B6 deficiency in cancer patients. Am J Clin Nutr 30: 1677–1679.
Saadatian-Elahi M, Norat T, Goudable J, Riboli E (2004) Biomarkers of dietary fatty acid intake and the risk of breast cancer: a meta-analysis. Int J Cancer 111: 584–591.
Schroecksnadel K, Frick B, Fuchs D (2003) Re: Plasma folate, vitamin B6, vitamin B12, homocysteine, and risk of breast cancer. J Natl Cancer Inst 95: 1091 author reply 1091.
Selhub J (2002) Folate, vitamin B12 and vitamin B6 and one carbon metabolism. J Nutr Health Aging 6: 39–42.
Shen J, Lai CQ, Mattei J, Ordovas JM, Tucker KL (2010) Association of vitamin B-6 status with inflammation, oxidative stress, and chronic inflammatory conditions: the Boston Puerto Rican Health Study. Am J Clin Nutr 91: 337–342.
Shrubsole MJ, Gao YT, Cai Q, Shu XO, Dai Q, Jin F, Zheng W (2006) MTR and MTRR polymorphisms, dietary intake, and breast cancer risk. Cancer Epidemiol Biomarkers Prev 15: 586–588.
Shrubsole MJ, Jin F, Dai Q, Shu XO, Potter JD, Hebert JR, Gao YT, Zheng W (2001) Dietary folate intake and breast cancer risk: results from the Shanghai Breast Cancer Study. Cancer Res 61: 7136–7141.
Shrubsole MJ, Shu XO, Li HL, Cai H, Yang G, Gao YT, Gao J, Zheng W (2011) Dietary B vitamin and methionine intakes and breast cancer risk among Chinese women. Am J Epidemiol 173: 1171–1182.
Sterne JA, Gavaghan D, Egger M (2000) Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. J Clin Epidemiol 53: 1119–1129.
Stevens VL, McCullough ML, Sun J, Gapstur SM (2010) Folate and other one-carbon metabolism-related nutrients and risk of postmenopausal breast cancer in the Cancer Prevention Study II Nutrition Cohort. Am J Clin Nutr 91: 1708–1715.
Suzuki R, Orsini N, Mignone L, Saji S, Wolk A (2008) Alcohol intake and risk of breast cancer defined by estrogen and progesterone receptor status—a meta-analysis of epidemiological studies. Int J Cancer 122: 1832–1841.
Thorand B, Kohlmeier L, Simonsen N, Croghan C, Thamm M (1998) Intake of fruits, vegetables, folic acid and related nutrients and risk of breast cancer in postmenopausal women. Public Health Nutr 1: 147–156.
Wu AH, Pike MC, Stram DO (1999a) Meta-analysis: dietary fat intake, serum estrogen levels, and the risk of breast cancer. J Natl Cancer Inst 91: 529–534.
Wu K, Helzlsouer KJ, Comstock GW, Hoffman SC, Nadeau MR, Selhub J (1999b) A prospective study on folate, B12, and pyridoxal 5′-phosphate (B6) and breast cancer. Cancer Epidemiol Biomarkers Prev 8: 209–217.
Wu Y, Zhang D, Kang S (2013) Physical activity and risk of breast cancer: a meta-analysis of prospective studies. Breast Cancer Res Treat 137: 869–882.
Xu X, Gammon MD, Zeisel SH, Lee YL, Wetmur JG, Teitelbaum SL, Bradshaw PT, Neugut AI, Santella RM, Chen J (2008) Choline metabolism and risk of breast cancer in a population-based study. FASEB J 22: 2045–2052.
Yang D, Baumgartner RN, Slattery ML, Wang C, Giuliano AR, Murtaugh MA, Risendal BC, Byers T, Baumgartner KB (2013) Dietary intake of folate, B-vitamins and methionine and breast cancer risk among Hispanic and non-Hispanic white women. PLoS One 8: e54495.
Zhang CX, Ho SC, Chen YM, Lin FY, Fu JH, Cheng SZ (2011) Dietary folate, vitamin B6, vitamin B12 and methionine intake and the risk of breast cancer by oestrogen and progesterone receptor status. Br J Nutr 106: 936–943.
Zhang SM, Cook NR, Albert CM, Gaziano JM, Buring JE, Manson JE (2008) Effect of combined folic acid, vitamin B6, and vitamin B12 on cancer risk in women: a randomized trial. JAMA 300: 2012–2021.
Zhang SM, Willett WC, Selhub J, Hunter DJ, Giovannucci EL, Holmes MD, Colditz GA, Hankinson SE (2003) Plasma folate, vitamin B6, vitamin B12, homocysteine, and risk of breast cancer. J Natl Cancer Inst 95: 373–380.
Zhu K, Davidson NE, Hunter S, Yang X, Payne-Wilks K, Roland CL, Phillips D, Bentley C, Dai M, Williams SM (2003) Methyl-group dietary intake and risk of breast cancer among African-American women: a case-control study by methylation status of the estrogen receptor alpha genes. Cancer Causes Control 14: 827–836.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Wu, W., Kang, S. & Zhang, D. Association of vitamin B6, vitamin B12 and methionine with risk of breast cancer: a dose–response meta-analysis. Br J Cancer 109, 1926–1944 (2013). https://doi.org/10.1038/bjc.2013.438
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.438
Keywords
This article is cited by
-
Interactions dietary components with expression level of breast cancer-related genes
Egyptian Journal of Medical Human Genetics (2022)
-
Dietary phytochemicals/nutrients as promising protector of breast cancer development: a comprehensive analysis
Pharmacological Reports (2022)
-
Vitamin B6, vitamin B12 and methionine and risk of pancreatic cancer: a meta-analysis
Nutrition Journal (2020)
-
Folic acid supplement use and breast cancer risk in BRCA1 and BRCA2 mutation carriers: a case–control study
Breast Cancer Research and Treatment (2019)
-
Dietary vitamin C intake and the risk of hip fracture: a dose-response meta-analysis
Osteoporosis International (2018)