Abstract
Globally, cardiovascular diseases (CVDs) are the number one cause of mortality. Approximately 18 million people died from CVDs in 2015, representing more than 30% of all global deaths. New diagnostic tools and therapies are eagerly required to decrease the prevalence of CVDs related to mortality and/or risk factors leading to CVDs. Oxylipins are a group of metabolites, generated via oxygenation of polyunsaturated fatty acids that are involved in inflammation, immunity, and vascular functions, etc. Thus far, over 100 oxylipins have been identified, and have overlapping and interconnected roles. Important CVD pathologies such as hyperlipidemia, hypertension, thrombosis, hemostasis and diabetes have been linked to abnormal oxylipin signaling. Oxylipins represent a new era of risk markers and/or therapeutic targets in several diseases including CVDs. The role of many oxylipins in the progression or regression in CVD, however, is still not fully understood. An increased knowledge of the role of these oxygenated polyunsaturated fatty acids in cardiovascular dysfunctions or CVDs including hypertension could possibly lead to the development of biomarkers for the detection and their treatment in the future.
Similar content being viewed by others
Introduction
Cardiovascular Diseases (CVDs) are the number one cause of death globally: more people die annually from CVDs than from any other disease [World Health Organization (WHO)]. An estimated ∼18 million people died from CVDs in 2015, representing 31% of all global deaths (WHO). Of these deaths, an estimated 7.4 million were due to coronary heart disease and 6.7 million were due to stroke (WHO). Most cardiovascular diseases can be prevented; if we establish and sort out the precise circulating biomarkers (plasma oxylipins?) for the early detection of CVDs, including hypertension, which may possibly help us to avoid, use of risk factors such as tobacco, unhealthy diet, sedentary life style, and harmful use of alcohol. Also, people with cardiovascular disease or who are considered a high cardiovascular risk (due to the presence of one or more risk factors such as: hypertension, diabetes, hyperlipidemia or an already established disease) need early detection and management using counseling and medicines, as appropriate (WHO). Globally, 1.39 billion persons, representing 31% of all adults (25 years and over), have hypertension1. Out of which, 75 million American adults have hypertension; that is 1 out of every 3 adults (CDC, 2016). Surprisingly, the state of West Virginia is ranked #1 (41.0%±1.5%) in the top 10 highest rated states for hypertensive populations in the U.S. (2013, Trust for America's Health). Also, only about half (54%) of people in the US with hypertension have their condition under control; the other half (46%) are not under control and hypertension costs the US $46 billion each year (CDC, 2016). In addition to the hypertensive cases, nearly 1 out of 3 American adults have pre-hypertensive conditions too (CDC, 2016), and pre-hypertension and hypertension are the global major risk factors for the cardiovascular diseases (CVDs)2. Therefore, newer early diagnostic tools in the form of circulating biomarkers [plasma oxygenated polyunsaturated fatty acids (oxylipins)?] and therapies are required to decrease the CVDs. Oxylipins are the oxygenated polyunsaturated fatty acids that regulate inflammation, vascular response and coronary hyperemic response3,4,5,6,7,8,9,10,11,12.
Oxylipins
Oxylipins are bioactive lipids generated by the oxidation of polyunsaturated fatty acids (PUFAs)13. Since their discovery almost five decades ago, numerous biologic functions have been linked to them and many others are still being elucidated. The advancement in detection and quantification rejuvenated both interest and research in oxylipins with accurate nanomolar detection using an array of state-of-the-art mass spectrometry instruments14. Still, studying the biological functions of oxylipins is challenged by the sheer number of oxylipins discovered, thus far, over 100 oxylipins have been identified13, and have overlapping and interconnected roles. Important cardiovascular disease (CVD) pathologies, including: hyperlipidemia, hypertension, thrombosis, hemostasis, and diabetes have been linked to abnormal oxylipin signaling15.
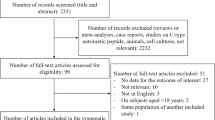
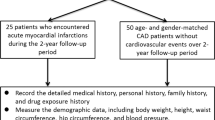
Oxylipins derived from arachidonic acid (AA) include EETs, HETEs, and prostanoids, whereas those derived from linoleic acid (LA) include EpOMEs and HODEs among others. Figure 1 illustrates some of AA- and LA-derived oxylipins and the main enzymes involved in their generation and breakdown, such as lipoxygenases, CYP-epoxygenases, ω-hydroxylases and cyclooxygenases. Figure 2 illustrates involvement of soluble epoxide hydrolase in changing the ratios of EpOME/DiHOME and EET/DHET, whereas, Figure 3 illustrate involvement of oxylipins in cardiovascular regulation.
Oxylipins biosynthesis
Oxylipins are both potent and short lived. Therefore, they are not stored; rather, they are synthesized de novo and regulated closely and exert their effect in a paracrine or autocrine manner13. Free PUFAs are mono- or dioxygenated by three families of enzymes: cyclooxygenase (COX), lipoxygenase (LOX), and cytochrome P450 (CYP) into distinct classes of oxylipins16. The type of oxylipins produced from PUFAs depends on the amount of dietary PUFAs consumed, the oxygenases (COX, LOX or CYP) present for metabolizing PUFAs, and the enzyme's affinity for a specific substrate PUFA3. The most well-known oxylipins are the eicosanoids (20-carbon compounds) formed from arachidonic acid (AA) and octadecanoids (18-carbon compounds) derived from linoleic acid (LA)3. Cyclooxygenase (COX) enzymes convert AA into prostanoids (PGs and thromboxanes). Also, COX enzymes can produce some hydroxy-metabolites, such as 11-HETE from AA and 9-HODE from LA17. Lipoxygenases (LOXs) catalyze the formation of hydroxy fatty acids, including: leukotrienes, lipoxins, resolvins, protectins, maresins, hepoxilins, and eoxins3. LOX enzymes also metabolize AA to form mid-chain (5-, 8-, 9-, 11-, 12-, and 15-) HETEs18. Cytochrome P450 (CYP) enzymes, which were originally known for their roles in xenobiotic metabolism, could either have epoxygenase or ω-hydroxylase activity3. ω-Hydroxylase enzymes (CYP4A and CYP4F) metabolize AA and generate ω-terminal (16-, 17-, 18-, 19-, and 20-) HETEs, whereas CYPs, with epoxygenase activity (CYP2C and CYP2J), metabolize AA and generate epoxyeicosatrienoic acid (EETs), which are further metabolized to dihydroxyeicosatrienoic acids (DHETs) by soluble epoxide hydrolase (sEH)13. AA can also be generated from LA metabolism19. Metabolism of LA includes the same enzyme families described above; for example, CYP epoxygenases metabolize LA to form EpOMEs, the epoxy compounds of LA. EpOMEs are hydrated by sEH to form DiHOMEs, the dihydroxy form of EpOMEs18. LOX enzymes form the hydroxy metabolites of LA: HODEs13. Oxylipins have a wide range of biological functions, many of which are still being investigated. They produce their effects through activating PPARs or through GPCRs20. Targeting sEH impacted the level of oxylipins directly affected by its catalytic activity, such as: EETs, DHETs, EpOMEs, and DiHOMEs and indirectly by affecting the other PUFAs pathways, such as; HODEs, and HETEs21. The latter observation could be explained by the shift observed in sEH−/− mice through AA metabolism due to EETs accumulation22, suggesting that the different oxylipin pathways affect one another. Further, compared to n-6 PUFAs, the supplemental dietary n-3 PUFAs have variety of health benefits against cardiovascular diseases by a decrease in the production of inflammatory mediators (eicosanoids, cytokines, and ROS) and the expression of adhesion molecules23,24,25,26,27. Also, the beneficial effects of n-3 PUFAs have been well discussed by Lorente-Cebrian et al in his review28, including enhanced vascular functions, cardioprotection, reduction in myocardial infarction, arrhythmia, sudden cardiac death, stroke, etc. However, the beneficial effects of n-3 PUFAs are not the interest of the current review article.
Epoxyeicosatrienoic acids (EETs)
EETs are 20-carbon metabolites of arachidonic acid (AA) with numerous physiologic actions. They are generated from AA by the cytochrome P450 epoxygenase pathway. Four distinct regioisomers are produced: 5,6-EET, 8,9-EET, 11,12-EET, and 14,15-EET. In the heart, EETs exert cardioprotective effects in ischemia/reperfusion injury29. EETs are classified as EDHFs; they are produced in endothelial cells and induce hyperpolarization in vascular smooth muscle cells by activating large conductance Ca2+-activated K+ channels (BKCa)30,31. EETs also cause vasodilation in many vascular beds, such as: the intestines32, kidney preglomerular vasculature33, conduit arteries34,35,36,37,38, and brain39. It is worth mentioning that small (KCa2.3) and medium (KCa3.1) conductance Ca2+-activated K+ channels are important in EETs-induced hyperpolarization31. EETs are metabolized rapidly by hydration to their corresponding, less active, DHETs by sEH, which is the main catabolic pathway responsible for EETs breakdown40. Not all EETs isomers are substrates for sEH; 5,6-EET is a poor substrate of sEH. In fact, this EET isomer (5,6-EET) along with 8,9-EET are substrates for cyclooxygenase (COX) pathway41. The half-life of 14,15-EET was found to be between 7.9–12.3 min42. Other catabolic pathways of EETs include ω-oxidation, β-oxidation, and chain elongation. The latter two pathways become more important when the activity of the main pathway, hydration by sEH, is inhibited41. Not only were EETs shown to have confirmed beneficial effects in numerous animal studies through their vasodilatory32,33,34,35,36,37,38,39, cardioprotective29, and anti-inflammatory effects43, they were also linked to decreased cardiovascular risk in epidemiological studies in humans44,45. Polymorphism variants where EETs production is decreased, such as decreased CYP2J2 expression (variant G-50T)45 or EETs breakdown is increased, such as increased sEH activity (variant K55R)44, had increased risk of coronary artery disease. It was speculated by some researchers that EETs exert their effects through specific cell surface receptors, which is supported by the finding that different responses were elicited by different stereoisomers and regioisomers of EETs46. However, it is worth mentioning that numerous reports linked EETs' signaling pathway with protein kinase A (PKA) and cAMP47.
Mid-chain hydroxyeicosatetraenoic acids (HETEs)
Mid-chain HETEs are produced through allylic oxidation of AA by lipoxygenase (LOX)22. They were shown to have chemotaxis effects, change in vascular tone, and induced the production of vascular endothelial growth factors48,49,50,51. Also, the increased formation of mid-chain HETEs was involved in cardiovascular dysfunction52,53,54,55. Also, mid-chain HETEs like 5-, 8-, 9-, 11-, and 12-HETE stimulate migration, chemotaxis and chemokinesis in leukocytes56,57,58,59, whereas, 15-HETE appears to have opposite effects60,61. Also, 15-HETE can be converted into lipoxins (LXs) which play a role in the resolution of inflammation62. Unlike the vasodilatory effect of EETs in the kidneys33, 12-HETE caused vasoconstriction in small renal arteries63. Also, the generation of mid-chain HETEs is increased in essential hypertension64 suggesting that they could be involved in its pathogenesis. These reports point to opposite effects of EETs vs HETEs in vascular biology. Maayah et al reported that mid-chain HETEs blocked the synthesis of EETs and increased their conversion to DHETs in RL-14 cells65. Moreover, although sEH is not directly involved in the generation or breakdown of mid-chain HETEs, sEH was found to be essential for mid-chain HETE–mediated induction of cellular hypertrophy65. Therefore, not only do EETs and mid-chain HETEs have opposite effects, they seem to affect the level of each other.
ω-Terminal hydroxyeicosatetraenoic acids (ω-terminal HETEs)
16-, 18-, 19-, and 20-HETEs are produced by cytochrome P450 ω-hydroxylase activity. 16-HETE is produced and released by polymorphonuclear leukocytes upon angiotensin II stimulation66. Of the ω-terminal HETEs, 20-HETE, which is a potent vasoconstrictor in mouse mesenteric arteries, mouse aorta and mouse coronary artery, is produced by CYP4A from arachidonic acid34,35,37,38,67,68,69,70,71. Also, 20-HETE is a potent vasoconstrictor in porcine coronary arteries72.
Epoxyoctadecaenoic acid (EpOMEs)
EpOMEs and DiHOMEs were reported to increase oxidative stress in vascular endothelial cells73,74,75; DiHOMEs were toxic to renal proximal tubular cells76 and intravenously injected 9,10-EpOME had cardiodepressive effects in dogs77. Pretreatment with 12,13-EpOME protected primary cultures of rabbit renal proximal tubular cells against hypoxia/reoxygenation injury78. Also, effects of EpOME/DiHOME ratio, induced by sEH inhibition using AUDA, improved renal recovery in response to ischemia/reperfusion injury in C57BL/6 mice79.
9-, 13-Hydroxyoctadecadienoic acids (9-, 13-HODEs)
Linoleic acid is also metabolized through hydroxylation by CYP epoxygenases to form hydroxyl-LA metabolites known as hydroxyoctadecadienoic acids (HODEs)22. HODEs are associated with oxidative stress80,81, and the 9-HODE induces macrophage IL-1β82. Also, 9- and 13-HODE activate plasminogen activator inhibitor type-1 via PPARγ activation in endothelial cells83, and 13-HODE is also suggested to have an anti-inflammatory role in inflammatory diseases through its effect as a PPARγ-agonist84,85,86,87,88. Also, 13-HODE increased prostacyclin (PGI2) biosynthesis, which was involved in splenic and coronary artery relaxation in smooth muscle cells in Mongrel dogs89. 9-HODE, unlike 13-HODE, was described as pro-inflammatory in an experimental wound-healing model in rats90,91, whereas, 13-HODE prevents platelets adhering in human vascular endothelial cells92,93.
Prostanoids
The term prostanoids comprises of two distinct groups: prostaglandins and thromboxanes. Prostaglandins G2 and H2, which are AA metabolites formed by COX isoforms (1 and 2), get converted into the 4 main bioactive PGs (D2, E2, I2, and F2α) and thromboxanes (TXA2 and TXB2)94,95. Most PGs have pro-inflammatory effects. However, PGE2 was found to have an anti-inflammatory role as well by up-regulating cAMP and inducing secretion of the anti-inflammatory IL-1096. Similarly, PGD2 attenuated inflammation in experimental models of pleuritis and colitis95. 6-keto-PGF1α is a stable metabolite and marker for PGI2 that is produced via cyclooxygenase (COX) signaling. 6-keto-PGF1α in humans is inversely related to cardiovascular events and high blood pressure97,98. PGF2α induces vasoconstriction in bovine, canine, and human coronary arteries99. PGF2α is associated with cardiac dysfunction and cardiac hypertrophy100,101. TXA2 induces vasoconstriction and aggregation of platelets102. Also, TXB2 is positively associated with high blood pressure and multiple cardiovascular dysfunctions97,98.
Discussion
Oxylipins regulate inflammation, vascular response and coronary hyperemic response3,4,5,6,7,9,10,11,12. Recently, in our laboratory, oxylipins were analyzed in both blood plasma and heart perfusates of adenosine A2A receptor knockout (A2AAR−/−) mice, where soluble epoxide hydrolase (sEH) was overexpressed and CYP2C was underexpressed69,103 compared to its wild-type mice (A2AAR+/+); Tie2-sEH Tr (sEH-overexpressed mice) compared to C57Bl/6; sEH knockout (sEH−/−) mice compared to its wild-type mice (sEH+/+); Tie2-CYP2J2 Tr (CYP2J2-overexpressed) compared to C57Bl/6 mice, and trans-4-[4-(3-adamantan-1-ylureido)cyclohexyloxy]benzoic acid (t-AUCB, sEH-inhibitor) treated C57Bl/6 compared to non-treated C57Bl/6 mice8,9,10,11,12. The heart perfusate data have demonstrated positive/negative effects of a brief ischemia on cardiac oxylipin levels (local) with enhanced or reduced coronary reactive hyperemic responses depending upon the mice (A2AAR−/−, sEH−/−, Tie2-sEH Tr, CYP2J2 Tr, C57Bl/6, and sEH-inhibitor-treated C57Bl/6 and other transgenic mice), as they are assessed before and after the ischemia in vitro mouse model of isolated heart9,10,11,12. Also, blood plasma oxylipins profile data of A2AAR−/− vs A2AAR+/+ have supported the data of heart perfusates (cardiac oxylipins profile) of A2AAR−/− vs A2AAR+/+ mice8. Further, there are evidences that show a relationship exists between endothelial dysfunctions involving cardiovascular diseases/hypertension and genetic polymorphisms in A2AAR, CYP2J2 and sEH genes in humans44,104,105,106,107,108. Similarly, A2AAR−/− have increased hypertension compared to A2AAR+/+ mice109. Hypertension was also observed in CYP2J5−/− compared to CYP2J5+/+ mice110, and sEH overexpression in rats have increased blood pressure compared to their respective control111, while sEH−/− mice had lower blood pressure40. Further, the up-regulation of angiotensin II is directly proportional to sEH up-regulation112, whereas, sEH inhibition blocks Angiotensin II-induced hypertension in rats113. As we mentioned earlier, the plasma levels of both EETs (oxylipins) and DHETs (oxylipins) levels in A2AAR−/− vs A2AAR+/+ mice supported the findings of the heart perfusate samples (cardiac oxylipins) of A2AAR−/− vs A2AAR+/+ mice; EETs/DHETs ratio was decreased by the elevated DHET levels which leads to significant reduction in coronary reactive hyperemic response in A2AAR−/− vs A2AAR+/+ mice8. Similarly, in the heart, EETs exert cardioprotective effects against ischemia/reperfusion injury29, and EETs are classified as EDHFs; they are produced in endothelial cells and induce hyperpolarization in vascular smooth muscle cells by activating large conductance BKCa30,31. EETs also cause vasodilation in many vascular beds, such as: the intestines32, kidney preglomerular vasculature33, conduit arteries34,35,36,37,38,69,103,114, and brain39. EETs are metabolized rapidly by hydration to their corresponding, less active, dihydroxyeicosatrienoic acids (DHETs) by soluble epoxide hydrolase sEH, which is the main catabolic pathway responsible for EETs breakdown40. Earlier, we reported that sEH knockout (sEH−/− mice) and pharmacologic inhibition of sEH decreased DHETs in heart perfusate (cardiac oxylipins) leading to significantly increased coronary reactive hyperemic response in sEH−/− and t-AUCB (sEH-inhibitor)-treated C57BL/6 vs their respective controls11,12. The increased expression of sEH and decreased expression of CYP2C in A2AAR−/− mice69,103 is probably the cause of an increase in DHETs' generation and drove the decrease in EET/DHET ratios in A2AAR−/− vs A2AAR+/+ mice8. Also, EETs have anti-inflammatory properties41, the higher the sEH activity [like K55R (genetic polymorphism in humans)] alters the ratio between EpOME:DiHOME (oxylipins) in the atherosclerosis risk in communities, where Caucasians carry K55R variant allele44. Also, we found out recently an enhanced coronary reactive response with the change in the isolated hearts perfusate oxylipins (cardiac) and plasma oxylipins (increased the ratio between EETs:DHETs, EpOMEs:DiHOMEs, and decreased in HETEs, prostanoids, TXB2, etc) in sEH−/−, Tie2-CYP2J2 Tr and sEH inhibitor-treated C57BL6 vs Tie2-sEH Tr and A2AAR−/− mice, and these oxylipins play an important role in the cardiovascular functions in mice8,9,10,11,12. Our observation in A2AAR−/− and Tie2-sEH Tr compared to its respective wild-type mice cardiac as well as plasma oxylipin data are very interesting since it suggests a possible decrease in the anti-inflammatory role of EETs and increase in the pro-inflammatory role of DHETs with the reduction in coronary reactive hyperemic response8,9. Also, effects have been reported on arachidonic acid metabolism leading to cardiovascular diseases due to cytochrome P450 polymorphism115, and this CYP450 polymorphisms are considered to be one of the determinants of susceptibility to cardiovascular diseases. CYP-epoxygenases, CYP2C and CYP2J2 metabolize arachidonic acid to form EETs, which are involved in vascular relaxation, anti-inflamation, anti-apoptosis, anti-thrombosis, and cardioprotective activities. Therefore, it is strongly suggested that genetic polymorphisms in CYP2C and CYP2J2 cause lower activities which are associated with an increased risk of several cardiovascular diseases like, hypertension and coronary artery disease116,117,118,119,120,121,122,123,124,125,126. Soluble epoxide hydrolase (sEH) metabolizes CYP-epoxygenases derived active epoxyeicosatrienoic acids from arachidonic acids to the less active dihydroxyeicosatrienoic acids (DHETs). Therefore, polymorphism in sEH gene has also been associated with cardiovascular diseases, such as the higher the sEH activity [K55R (genetic polymorphism in humans)] alters the ratio between EpOME:DiHOME (oxylipins) in the atherosclerosis risk in communities, where Caucasians carry K55R variant allele44,127. Also, genetic polymorphisms in ω-hydroxylases (CYP4A11 & CYP4F2) are associated with higher risk of hypertension through 20-HETE128,129,130. As we mentioned earlier, a relationship exists between endothelial dysfunctions involving cardiovascular diseases/hypertension and genetic polymorphisms in A2AAR, CYP2J2 and sEH genes in humans44,104,105,106,108. Therefore, we observed recently an enhanced coronary reactive response with the change in isolated hearts perfusate oxylipins (cardiac) and plasma oxylipins (increased the ratio between EETs:DHETs, EpOMEs:DiHOMEs, and decreased in HETEs, prostanoids, TXB2, etc) in sEH−/−, Tie2-CYP2J2 Tr and sEH inhibitor-treated C57BL6 compared to Tie2-sEH Tr and A2AAR−/− mice, and these oxylipins play an important role in the cardiovascular functions in mice8,9,10,11,12. The attenuated coronary reactive hyperemia (CRH) in A2AAR−/− and Tie2-sEH Tr mice could be due to decreased EET/DHET ratio, which could be attributed to the increased expression of sEH and decreased expression of CYP2C69,103, and this may indicate an overall reduction in EETs vasodilatory and anti-inflammatory activity in A2AAR−/− and Tie2-sEH Tr mice compared to their respective wild-type mice8,9.
In addition to EETs and DHETs, mid-chain (5-, 8-, 11-, 12- and 15-) HETEs were also detected in both blood plasma and heart perfusates, and they were increased with reduced coronary reactive hyperemic response in A2AAR−/− and Tie2-sEH Tr compared to their respective wild-type mice8,9. Lipoxygenases produce mid-chain HETEs from arachidonic acid (AA)22. Also, CYP-epoxygenase 1B1 produces mid-chain HETEs through oxidation of AA, and mid-chain HETEs have pro-inflammatory and vasoconstriction properties22,65,131. Further, cardiovascular dysfunction associated with increased formation of mid-chain HETEs have been reported52,53,54,55. As we mentioned earlier, heart perfusates and blood plasma demonstrated an increase in mid-chain HETEs in A2AAR−/− and Tie2-sEH Tr with reduced coronary reactive hyperemic response compared to their respective wild-type mice8,9. Therefore, the increase in mid-chain (5-, 8-, 11-, 12- and 15-) HETEs in A2AAR−/− and Tie2-sEH Tr mice, along with the decreased EET/DHET ratios, indicated an increase in the pro-inflammation and vasoconstriction associated with A2AAR–deletion (A2AAR−/−) and sEH overexpression (Tie2-sEH Tr) in mice, and might have contributed to the decrease or reduction of coronary reactive hyperemic response in both A2AAR−/− and Tie2-sEH Tr compared to their respective wild-type mice8,9.
Omega-terminal HETEs are also generated from AA, but through ω-hydroxylases (CYP4A, CYP4F)132. The primary oxylipin of ω-terminal HETEs is 20-HETE132, which promotes hypertension, vascular contraction, and vascular dysfunction133,134. Further, blocking 20-HETE synthesis reduced mean arterial pressure in old spontaneously hypertensive (SHR) female rats135. Our lab has recently reported that blocking ω-hydroxylases by DDMS/HET0016 enhanced coronary reactive hyperemic response and vascular relaxation in mesenteric arteries of sEH-overexpressed (Tie2-sEH Tr) and control mice9,67,136. Similarly, targeting the ω-terminal–HETEs pathway, reversed the decreased coronary reactive hyperemic response in A2AAR−/− mice8, because A2AAR−/− mice have ω-hydroxylases upregulated34,71. Therefore, ω-hydroxylases–inhibition reversed the decreased coronary reactive hyperemic response as well as vascular relaxation in A2AAR−/− mouse aorta and mesenteric arteries9,34,67,71,136. Further, we were able to detect these ω-terminal (19- and 20)-HETEs in plasma samples through LC-MS/MS and found increased levels of 20-HETE8. Therefore, the increased 20-HETE formation through ω-hydroxylases in A2AAR−/− compared to A2AAR+/+ mice, along with the other changes in plasma/cardiac oxylipins, suggests an increase in the pro-inflammation state, vascular contraction, and vascular dysfunction associated with A2AAR–deletion (A2AAR−/−) or sEH-overexpression (Tie2-sEH Tr) in mice may have contributed to the attenuated coronary reactive hyperemic response in A2AAR−/− and Tie2-sEH Tr compared to their respective wild-type mice. Similarly, in humans, 20-HETE is produced by CYP4A and CYP4F, and CYP4A11 genes, and polymorphisms in these genes are associated with essential hypertension in the male western Chinese Han population137. Also, CYP4A11 gene polymorphism is involved in coronary artery disease as well as myocardial infarction in Han and Uygur populations in China138,139.
Deletion of A2AAR in A2AAR−/− mice was associated with increased plasma/cardiac prostanoid levels too, including: PGF2α, PGE2, PGD2, and TXB2 compared to their respective wild type mice8. Prostanoids include two groups of metabolites (oxylipins): 1) thromboxanes (TXA2 and TXB2) and 2) bioactive prostaglandins (PGF2α, PGE2, PGI2, PGD2), and they are generally pro-inflammatory94,95. Therefore, the increased prostanoid levels in A2AAR−/− mice may have contributed to an increase in the proinflammatory state in A2AAR−/− compared to their respective wild-type mice8
Soluble epoxide hydrolase (sEH) role in cardiovascular biology extends beyond its role in the conversion of 5,6-, 8,9-, 11,12- and 14,15-EETs into 5,6-, 8,9-, 11,12- and 14,15-DHETs; it also plays a central role in the metabolism of arachidonic-, linoleic- and omega-3-derived oxylipins22. Like EpOMEs, whose parental fatty acid is linoleic acid, they are hydrolyzed to DiHOMEs by sEH. Also, we reported earlier that the deletion of sEH (sEH−/− mice)12 and inhibition of sEH by t-AUCB11 increased EpOMEs, decreased DiHOMEs, and increased EpOME/DiHOME ratio in heart perfusate. The increased EpOME/DiHOME and EETs/DHETs ratios were believed to contribute to the enhancement of coronary reactive hyperemic response11, which suggested that increased EpOME/DiHOME and EETs/DHETs ratios may have had a positive role in mediating vasodilation in coronary and aortas11,36,37,38,69,103. Also, a protective effect against hypoxia/reoxygenation injury by EpOMEs in primary cultures of rabbit renal proximal tubular cells was reported by Nowak et al 78, an effect which was faded away with DiHOMEs78. Further, endothelium-dependent vasodilation in the cerebral circulation was impaired by decreased EpOME/DiHOME ratio in Tie2-sEH Tr mice140. Therefore, in A2AAR-null mice had decreased EpOME/DiHOME ratio due to increased DiHOMEs in the plasma8. Whereas, sEH-null and C57Bl/6 mice treated with sEH inhibitor (t-AUCB) had an increased EpOME/DiHOME ratio due to increased EpOMEs and decreased DiHOMEs in the heart perfusates12. Also, DiHOMEs were reported to have deleterious effects, including: cytotoxic, cardiodepressive and vascular contraction141,142. Because of that, the decreased EpOME/DiHOME ratio and increased DiHOMEs in A2AAR-null mice may have contributed to the blunted coronary reactive hyperemic response. As mentioned earlier, sEH was overexpressed and CYP-epoxygenase was underexpressed A2AAR-null compared to wild-type mice69,103. Further, polymorphism in sEH gene has been associated with cardiovascular diseases, such as the higher the sEH activity [K55R (genetic polymorphism in humans)] alters the ratio between EpOME:DiHOME (oxylipins) in the atherosclerosis risk in communities, where Caucasians carry K55R variant allele44,127.
In addition to EpOMEs, HODEs are generated through hydroxylation of LA by CYP epoxygenases or lipoxygenases22. 9-HODE, but not 13-HODE, was increased in A2AAR−/− vs A2AAR+/+ mice. Role of 9-HODE is pro-inflammatory90,91, whereas role of 13-HODE could be anti-inflammatory84,85,86,87,88. The opposite effects of these two isomer oxylipins make this observation consistent with our earlier reports of an increased 13–HODE level in sEH–deleted (sEH−/−) and C57Bl/6 mice treated with sEH inhibitor (t-AUCB)11,12. The increased 9-HODE levels in A2AAR−/− mice plasma may be linked to the reported increase in sEH-expression and decreased expression of CYP-epoxygenase in A2AAR−/− compared to its wild-type mice69,103. Thus, the increased 9-HODE levels in A2AAR−/− and the decreased 9-HODE levels in sEH−/− and C57Bl/6 mice treated with sEH inhibitor (t-AUCB) may have contributed to the reduction of coronary reactive hyperemic response in A2AAR−/− and increased coronary reactive hyperemic response (CRH) in sEH−/− and C57Bl/6 mice treated with sEH inhibitor (t-AUCB)11,12.
Vascular endothelial overexpression of human CYP2J2 in mice (Tie2-CYP2J2 Tr) increased CRH after brief ischemia compared to respective wild-type mice10. As we described earlier, ischemic insult to the heart is likely to cause damage if not corrected within a short period of time8,9,11,12. The heart responds to ischemic insult by increasing coronary flow through CRH to reduce the deleterious effects of ischemia-induced damage8,9,11,12,143. Also, we previously described that the role of EETs and DHETs, as well as other oxylipins, in correlation with the changes in CRH in mice in response to brief ischemic insult8,9,11,12. More generation of EETs compared to DHETs have well-established their beneficial cardiovascular effects8,9,11,12,47,142,144,145; more EETs generation compared to DHETs protect from myocardial and cerebral ischemia/reperfusion injury29,146 and relaxes vascular beds, including: the intestines, preglomerular and brain32,33,39. Vascular endothelial overexpression of human CYP2J2 in mice (Tie2-CYP2J2 Tr) generates more EETs compared to their respective WT mice from AA through epoxidation11,147. The strategy to increase EETs level is to create the endothelial overexpression of CYP2J2 (Tie2-CYP2J2 Tr) in mice141,148. Endothelial overexpression of human CYP2J2 protected from cerebral ischemia in male mice, and 11,12- and 14,15-EET levels were increased in aortic endothelial cell (isolated from Tie2-CYP2J2 Tr mice) culture medium148. Jia et al also suggested that the protection against cerebral ischemia was linked to increase in blood flow and anti-inflammatory activities in endothelial overexpression of human CYP2J2 in mice (Tie2-CYP2J2 Tr)148, both of which are recognized effects of EETs32,33,39,149. In our lab, these Tie2-CYP2J2 Tr mice had increased CRH compared to its wild-type mice10, and this study also suggests that CYP2J2-derived EETs do play a significant role in CRH after a brief ischemic insult10. The CYP2J2*7 polymorphism in humans, which is associated with reduced CYP2J2 activity, was linked to higher risk of adverse cardiovascular outcomes including myocardial infarction125,150. Also, hypertension was observed in CYP2J5−/− compared to CYP2J5+/+ mice110.
In addition to EETs and DHETs in Tie2-CYP2J2 Tr mice, ω-terminal HETEs are generated from AA by CYP4A and CYP4F subfamilies132. The 19- and 20-HETEs are potent oxylipins typically found at very low levels, and these ω-terminal HETEs were below detectable levels in our mouse heart perfusate samples in both Tie2-CYP2J2 Tr and their respective wild-type mice10. Since the 20-HETE is a potent vasoconstrictor and involved with the renin-angiotensin system to produce hypertension, vasoconstriction, and vascular dysfunction132,133,134, we analyzed the effect of inhibiting ω-hydroxylases (CYP4A & CYP4F) activities by DDMS. DDMS enhanced CRH more in Tie2-CYP2J2 Tr vs WT mice10.
Another group of oxylipins produced by AA through cyclooxygenase pathway is prostanoids, which include prostaglandins (PGs) and TXB2. Vascular endothelial overexpression of CYP2J2 in mice (Tie2-CYP2J2 Tr) did not have significant changes in the cardiac prostanoid levels, but we observed a trend towards lower in Tie2-CYP2J2 Tr vs WT mice10. PGs are generally pro-inflammatory, but PGD2 and PGE2 have anti-inflammatory properties and secretes anti-inflammatory IL-1095,96. We described earlier that by targeting the EETs pathway (sEH deletion or sEH inhibition), the levels of cardiac prostanoids were decreased in isolated mouse heart perfusates11,12. Though, mice overexpressing the EETs-generating CYP2J2 in this study did not have significant change in prostanoid levels10, but interestingly, the levels of cardiac PGF2α and cardiac PGE2 were decreased in response to ischemia in Tie2-CYP2J2 Tr vs WT mice10.
Interestingly, 8-iso-PGF2α was significantly lower in Tie2-CYP2J2 Tr vs WT mice, and 8-iso-PGF2α is one of the isoprostanes, which are produced through lipid peroxidation of AA151. 8-iso-PGF2α, produced under the elevated level of reactive oxygen species (ROS), act as a surrogate marker for ROS production141. 8-iso-PGF2α is a potent vasoconstrictor in isolated guinea pig hearts151. The level of 8-iso-PGF2α was not changed by ischemic insult in Tie2-CYP2J2 Tr and WT mice, possibly because of brief ischemic insult, but the level of 8-iso-PGF2α was lower in Tie2-CYP2J2 Tr vs WT mice pre- and post-ischemia10. The decrease in 8-iso-PGF2α levels in Tie2-CYP2J2 Tr vs WT mice, and the subsequent decrease in vasoconstrictive activity, may have contributed to the enhanced CRH observed in Tie2-CYP2J2 Tr vs WT mice10.
Therefore, an increase in knowledge of plasma oxylipins profile in CVDs including hypertensive individuals, and these plasma oxylipins could be the predictors of cardiovascular diseases and hypertension. Recently, we observed increased 8,9-,11,12-,14,15-DHETs; increased 5-,11-,15-, 19-, 20-HETEs; increased prostanoids (6-keto-PGF1α, PGF2α, PGD2, PG-E2, and TxB2) levels; increased 9,10-,12,13-DiHOMEs; increased 9-, 13-HODEs; decreased in the ratio of 8,9-EETs:8,9-DHETs; 11,12-EETs:11,12-DHETs; 14,15-EETs: 14,15-DHETs and decreased 9,10- and 12,13- EpOME/DiHOME ratios in the plasma of A2AAR−/− vs A2AAR+/+ mice8. Further, A2AAR−/− mice have reduced CRH response, reduced vasodilation, hypertension with overexpression of soluble epoxide hydrolase and underexpression of CYP-epoxygenases in A2AAR−/− vs A2AAR+/+ mice8,69,103,109. These plasma oxylipins may be used as circulating biomarkers possibly detecting cardiovascular dysfunctions or cardiovascular diseases in future. Because, these oxygenated polyunsaturated fatty acids (oxylipins) regulate inflammation, vascular response, atherosclerosis, hypertension, and coronary hyperemic response3,4,5,6,7,8,9,10,11,12,44,109,110,127. Also, a strong relationship exists between endothelial dysfunctions involving cardiovascular diseases/hypertension and genetic polymorphisms in A2AAR, CYP2J2 and sEH genes in humans44,104,105,106,107,108.
Conclusion
A possible relationship exists between positive/negative changes in oxylipins profile and positive/negative changes in cardiovascular function in A2AAR−/−, sEH−/−, Tie2-sEH Tr, CYP2J2 Tr, C57Bl/6, and sEH-inhibitor-treated C57Bl/6 mice8,9,10,11,12. Also, a relationship exists between cardiovascular diseases and polymorphisms in adenosine receptors including A2A, CYP-epoxygenases (CYP2C, CYP2J2) and soluble epoxide hydrolase genes in humans44,104,105,106,107,108. Further, A2A AR−/− mice had sEH overexpressed and CYP2C underexpressed69,103, and the sEH gene, EPHX2, is called a susceptibility gene for CVDs in humans44. Higher sEH activity (K55R) due to polymorphism altered the ratio between EpOMEs: DiHOMEs with elevated atherosclerosis risk in Caucasian populations44. Furthermore, mid-chain (5-, 11-, 12- and 15-) HETEs (oxylipins) have chemotaxis effects, change vascular tone, and produce vascular endothelial growth factors48,49,50,51. Also, increased levels of mid-chain HETEs have been linked with cardiovascular dysfunctions52,53,54,55. Unlike the vasodilation, cardioprotective and anti-hypertensive effects of EETs in the reno-cardiovascular system33, the mid-chain HETEs are involved in essential hypertension64. Recently, we discovered an enhanced CRH response with a change in cardiac and plasma oxylipins (increase in the ratio between EETs:DHETs and EpOMEs:DiHOMEs, and decreases in HETEs, HODEs, prostanoids, TxB2, etc) isolated from mouse (sEH−/−,Tie2-CYP2J2 Tr and sEH inhibitor-treated C57BL/6) heart perfusates and blood plasma vs A2AAR−/− and Tie2-sEHTr mice (reduced CRH response, decreased ratio between EETs:DHETs and EpOMEs:DiHOMEs, and increases in HETEs, HODEs, prostanoids, TXB2, etc)8,9,10,11,12. These cardiac and plasma oxylipins play a pivotal role in the regulation of cardiovascular functions in mice8,9,10,11,12. DHETs are the sEH-catalyzed metabolic breakdown products of EETs; EETs have anti-inflammatory properties41, but A2AAR−/− mice have increased DHETs vs EETs due to increased expression of sEH and decreased expression of CYP2C with more vasoconstriction in A2AAR−/− vs A2AAR+/+ mice8,69,103. Whereas, sEH−/− mice have increased EETs vs DHETs with more A2AAR upregulation and vasodilation in sEH−/− vs sEH+/+ mice12,36. Increased ω-HETEs (20-HETE) and mid-chain HETEs are observed in blood plasma of A2AAR−/− vs A2AAR+/+ mice8. Whereas, 20-HETE and mid-chain HETEs were decreased in sEH−/− vs sEH+/+ mice12. Also, 20-HETE promotes hypertension, vasoconstriction, and vascular dysfunction133,134. A2AAR−/− mice had increased plasma prostanoid levels, including 6-keto-PGF1α, PGE2, PGF2α, and TXB28. Also, prostaglandins are pro-inflammatory95, and TXB2 is the inactive degradation product of TXA2, which mediates platelet aggregation, smooth muscle contraction, and endothelial inflammation95. In A2AAR−/− mice, a decrease in EpOME/DiHOME ratio was driven by increased DiHOMEs and decreased EpOMEs in the blood plasma with reduced CRH8, whereas, an increase in EpOME/DiHOME ratio was driven by increased EpOMEs and decreased DiHOMEs with enhanced CRH12, and DiHOMEs have deleterious effects, including cytotoxic, cardiodepressive, and vasoconstrictive properties141,142. HODEs were increased in A2AAR−/− vs A2AAR+/+ mice8, and HODEs are thought to be pro-inflammatory90,91. All these changes in cardiac and plasma oxylipins profile in A2AAR−/− and Tie2-sEHTr compared to their respective wild-type and sEH−/−, Tie2-CYP2J2 Tr and sEH inhibitor-treated C57BL/6 mice may be responsible for the significantly reduced CRH response, increase in blood pressure, increase in vasoconstriction, and cardiovascular dysfunctions8,9,10,11,12,44,48,49,50,51,52,53,54,55,64,103,109,133,134. Therefore, an increase in knowledge of plasma oxylipins profile in CVDs including hypertensive individuals may be used as circulating biomarkers possibly detecting cardiovascular dysfunctions or cardiovascular diseases in future.
Abbreviations
6-keto-PGF1α: 6-keto prostaglandin-F1α; AA: Arachinodic acid; A2AAR: A2A adenosine receptor; BK: Large conductance potassium channels; COX: Cyclooxygenase; CRH: coronary reactive hyperemia; CYP2J2: Cytochrome P450 2J2; CYP450: cytochrome P450; DDMS: dibromo-dodecenyl-methylsulfimide; DHETs: dihydroxyeicosatrienoic acids; DiHOMEs: dihydroxyoctadecaenoic acids; EDHF: endothelium-derived hyperpolarizing factor; EETs: epoxyeicosatrienoic acids; EpOMEs: epoxyoctadecaenoic acids; HETEs: hydroxyeicosatetraenoic acids; HODEs: hydroxyoctadecadienoic acids; KATP: ATP-sensitive K+ channels; KCa: calcium-acitvated K+ channels; LC-MS/MS: liquid chromatography, tandem mass spectroscopy; LOX: Lipoxygenase; PG: prostaglandin; PHF: peak hyperemic flow; PUFAs: polyunsaturated fatty acids; sEH: soluble epoxide hydrolase; sEH−/−: sEH–knockout mice; sEH+/+: wild type mice normally expressing sEH; t-AUCB: trans-4-[4-(3-adamantan-1-ylureido)cyclohexyloxy] benzoic acid; TXA2: thromboxane A2; TXB2: thromboxane B2; PGF2α: prostaglandin-F2α; PGD2: prostaglandin-D2; PGE2 prostaglandin-E2; LA: linoleic acid.
References
Bloch MJ. Worldwide prevalence of hypertension exceeds 1.3 billion. J Am Soc Hypertens 2016; 10: 753–54.
Albarwani S, Al-Siyabi S, Tanira MO. Prehypertension: Underlying pathology and therapeutic options. World J Cardiol 2014; 6: 728–43.
Gabbs M, Leng S, Devassy JG, Monirujjaman M, Aukema HM. Advances in our understanding of oxylipins derived from dietary PUFAs. Adv Nutr 2015; 6: 513–40.
Nishimaki S, Seki K. An imbalance between prostacyclin and thromboxane in relation to cerebral blood flow in neonates with maternal preeclampsia. Prostaglandins Other Lipid Mediat 1999; 58: 43–9.
Norris PC, Dennis EA. A lipidomic perspective on inflammatory macrophage eicosanoid signaling. Adv Biol Regul 2014; 54: 99–110.
Dennis EA, Norris PC. Eicosanoid storm in infection and inflammation. Nat Rev Immunol 2015; 15: 511–23.
Eskildsen MP, Hansen PB, Stubbe J, Toft A, Walter S, Marcussen N, et al. Prostaglandin I2 and prostaglandin E2 modulate human intrarenal artery contractility through prostaglandin E2-EP4, prostacyclin-IP, and thromboxane A2-TP receptors. Hypertension 2014; 64: 551–6.
Hanif A, Edin ML, Zeldin DC, Morisseau C, Falck JR, Ledent C, et al. Reduced coronary reactive hyperemia in mice was reversed by the soluble epoxide hydrolase inhibitor (t-AUCB): Role of adenosine A2A receptor and plasma oxylipins. Prostaglandins Other Lipid Mediat 2017; 131: 83–95.
Hanif A, Edin ML, Zeldin DC, Morisseau C, Falck JR, Nayeem MA. Vascular endothelial over-expression of human soluble epoxide hydrolase (Tie2-sEH Tr) attenuates coronary reactive hyperemia in mice: role of oxylipins and omega-hydroxylases. PLoS One 2017; 12: e0169584.
Hanif A, Edin ML, Zeldin DC, Morisseau C, Falck JR, Nayeem MA. Vascular endothelial overexpression of human CYP2J2 (Tie2-CYP2J2 Tr) modulates cardiac oxylipin profiles and enhances coronary reactive hyperemia in mice. PLoS One 2017; 12: e0174137.
Hanif A, Edin ML, Zeldin DC, Morisseau C, Nayeem MA. Effect of soluble epoxide hydrolase on the modulation of coronary reactive hyperemia: role of oxylipins and PPARgamma. PLoS One 2016; 11: e0162147.
Hanif A, Edin ML, Zeldin DC, Morisseau C, Nayeem MA. Deletion of soluble epoxide hydrolase enhances coronary reactive hyperemia in isolated mouse heart: role of oxylipins and PPARgamma. Am J Physiol Regul Integr Comp Physiol 2016; 311: R676–R88.
Tourdot BE, Ahmed I, Holinstat M. The emerging role of oxylipins in thrombosis and diabetes. Front Pharmacol 2014; 4: 176.
Strassburg K, Huijbrechts AM, Kortekaas KA, Lindeman JH, Pedersen TL, Dane A, et al. Quantitative profiling of oxylipins through comprehensive LC-MS/MS analysis: application in cardiac surgery. Anal Bioanal Chem 2012; 404: 1413–26.
Gleim S, Stitham J, Tang WH, Martin KA, Hwa J. An eicosanoid-centric view of atherothrombotic risk factors. Cell Mol Life Sci 2012; 69: 3361–80.
Massey KA, Nicolaou A. Lipidomics of oxidized polyunsaturated fatty acids. Free Radic Biol Med 2013; 59: 45–55.
Thuresson ED, Lakkides KM, Smith WL. Different catalytically competent arrangements of arachidonic acid within the cyclooxygenase active site of prostaglandin endoperoxide H synthase-1 lead to the formation of different oxygenated products. J Biol Chem 2000; 275: 8501–7.
Askari AA, Thomson S, Edin ML, Lih FB, Zeldin DC, Bishop-Bailey D. Basal and inducible anti-inflammatory epoxygenase activity in endothelial cells. Biochem Biophys Res Commun 2014; 446: 633–7.
Lagarde M, Bernoud-Hubac N, Calzada C, Vericel E, Guichardant M. Lipidomics of essential fatty acids and oxygenated metabolites. Mol Nutr Food Res 2013; 57: 1347–58.
Shearer GC, Newman JW. Impact of circulating esterified eicosanoids and other oxylipins on endothelial function. Curr Atheroscler Rep 2009; 11: 403–10.
Luria A, Weldon SM, Kabcenell AK, Ingraham RH, Matera D, Jiang H, et al. Compensatory mechanism for homeostatic blood pressure regulation in Ephx2 gene-disrupted mice. J Biol Chem 2007; 282: 2891–8.
Konkel A, Schunck WH. Role of cytochrome P450 enzymes in the bioactivation of polyunsaturated fatty acids. Biochim Biophys Acta 2011; 1814: 210–22.
Calder PC. Polyunsaturated fatty acids, inflammation, and immunity. Lipids 2001; 36: 1007–24.
Calder PC. n-3 fatty acids, inflammation, and immunity--relevance to postsurgical and critically ill patients. Lipids 2004; 39: 1147–61.
Calder PC. N-3 polyunsaturated fatty acids and inflammation: from molecular biology to the clinic. Lipids 2003; 38: 343–52.
Calder PC. Polyunsaturated fatty acids and inflammation. Biochem Soc Trans 2005; 33: 423–7.
Yaqoob P. Fatty acids as gatekeepers of immune cell regulation. Trends Immunol 2003; 24: 639–45.
Lorente-Cebrian S, Costa AG, Navas-Carretero S, Zabala M, Martinez JA, Moreno-Aliaga MJ. Role of omega-3 fatty acids in obesity, metabolic syndrome, and cardiovascular diseases: a review of the evidence. J Physiol Biochem 2013; 69: 633–51.
Seubert J, Yang B, Bradbury JA, Graves J, Degraff LM, Gabel S, et al. Enhanced postischemic functional recovery in CYP2J2 transgenic hearts involves mitochondrial ATP-sensitive K+ channels and p42/p44 MAPK pathway. Circ Res 2004; 95: 506–14.
Campbell WB, Gebremedhin D, Pratt PF, Harder DR. Identification of epoxyeicosatrienoic acids as endothelium-derived hyperpolarizing factors. Circ Res 1996; 78: 415–23.
Fleming I. The pharmacology of the cytochrome P450 epoxygenase/soluble epoxide hydrolase axis in the vasculature and cardiovascular disease. Pharmacol Rev 2014; 66: 1106–40.
Proctor KG, Falck JR, Capdevila J. Intestinal vasodilation by epoxyeicosatrienoic acids: arachidonic acid metabolites produced by a cytochrome P450 monooxygenase. Circ Res 1987; 60: 50–9.
Imig JD, Navar LG, Roman RJ, Reddy KK, Falck JR. Actions of epoxygenase metabolites on the preglomerular vasculature. J Am Soc Nephrol 1996; 7: 2364–70.
Nayeem MA, Poloyac SM, Falck JR, Zeldin DC, Ledent C, Ponnoth DS, et al. Role of CYP epoxygenases in A2A AR-mediated relaxation using A2A AR-null and wild-type mice. Am J Physiol Heart Circ Physiol 2008; 295: H2068–78.
Nayeem MA, Ponnoth DS, Boegehold MA, Zeldin DC, Falck JR, Mustafa SJ. High-salt diet enhances mouse aortic relaxation through adenosine A2A receptor via CYP epoxygenases. Am J Physiol Regul Integr Comp Physiol 2009; 296: R567–74.
Nayeem MA, Pradhan I, Mustafa SJ, Morisseau C, Falck JR, Zeldin DC. Adenosine A2A receptor modulates vascular response in soluble epoxide hydrolase-null mice through CYP-epoxygenases and PPARgamma. Am J Physiol Regul Integr Comp Physiol 2013; 304: R23–32.
Nayeem MA, Zeldin DC, Boegehold MA, Falck JR. Salt modulates vascular response through adenosine A(2A) receptor in eNOS-null mice: role of CYP450 epoxygenase and soluble epoxide hydrolase. Mol Cell Biochem 2011; 350: 101–11.
Nayeem MA, Zeldin DC, Boegehold MA, Morisseau C, Marowsky A, Ponnoth DS, et al. Modulation by salt intake of the vascular response mediated through adenosine A(2A) receptor: role of CYP epoxygenase and soluble epoxide hydrolase. Am J Physiol Regul Integr Comp Physiol 2010; 299: R325–33.
Gebremedhin D, Ma YH, Falck JR, Roman RJ, VanRollins M, Harder DR. Mechanism of action of cerebral epoxyeicosatrienoic acids on cerebral arterial smooth muscle. Am J Physiol 1992; 263: H519–25.
Sinal CJ, Miyata M, Tohkin M, Nagata K, Bend JR, Gonzalez FJ. Targeted disruption of soluble epoxide hydrolase reveals a role in blood pressure regulation. J Biol Chem 2000; 275: 40504–10.
Imig JD. Epoxides and soluble epoxide hydrolase in cardiovascular physiology. Physiol Rev 2012; 92: 101–30.
Catella F, Lawson JA, Fitzgerald DJ, FitzGerald GA. Endogenous biosynthesis of arachidonic acid epoxides in humans: increased formation in pregnancy-induced hypertension. Proc Natl Acad Sci U S A 1990; 87: 5893–7.
Shahabi P, Siest G, Meyer UA, Visvikis-Siest S. Human cytochrome P450 epoxygenases: variability in expression and role in inflammation-related disorders. Pharmacol Ther 2014; 144: 134–61.
Lee CR, North KE, Bray MS, Fornage M, Seubert JM, Newman JW, et al. Genetic variation in soluble epoxide hydrolase (EPHX2) and risk of coronary heart disease: The Atherosclerosis Risk in Communities (ARIC) study. Hum Mol Genet 2006; 15: 1640–9.
Lee CR, North KE, Bray MS, Couper DJ, Heiss G, Zeldin DC. CYP2J2 and CYP2C8 polymorphisms and coronary heart disease risk: the Atherosclerosis Risk in Communities (ARIC) study. Pharmacogenet Genomics 2007; 17: 349–58.
Yang W, Tuniki VR, Anjaiah S, Falck JR, Hillard CJ, Campbell WB. Characterization of epoxyeicosatrienoic acid binding site in U937 membranes using a novel radiolabeled agonist, 20-125i-14,15-epoxyeicosa-8(Z)-enoic acid. J Pharmacol Exp Ther 2008; 324: 1019–27.
Node K, Ruan XL, Dai J, Yang SX, Graham L, Zeldin DC, et al. Activation of Galphas mediates induction of tissue-type plasminogen activator gene transcription by epoxyeicosatrienoic acids. J Biol Chem 2001; 276: 15983–9.
Honda HM, Leitinger N, Frankel M, Goldhaber JI, Natarajan R, Nadler JL, et al. Induction of monocyte binding to endothelial cells by MM-LDL: role of lipoxygenase metabolites. Arterioscler Thromb Vasc Biol 1999; 19: 680–6.
Nakao J, Ooyama T, Ito H, Chang WC, Murota S. Comparative effect of lipoxygenase products of arachidonic acid on rat aortic smooth muscle cell migration. Atherosclerosis 1982; 44: 339–42.
Stern N, Natarajan R, Tuck ML, Laird E, Nadler JL. Selective inhibition of angiotensin-II-mediated aldosterone secretion by 5-hydroxyeicosatetraenoic acid. Endocrinology 1989; 125: 3090–5.
Tang DG, Renaud C, Stojakovic S, Diglio CA, Porter A, Honn KV. 12(S)-HETE is a mitogenic factor for microvascular endothelial cells: its potential role in angiogenesis. Biochem Biophys Res Commun 1995; 211: 462–8.
Conrad DJ, Kuhn H, Mulkins M, Highland E, Sigal E. Specific inflammatory cytokines regulate the expression of human monocyte 15-lipoxygenase. Proc Natl Acad Sci U S A 1992; 89: 217–21.
Stern N, Yanagawa N, Saito F, Hori M, Natarajan R, Nadler J, et al. Potential role of 12 hydroxyeicosatetraenoic acid in angiotensin II-induced calcium signal in rat glomerulosa cells. Endocrinology 1993; 133: 843–7.
Wen Y, Nadler JL, Gonzales N, Scott S, Clauser E, Natarajan R. Mechanisms of ANGII-induced mitogenic responses: role of 12-lipoxygenase and biphasic MAP kinase. Am J Physiol 1996; 271: C1212–20.
Patricia MK, Kim JA, Harper CM, Shih PT, Berliner JA, Natarajan R, et al. Lipoxygenase products increase monocyte adhesion to human aortic endothelial cells. Arterioscler Thromb Vasc Biol 1999; 19: 2615–22.
Goetzl EJ, Pickett WC. The human PMN leukocyte chemotactic activity of complex hydroxy-eicosatetraenoic acids (HETEs). J Immunol 1980; 125: 1789–91.
Goldman DW, Pickett WC, Goetzl EJ. Human neutrophil chemotactic and degranulating activities of leukotriene B5 (LTB5) derived from eicosapentaenoic acid. Biochem Biophys Res Commun 1983; 117: 282–8.
Strassburg K, Esser D, Vreeken RJ, Hankemeier T, Muller M, van Duynhoven J, et al. Postprandial fatty acid specific changes in circulating oxylipins in lean and obese men after high-fat challenge tests. Mol Nutr Food Res 2014; 58: 591–600.
Kim JW, Zou Y, Yoon S, Lee JH, Kim YK, Yu BP, et al. Vascular aging: molecular modulation of the prostanoid cascade by calorie restriction. J Gerontol A Biol Sci Med Sci 2004; 59: B876–85.
Smith RJ, Justen JM, Nidy EG, Sam LM, Bleasdale JE. Transmembrane signaling in human polymorphonuclear neutrophils: 15(S)-hydroxy-(5Z,8Z,11Z,13E)-eicosatetraenoic acid modulates receptor agonist-triggered cell activation. Proc Natl Acad Sci U S A 1993; 90: 7270–4.
Takenaga M, Hirai A, Terano T, Tamura Y, Kitagawa H, Yoshida S. Comparison of the in vitro effect of eicosapentaenoic acid (EPA)-derived lipoxygenase metabolites on human platelet function with those of arachidonic acid. Thromb Res 1986; 41: 373–84.
Buckley CD, Gilroy DW, Serhan CN. Proresolving lipid mediators and mechanisms in the resolution of acute inflammation. Immunity 2014; 40: 315–27.
Ma YH, Harder DR, Clark JE, Roman RJ. Effects of 12-HETE on isolated dog renal arcuate arteries. Am J Physiol 1991; 261: H451–6.
Dolegowska B, Blogowski W, Kedzierska K, Safranow K, Jakubowska K, Olszewska M, et al. Platelets arachidonic acid metabolism in patients with essential hypertension. Platelets 2009; 20: 242–9.
Maayah ZH, El-Kadi AO. The role of mid-chain hydroxyeicosatetraenoic acids in the pathogenesis of hypertension and cardiac hypertrophy. Arch Toxicol 2016; 90: 119–36.
Bednar MM, Gross CE, Balazy MK, Belosludtsev Y, Colella DT, Falck JR, et al. 16(R)-hydroxy-5,8,11,14-eicosatetraenoic acid, a new arachidonate metabolite in human polymorphonuclear leukocytes. Biochem Pharmacol 2000; 60: 447–55.
Yadav VR, Hong KL, Zeldin DC, Nayeem MA. Vascular endothelial over-expression of soluble epoxide hydrolase (Tie2-sEH) enhances adenosine A1 receptor-dependent contraction in mouse mesenteric arteries: role of ATP-sensitive K+ channels. Mol Cell Biochem 2016; 422: 197–206.
Yadav VR, Nayeem MA, Tilley SL, Mustafa SJ. Angiotensin II stimulation alters vasomotor response to adenosine in mouse mesenteric artery: Role for A and A adenosine receptors. Br J Pharmacol 2015; 172: 4959–69.
Pradhan I, Zeldin DC, Ledent C, Mustafa JS, Falck JR, Nayeem MA. High salt diet exacerbates vascular contraction in the absence of adenosine A(2)A receptor. J Cardiovasc Pharmacol 2014; 63: 385–94.
Kunduri SS, Mustafa SJ, Ponnoth DS, Dick GM, Nayeem MA. Adenosine A1 receptors link to smooth muscle contraction via CYP4a, protein kinase C-alpha, and ERK1/2. J Cardiovasc Pharmacol 2013; 62: 78–83.
Ponnoth DS, Nayeem MA, Kunduri SS, Tilley SL, Zeldin DC, Ledent C, et al. Role of omega-hydroxylase in adenosine-mediated aortic response through MAP kinase using A2A-receptor knockout mice. Am J Physiol Regul Integr Comp Physiol 2012; 302: R400–8.
Ramsden CE, Ringel A, Majchrzak-Hong SF, Yang J, Blanchard H, Zamora D, et al. Dietary linoleic acid-induced alterations in pro- and anti-nociceptive lipid autacoids: Implications for idiopathic pain syndromes? Mol Pain 2016; 12. pii: 1744806916636386. doi: 10.1177/1744806916636386.
Viswanathan S, Hammock BD, Newman JW, Meerarani P, Toborek M, Hennig B. Involvement of CYP2C9 in mediating the proinflammatory effects of linoleic acid in vascular endothelial cells. J Am Coll Nutr 2003; 22: 502–10.
Moller K, Ostermann AI, Rund K, Thoms S, Blume C, Stahl F, et al. Influence of weight reduction on blood levels of C-reactive protein, tumor necrosis factor-alpha, interleukin-6, and oxylipins in obese subjects. Prostaglandins Leukot Essent Fatty Acids 2016; 106: 39–49.
Vericel E, Croset M, Sedivy P, Courpron P, Dechavanne M, Lagarde M. Platelets and aging. I--Aggregation, arachidonate metabolism and antioxidant status. Thromb Res 1988; 49: 331–42.
Moran JH, Weise R, Schnellmann RG, Freeman JP, Grant DF. Cytotoxicity of linoleic acid diols to renal proximal tubular cells. Toxicol Appl Pharmacol 1997; 146: 53–9.
Sugiyama S, Hayakawa M, Nagai S, Ajioka M, Ozawa T. Leukotoxin, 9, 10-epoxy-12-octadecenoate, causes cardiac failure in dogs. Life Sci 1987; 40: 225–31.
Nowak G, Grant DF, Moran JH. Linoleic acid epoxide promotes the maintenance of mitochondrial function and active Na+ transport following hypoxia. Toxicol Lett 2004; 147: 161–75.
Lee JP, Yang SH, Lee HY, Kim B, Cho JY, Paik JH, et al. Soluble epoxide hydrolase activity determines the severity of ischemia-reperfusion injury in kidney. PLoS One 2012; 7: e37075.
Folcik VA, Cathcart MK. Predominance of esterified hydroperoxy-linoleic acid in human monocyte-oxidized LDL. J Lipid Res 1994; 35: 1570–82.
Honn KV, Nelson KK, Renaud C, Bazaz R, Diglio CA, Timar J. Fatty acid modulation of tumor cell adhesion to microvessel endothelium and experimental metastasis. Prostaglandins 1992; 44: 413–29.
Kramer HJ, Stevens J, Grimminger F, Seeger W. Fish oil fatty acids and human platelets: dose-dependent decrease in dienoic and increase in trienoic thromboxane generation. Biochem Pharmacol 1996; 52: 1211–7.
Marmol F, Puig-Parellada P, Sanchez J, Trullas R. Influence of aging on thromboxane A2 and prostacyclin levels in rat hippocampal brain slices. Neurobiol Aging 1999; 20: 695–7.
Emerson MR, LeVine SM. Experimental allergic encephalomyelitis is exacerbated in mice deficient for 12/15-lipoxygenase or 5-lipoxygenase. Brain Res 2004; 1021: 140–5.
Belvisi MG, Mitchell JA. Targeting PPAR receptors in the airway for the treatment of inflammatory lung disease. Br J Pharmacol 2009; 158: 994–1003.
Altmann R, Hausmann M, Spottl T, Gruber M, Bull AW, Menzel K, et al. 13-Oxo-ODE is an endogenous ligand for PPARgamma in human colonic epithelial cells. Biochem Pharmacol 2007; 74: 612–22.
Stoll LL, Morland MR, Spector AA. 13-HODE increases intracellular calcium in vascular smooth muscle cells. Am J Physiol 1994; 266: C990–6.
Fritsche KL. Too much linoleic acid promotes inflammation-doesn't it? Prostaglandins Leukot Essent Fatty Acids 2008; 79: 173–5.
De Meyer GR, Bult H, Verbeuren TJ, Herman AG. The role of endothelial cells in the relaxations induced by 13-hydroxy- and 13-hydroperoxylinoleic acid in canine arteries. Br J Pharmacol 1992; 107: 597–603.
Obinata H, Izumi T. G2A as a receptor for oxidized free fatty acids. Prostaglandins Other Lipid Mediat 2009; 89: 66–72.
Hattori T, Obinata H, Ogawa A, Kishi M, Tatei K, Ishikawa O, et al. G2A plays proinflammatory roles in human keratinocytes under oxidative stress as a receptor for 9-hydroxyoctadecadienoic acid. J Invest Dermatol 2008; 128: 1123–33.
Buchanan MR, Haas TA, Lagarde M, Guichardant M. 13-Hydroxyoctadecadienoic acid is the vessel wall chemorepellant factor, LOX. J Biol Chem 1985; 260: 16056–9.
Theken KN, Schuck RN, Edin ML, Tran B, Ellis K, Bass A, et al. Evaluation of cytochrome P450-derived eicosanoids in humans with stable atherosclerotic cardiovascular disease. Atherosclerosis 2012; 222: 530–6.
Ricciotti E, FitzGerald GA. Prostaglandins and inflammation. Arterioscler Thromb Vasc Biol 2011; 31: 986–1000.
Tam VC. Lipidomic profiling of bioactive lipids by mass spectrometry during microbial infections. Semin Immunol 2013; 25: 240–8.
Sha W, Brune B, Weigert A. The multi-faceted roles of prostaglandin E2 in cancer-infiltrating mononuclear phagocyte biology. Immunobiology 2012; 217: 1225–32.
Caligiuri SPB, Aukema HM, Ravandi A, Lavallee R, Guzman R, Pierce GN. Specific plasma oxylipins increase the odds of cardiovascular and cerebrovascular events in patients with peripheral artery disease. Can J Physiol Pharmacol 2017; 95: 961–8.
Caligiuri SP, Rodriguez-Leyva D, Aukema HM, Ravandi A, Weighell W, Guzman R, et al. Dietary flaxseed reduces central aortic blood pressure without cardiac involvement but through changes in plasma oxylipins. Hypertension 2016; 68: 1031–8.
Kuhn H, Banthiya S, van Leyen K. Mammalian lipoxygenases and their biological relevance. Biochim Biophys Acta 2015; 1851: 308–30.
Adams JW, Sah VP, Henderson SA, Brown JH. Tyrosine kinase and c-Jun NH2-terminal kinase mediate hypertrophic responses to prostaglandin F2alpha in cultured neonatal rat ventricular myocytes. Circ Res 1998; 83: 167–78.
Gunter BR, Butler KA, Wallace RL, Smith SM, Harirforoosh S. Non-steroidal anti-inflammatory drug-induced cardiovascular adverse events: a meta-analysis. J Clin Pharm Ther 2017; 42: 27–38.
Cheng Y, Austin SC, Rocca B, Koller BH, Coffman TM, Grosser T, et al. Role of prostacyclin in the cardiovascular response to thromboxane A2. Science 2002; 296: 539–41.
Pradhan I, Ledent C, Mustafa SJ, Morisseau C, Nayeem MA. High salt diet modulates vascular response in A2AAR (+/+) and A 2AAR (−/−) mice: role of sEH, PPARgamma, and KATP channels. Mol Cell Biochem 2015; 404: 87–96.
Renda G, Zimarino M, Antonucci I, Tatasciore A, Ruggieri B, Bucciarelli T, et al. Genetic determinants of blood pressure responses to caffeine drinking. Am J Clin Nutr 2012; 95: 241–8.
Zhai YJ, Liu P, He HR, Zheng XW, Wang Y, Yang QT, et al. The association of ADORA2A and ADORA2B polymorphisms with the risk and severity of chronic heart failure: a case-control study of a northern Chinese population. Int J Mol Sci 2015; 16: 2732–46.
Beshay N.M, Zordoky AOSE-K. Effect of cytochrome P450 polymorphism on arachidonic acid metabolism and their impact on cardiovascular diseases. Pharmacol Ther 2010; 125: 446–63.
Arun Kumar AS, Kumar SS, Umamaheswaran G, Kesavan R, Balachandar J, Adithan C. Association of CYP2C8, CYP2C9 and CYP2J2 gene polymorphisms with myocardial infarction in South Indian population. Pharmacol Rep 2015; 67: 97–101.
Sandberg M, Hassett C, Adman ET, Meijer J, Omiecinski CJ. Identification and functional characterization of human soluble epoxide hydrolase genetic polymorphisms. J Biol Chem 2000; 275: 28873–81.
Ledent C, Vaugeois JM, Schiffmann SN, Pedrazzini T, El Yacoubi M, Vanderhaeghen JJ, et al. Aggressiveness, hypoalgesia and high blood pressure in mice lacking the adenosine A2a receptor. Nature 1997; 388: 674–8.
Athirakul K, Bradbury Dagger JA, Graves JP, Degraff LM, Ma J, Zhao Y, et al. Increased blood pressure in mice lacking cytochrome P450 2J5. Faseb J 2008; 22: 4096–108.
Seubert JM, Xu F, Graves JP, Collins JB, Sieber SO, Paules RS, et al. Differential renal gene expression in prehypertensive and hypertensive spontaneously hypertensive rats. Am J Physiol Renal Physiol 2005; 289: F552–61.
Ai D, Fu Y, Guo D, Tanaka H, Wang N, Tang C, et al. Angiotensin II up-regulates soluble epoxide hydrolase in vascular endothelium in vitro and in vivo. Proc Natl Acad Sci U S A 2007; 104: 9018–23.
Honetschlagerova Z, Sporkova A, Kopkan L, Huskova Z, Hwang SH, Hammock BD, et al. Inhibition of soluble epoxide hydrolase improves the impaired pressure-natriuresis relationship and attenuates the development of hypertension and hypertension-associated end-organ damage in Cyp1a1-Ren-2 transgenic rats. J Hypertens 2011; 29: 1590–601.
Ponnoth DS, Nayeem MA, Tilley SL, Ledent C, Jamal Mustafa S. CYP-epoxygenases contribute to A2A receptor-mediated aortic relaxation via sarcolemmal KATP channels. Am J Physiol Regul Integr Comp Physiol 2012; 303: R1003–10.
Zordoky BN, El-Kadi AO. Effect of cytochrome P450 polymorphism on arachidonic acid metabolism and their impact on cardiovascular diseases. Pharmacol Ther 2010; 125: 446–63.
Dai D, Zeldin DC, Blaisdell JA, Chanas B, Coulter SJ, Ghanayem BI, et al. Polymorphisms in human CYP2C8 decrease metabolism of the anticancer drug paclitaxel and arachidonic acid. Pharmacogenetics 2001; 11: 597–607.
Goldstein JA. Clinical relevance of genetic polymorphisms in the human CYP2C subfamily. Br J Clin Pharmacol 2001; 52: 349–55.
Goldstein JA, Ishizaki T, Chiba K, de Morais SM, Bell D, Krahn PM, et al. Frequencies of the defective CYP2C19 alleles responsible for the mephenytoin poor metabolizer phenotype in various Oriental, Caucasian, Saudi Arabian and American black populations. Pharmacogenetics 1997; 7: 59–64.
Kaur-Knudsen D, Bojesen SE, Nordestgaard BG. Common polymorphisms in CYP2C9, subclinical atherosclerosis and risk of ischemic vascular disease in 52,000 individuals. Pharmacogenomics J 2009; 9: 327–32.
Mizutani T. PM frequencies of major CYPs in Asians and Caucasians. Drug Metab Rev 2003; 35: 99–106.
Rodriguez-Antona C, Gomez A, Karlgren M, Sim SC, Ingelman-Sundberg M. Molecular genetics and epigenetics of the cytochrome P450 gene family and its relevance for cancer risk and treatment. Hum Genet 2010; 127: 1–17.
Ercan B, Ayaz L, Cicek D, Tamer L. Role of CYP2C9 and CYP2C19 polymorphisms in patients with atherosclerosis. Cell Biochem Funct 2008; 26: 309–13.
King LM, Gainer JV, David GL, Dai D, Goldstein JA, Brown NJ, et al. Single nucleotide polymorphisms in the CYP2J2 and CYP2C8 genes and the risk of hypertension. Pharmacogenet Genomics 2005; 15: 7–13.
King LM, Ma J, Srettabunjong S, Graves J, Bradbury JA, Li L, et al. Cloning of CYP2J2 gene and identification of functional polymorphisms. Mol Pharmacol 2002; 61: 840–52.
Spiecker M, Darius H, Hankeln T, Soufi M, Sattler AM, Schaefer JR, et al. Risk of coronary artery disease associated with polymorphism of the cytochrome P450 epoxygenase CYP2J2. Circulation 2004; 110: 2132–6.
Spiecker M, Liao J. Cytochrome P450 epoxygenase CYP2J2 and the risk of coronary artery disease. Trends Cardiovasc Med 2006; 16: 204–8.
Koerner IP, Jacks R, DeBarber AE, Koop D, Mao P, Grant DF, et al. Polymorphisms in the human soluble epoxide hydrolase gene EPHX2 linked to neuronal survival after ischemic injury. J Neurosci 2007; 27: 4642–9.
Gainer JV, Bellamine A, Dawson EP, Womble KE, Grant SW, Wang Y, et al. Functional variant of CYP4A11 20-hydroxyeicosatetraenoic acid synthase is associated with essential hypertension. Circulation 2005; 111: 63–9.
Ward NC, Tsai IJ, Barden A, van Bockxmeer FM, Puddey IB, Hodgson JM, et al. A single nucleotide polymorphism in the CYP4F2 but not CYP4A11 gene is associated with increased 20-HETE excretion and blood pressure. Hypertension 2008; 51: 1393–8.
Stec DE, Roman RJ, Flasch A, Rieder MJ. Functional polymorphism in human CYP4F2 decreases 20-HETE production. Physiol Genomics 2007; 30: 74–81.
Burhop KE, Selig WM, Malik AB. Monohydroxyeicosatetraenoic acids (5-HETE and 15-HETE) induce pulmonary vasoconstriction and edema. Circ Res 1988; 62: 687–98.
Hoopes SL, Garcia V, Edin ML, Schwartzman ML, Zeldin DC. Vascular actions of 20-HETE. Prostaglandins Other Lipid Mediat 2015; 120: 9–16.
Dunn KM, Renic M, Flasch AK, Harder DR, Falck J, Roman RJ. Elevated production of 20-HETE in the cerebral vasculature contributes to severity of ischemic stroke and oxidative stress in spontaneously hypertensive rats. Am J Physiol Heart Circ Physiol 2008; 295: H2455–65.
Cheng J, Ou JS, Singh H, Falck JR, Narsimhaswamy D, Pritchard KA Jr. et al. 20-hydroxyeicosatetraenoic acid causes endothelial dysfunction via eNOS uncoupling. Am J Physiol Heart Circ Physiol 2008; 294: H1018–26.
Waldman M, Peterson SJ, Arad M, Hochhauser E. The role of 20-HETE in cardiovascular diseases and its risk factors. Prostaglandins Other Lipid Mediat 2016; 125: 108–17.
Yadav VR, Zeldin DC, Mustafa SJ, Xie S, Nayeem MA. Soluble epoxide hydrolase modulates adenosine receptor-induced vascular response in mouse mesenteric arteries. FASEB J 2015; 29: 783.5.
Yang H, Fu Z, Ma Y, Huang D, Zhu Q, Erdenbat C, et al. CYP4A11 gene T8590C polymorphism is associated with essential hypertension in the male western Chinese Han population. Clin Exp Hypertens 2014; 36: 398–403.
Fu Z, Yang H, Ma Y, Huang D, Xie X, Zheng Y, et al. Haplotype study of the CYP4A11 gene and coronary artery disease in Han and Uygur populations in China. Gene 2013; 512: 510–6.
Fu Z, Nakayama T, Sato N, Izumi Y, Kasamaki Y, Shindo A, et al. Haplotype-based case-control study of CYP4A11 gene and myocardial infarction. Hereditas 2012; 149: 91–8.
Zhang W, Davis CM, Edin ML, Lee CR, Zeldin DC, Alkayed NJ. Role of endothelial soluble epoxide hydrolase in cerebrovascular function and ischemic injury. PLoS One 2013; 8: e61244.
Edin ML, Wang Z, Bradbury JA, Graves JP, Lih FB, DeGraff LM, et al. Endothelial expression of human cytochrome P450 epoxygenase CYP2C8 increases susceptibility to ischemia-reperfusion injury in isolated mouse heart. FASEB J 2011; 25: 3436–47.
Moghaddam MF, Grant DF, Cheek JM, Greene JF, Williamson KC, Hammock BD. Bioactivation of leukotoxins to their toxic diols by epoxide hydrolase. Nat Med 1997; 3: 562–6.
Coffman JD, Gregg DE. Reactive hyperemia characteristics of the myocardium. Am J Physiol 1960; 199: 1143–9.
Fang X, Weintraub NL, McCaw RB, Hu S, Harmon SD, Rice JB, et al. Effect of soluble epoxide hydrolase inhibition on epoxyeicosatrienoic acid metabolism in human blood vessels. Am J Physiol Heart Circ Physiol 2004; 287: H2412–20.
Fang X, Kaduce TL, Weintraub NL, Harmon S, Teesch LM, Morisseau C, et al. Pathways of epoxyeicosatrienoic acid metabolism in endothelial cells. Implications for the vascular effects of soluble epoxide hydrolase inhibition. J Biol Chem 2001; 276: 14867–74.
Li R, Xu X, Chen C, Yu X, Edin ML, Degraff LM, et al. Cytochrome P450 2J2 is protective against global cerebral ischemia in transgenic mice. Prostaglandins Other Lipid Mediat 2012; 99: 68–78.
Chen W, Yang S, Ping W, Fu X, Xu Q, Wang J. CYP2J2 and EETs protect against lung ischemia/reperfusion injury via anti-inflammatory effects in vivo and in vitro. Cell Physiol Biochem 2015; 35: 2043–54.
Jia J, Davis CM, Zhang W, Edin ML, Jouihan S, Jia T, et al. Sex- and isoform-specific mechanism of neuroprotection by transgenic expression of P450 epoxygenase in vascular endothelium. Exp Neurol 2016; 279: 75–85.
Larsen BT, Miura H, Hatoum OA, Campbell WB, Hammock BD, Zeldin DC, et al. Epoxyeicosatrienoic and dihydroxyeicosatrienoic acids dilate human coronary arterioles via BK(Ca) channels: implications for soluble epoxide hydrolase inhibition. Am J Physiol Heart Circ Physiol 2006; 290: H491–9.
Marciante KD, Totah RA, Heckbert SR, Smith NL, Lemaitre RN, Lumley T, et al. Common variation in cytochrome P450 epoxygenase genes and the risk of incident nonfatal myocardial infarction and ischemic stroke. Pharmacogenet Genomics 2008; 18: 535–43.
Mobert J, Becker BF, Zahler S, Gerlach E. Hemodynamic effects of isoprostanes (8-iso-prostaglandin F2alpha and E2) in isolated guinea pig hearts. J Cardiovasc Pharmacol 1997; 29: 789–94.
Acknowledgements
This work was supported by National Institutes of Health's grant HL-114559 to M A NAYEEM.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nayeem, M.A. Role of oxylipins in cardiovascular diseases. Acta Pharmacol Sin 39, 1142–1154 (2018). https://doi.org/10.1038/aps.2018.24
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2018.24
Keywords
This article is cited by
-
The effect of canagliflozin on gut microbiota and metabolites in type 2 diabetic mice
Genes & Genomics (2024)
-
Plasma metabolomic characterization of premature ovarian insufficiency
Journal of Ovarian Research (2023)
-
Effect of cardiopulmonary bypass on plasma and erythrocytes oxylipins
Lipids in Health and Disease (2023)
-
Senescence-associated 13-HODE production promotes age-related liver steatosis by directly inhibiting catalase activity
Nature Communications (2023)
-
A Targeted Lipidomic Reveals CYP450-Derived Oxylipin Linked to the Inflammatory Response by Polycyclic Aromatic Hydrocarbon Exposure in Children
Exposure and Health (2023)