Abstract
Anlotinib is a new oral tyrosine kinase inhibitor; this study was designed to characterize its pharmacokinetics and disposition. Anlotinib was evaluated in rats, tumor-bearing mice, and dogs and also assessed in vitro to characterize its pharmacokinetics and disposition and drug interaction potential. Samples were analyzed by liquid chromatography/mass spectrometry. Anlotinib, having good membrane permeability, was rapidly absorbed with oral bioavailability of 28%–58% in rats and 41%–77% in dogs. Terminal half-life of anlotinib in dogs (22.8±11.0 h) was longer than that in rats (5.1±1.6 h). This difference appeared to be mainly associated with an interspecies difference in total plasma clearance (rats, 5.35±1.31 L·h−1·kg−1; dogs, 0.40±0.06 L·h−1/kg−1). Cytochrome P450-mediated metabolism was probably the major elimination pathway. Human CYP3A had the greatest metabolic capability with other human P450s playing minor roles. Anlotinib exhibited large apparent volumes of distribution in rats (27.6±3.1 L/kg) and dogs (6.6±2.5 L/kg) and was highly bound in rat (97%), dog (96%), and human plasma (93%). In human plasma, anlotinib was predominantly bound to albumin and lipoproteins, rather than to α1-acid glycoprotein or γ-globulins. Concentrations of anlotinib in various tissue homogenates of rat and in those of tumor-bearing mouse were significantly higher than the associated plasma concentrations. Anlotinib exhibited limited in vitro potency to inhibit many human P450s, UDP-glucuronosyltransferases, and transporters, except for CYP3A4 and CYP2C9 (in vitro half maximum inhibitory concentrations, <1 μmol/L). Based on early reported human pharmacokinetics, drug interaction indices were 0.16 for CYP3A4 and 0.02 for CYP2C9, suggesting that anlotinib had a low propensity to precipitate drug interactions on these enzymes. Anlotinib exhibits many pharmacokinetic characteristics similar to other tyrosine kinase inhibitors, except for terminal half-life, interactions with drug metabolizing enzymes and transporters, and plasma protein binding.
Similar content being viewed by others
Introduction
Tyrosine kinases are key components of signal transduction pathways in the cell that relay information about conditions in the extracellular domain or the cytoplasm to pass on to the nucleus. Many tumor cells show abnormal activity of specific tyrosine kinases1. To control such abnormal activity, a major effort has been made to discover small-molecule inhibitors that can block the phosphorylation mediated by the tyrosine kinases. Molecularly targeted therapies based on tyrosine kinase inhibitors normally have a higher specificity toward tumor cells and less toxicity compared with cytotoxic chemotherapy. Clinical success of tyrosine kinase inhibitors in various advanced refractory tumors has established a paradigm for the treatment of tumors whose growth is acutely dependent on specific kinase targets2.
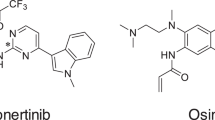
Anlotinib (AL3818), known as 1-[[[4-(4-fluoro-2-methyl-1H-indol-5-yloxy)-6-methoxyquinolin-7-yl]oxy]methyl]cyclopropanamine, is a novel multi-targeted tyrosine kinase inhibitor (details pending publication elsewhere). Anlotinib was found to suppress tumor development mainly through inhibition of VEGFR2 with a half maximum inhibitory concentration of 0.2 nmol/L; it inhibited tumor angiogenesis in vitro and in vivo. Oral administration of anlotinib resulted in reduced growth of several established human tumor xenografts in nude mice with little toxicity. A recent phase I study in patients with advanced refractory solid tumors (ClinicalTrials.gov Identifier: NCT01833923, at https://clinicaltrials.gov/) indicated that anlotinib, at the dose of 12 mg once daily at the 2-week on/1-week off schedule, displayed manageable toxicity, long circulation, and broad-spectrum antitumor potential3. More recently, a randomized, double-blind, placebo-controlled, multi-centered phase III study in 437 patients with advanced non-small cell lung cancer (NCT02388919) suggested that treatment with anlotinib could be promising, given significantly prolonged median overall survival (9.6 months versus 6.3 months for the anlotinib-treated and control groups, respectively)4. Currently, additional clinical studies are ongoing in a variety of malignancies including metastatic colorectal cancer (phase III; NCT02332499), medullary thyroid carcinoma (phase II; NCT02586350), differentiated thyroid carcinoma (phase II; NCT02586337), soft tissue sarcoma (phase II; NCT02449343), renal clear cell cancer (phase II; NCT02072031), gastric cancer (phase II; NCT02461407), esophageal squamous cell carcinoma (phase II; NCT02649361), and hepatocellular carcinoma (phase II; NCT02809534).
To evaluate the drug-like properties of anlotinib and to support associated safety and anticancer effect assessment in experimental animals and the follow-up clinical trials, pharmacokinetic studies in rats, tumor-bearing mice, and dogs, as well as associated in vitro studies, were performed to assess the compound's absorption, distribution, metabolism, and excretion. These experimental animal species were also used in nonclinical evaluation of safety or anticancer effects of anlotinib. This report describes findings from the preclinical pharmacokinetic studies.
Materials and methods
Chemicals and materials
Anlotinib (dihydrochloride form; purity >99%) used in animal studies and reference standard of anlotinib (dihydrochloride form; purity >99%) for analysis use were obtained from Jiangsu Chia-tai Tianqing Pharmaceutical Co, Ltd (Nanjing, China). For oral and intravenous administration to rats and dogs, anlotinib was dissolved in physiological saline to a variety of concentrations.
Sodium heparin, isoflurane, saline, and taurocholic acid were obtained from Sinopharm Chemical Reagent Co, Ltd (Shanghai, China). Pentobarbital was obtained from Shanghai Westang Biotechnology (Shanghai, China). Vardenafil hydrochloride, antipyrine, atenolol, imatinib mesylate, rhodamine 123, sulfasalazine, verapamil, MK571, novobiocin, Hank's balanced salt solution, nicotinamide adenine dinucleotide phosphate, glucose-6-phosphate, phenacetin, coumarin, bupropion, amodiaquine, diclofenac, (S)-mephenytoin, dextrorphan, chlorzoxazone, gluocose-6-phosphate monosodium salt, β-estradiol, trifluoperazine, 4-methylumbelliferone, β-estradiol-3-β-D-glucuronide, trifluoperazine-N-β-D-glucuronide, 4-methylumbelliferyl-β-D-glucuronide, atazanavir, hecogenin, phenylbutazone, niflumic acid, alamethicin, Uridine 5′-diphosphoglucuronic acid (UDPGA), estradiol-17β-D-glucuronide, estrone-3-sulfate, para-aminohippuric acid, tetraethylammonium, methotrexate, cimetidine, probenecid, rifampin, and ethyl acetate were obtained from Sigma-Aldrich (St Louis, MO, USA). Senkyunolides I were obtained from Shanghai Standard Technology (Shanghai, China). Tariquidar was obtained from Selleck (Houston, TX, USA). Ginsenoside Rg1 and midazolam was obtained from the National Institutes for Food and Drug Control (Beijing, China). HPLC-grade acetonitrile, formic acid, and methanol were obtained from Merck (Darmstadt, Germany). HPLC-grade water was prepared using a Millipore Milli-Q integral water purifying system (Bedford, MA, USA).
Human colon carcinoma (Caco-2) cells and human embryonic kidney 293 (HEK-293) cells were obtained from American Type Culture Collection (Manassas, VA, USA). Dulbecco's modified Eagle's medium, penicillin-streptomycin, and nonessential amino acids were obtained from Gibco Invitrogen Cell Culture (Grand Island, NY, USA). Fetal bovine serum was obtained from Corning Gentest (Woburn, MA, USA). Pooled human liver microsomes, cDNA-expressed human cytochrome P450 (P450) enzymes (CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP2E1, CYP3A4, and CYP3A5), and CYP enzymes high throughput inhibitor screening kits of CYP1A2/CEC, CYP2B6/EFC, CYP2C8/DBF, CYP2C9/MFC, CYP2C19/CEC, CYP2D6/AMMC, and CYP3A4/BFC were obtained from Corning Gentest. Baculovirus insect cell-expressed human uridine 5′-diphosphoglucuronosyltransferases (UGT1A1, UGT1A3, UGT1A4, UGT1A6, UGT1A9, UGT2B7, and UGT2B15) was obtained also from Corning Gentest. Rat liver microsomes and dog liver microsomes were prepared in house. Full open reading frames of cDNA for human organic anion-transporting polypeptide (OATP) 1B1, human OATP1B3, human organic anion transporter (OAT) 1, human OAT3, and human organic cation transporter (OCT) 2 were synthesized and subcloned into pcDNA 3.1(+) expression vectors by Invitrogen Life Technologies (Shanghai, China). Prior to the study, all expression plasmids were sequence-verified according to their GeneBank accession numbers (human OATP1B1, NM_006446; human OATP1B3, NM_019844; human OAT1, NM_004790; human OAT3, NM_004254; human OCT2, NM_003058). Inside-out membrane vesicles (5 mg protein/mL), prepared from insect cells expressing human multidrug resistance 1 (MDR1), multidrug resistance-associated protein 2 (MRP1), or human breast cancer resistance protein (BCRP), were purchased from Genomembrane (Kanazawa, Ishikawa Prefecture, Japan). Lyophilized albumin (prepared from human plasma; purity ≥95%), lyophilized α1-acid glycoprotein (prepared from human plasma; purity >95%), high density lipoproteins (prepared from human plasma; purity >95%), low density lipoproteins (prepared from human plasma; purity >95%), and very low density lipoproteins (prepared from human plasma; purity >95%) were obtained from Athens Research & Technology (Athens, GA, USA). γ-Globulins (prepared from human blood; purity >99%) were obtained from Sigma-Aldrich.
Spectra/Por1 2 RC dialysis membranes (cellulose tubing, 15 m×6.4 mm id) with a molecular weight cutoff of 12–14 kDa were obtained from Spectrum Laboratories Inc (Rancho Dominguez, CA, USA). Millicell-PCF filter inserts (0.4-μm, 12-mm diameter) were obtained from Millipore (Bedford, MA, USA).
Experimental animals
All animal care and use complied with the Guidance for Ethical Treatment of Laboratory Animals (The Ministry of Science and Technology of China, 2006, at www.most.gov.cn/fggw/zfwj/zfwj2006). All animal studies were implemented according to protocols, which were reviewed and approved by the Institutional Animal Care and Use Committee at Shanghai Institute of Materia Medica (Shanghai, China). Male and female Sprague Dawley rats (230–270 g) were obtained from SIPPR-BK Laboratory Animal Co Ltd (Shanghai, China). Female Balb/cA nude mice (18–20 g) were obtained from Shanghai Laboratory Animal Center (Shanghai, China). Nude mice were inoculated subcutaneously with 5×106 human colon cancer SW620 cells to establish a human tumor xenograft; the tumor-bearing mice were used when the tumors reached a volume of 400–600 mm3. Male and female beagle dogs (7–9 kg) were obtained from School of Agriculture and Biology, Shanghai Jiao Tong University (Shanghai, China). The animals were maintained on controlled temperature (20–24 °C), relative humidity (40%–70%), and a 12-h cycle of light and dark. The animals were given commercial diets, except for an overnight fasting period before dosing, and filtered tap water ad libitum. The rats and mice were acclimated to the facilities for 1 week before use and the dogs for 2 weeks. A total of 118 rats, 60 nude mice, and 24 dogs were used in the experiments described here.
Rat studies
Rats were randomly assigned to four groups (five male and five female rats per group) to receive a single oral dose of anlotinib at 1.5, 3, or 6 mg/kg (via gavage) or a single intravenous dose at 1.5 mg/kg (from the tail vein). Serial blood samples (around 0.25 mL; before and 5, 15, and 30 min and 1, 2, 4, 6, 8, 11, and 24 h after dosing) were collected in heparinized tubes from the orbital sinuses of rats under isoflurane anesthesia and centrifuged at 1300×g for 10 min to yield plasma fractions.
Rats under isoflurane anesthesia were killed by bleeding from the abdominal aorta at 1, 4, 8, and 24 h (three male and three female rats per time point) after a single oral dose of anlotinib at 3 mg/kg. The blood of rats was collected in heparinized evacuated blood collection tubes and centrifuged to yield plasma fractions. The testicles (male only), ovaries (female only), wombs (female only), bladders, adiposes, kidneys, adrenal glands, spleens, pancreases, stomachs, small intestines, colons, livers, hearts, lungs, brains, skeletal muscles, and femur bones were excised from the rats, rinsed in ice-cold saline, blotted, and weighed. The collected tissues were homogenized in four-fold volume of ice-cold water, except for the ovary, adipose, bladder, and adrenal glands, which were homogenized in 9-, 9-, 19-, and 29-fold volumes of ice-cold water, respectively.
Three male and three female rats were housed singly in metabolic cages with the urine collection tubes frozen at −15 °C during sample collection. Urine and feces samples were collected from rats before and 0–4, 4–10, and 10–24 h after a single intravenous dose of anlotinib at 1.5 mg/kg and weighed.
Three male and three female rats received in-house bile-duct-cannulation under pentobarbital anesthesia and were allowed to regain their preoperative body weights before use. Serial bile samples were collected before and 0–3, 3–6, 6–9, 9–12, 12–18, and 18–24 h after a single intravenous dose of anlotinib at 1.5 mg/kg and weighed.
All rat samples were stored at −70 °C pending analysis.
Tumor-bearing mouse studies
Female tumor-bearing mice were randomly assigned to three groups (20 mice per group) to receive a single oral dose of anlotinib at 0.75, 1.5, or 3 mg/kg (via gavage). Mice under isoflurane anesthesia were killed by bleeding from the orbital sinus at 2, 4, 8, and 24 h (five mice per time point) after dosing. The blood of mice was collected in heparinized tubes and centrifuged to yield plasma fractions. The lungs, livers, kidneys, colons, and tumor tissues were excised from the mice, rinsed in ice-cold saline, blotted, and weighed. The collected tissues were homogenized in four-fold volume of ice-cold water, except for the lungs, which were homogenized in nine-fold volumes of ice-cold water.
All mouse samples were stored at −70 °C pending analysis.
Dog study
Dogs were randomly assigned to four groups (three male and three female dogs per group) to receive a single oral dose of anlotinib at 0.5, 1, or 2 mg/kg (via gavage) or a single intravenous dose at 0.5 mg/kg (from left forelimb vein). Serial blood samples (around 0.5 mL; before and 5, 15, and 30 min and 1, 2, 4, 6, 8, 11, and 24 h after dosing) were collected in heparinized tubes from the right forelimb vein of dogs and centrifuged to yield plasma fractions.
All dog plasma samples were stored at −70 °C pending analysis.
In vitro assessment of pharmacokinetic and related physicochemical properties
Binding of anlotinib in plasma was assessed by a method of equilibrium dialysis [10 h at 37 °C; using Spectra/Por1 2 RC dialysis membranes with a molecular weight cutoff of 12–14 kDa and phosphate buffered saline (pH 7.4) as dialysate]5. Anlotinib was spiked into blank rat, dog, or human plasma to generate concentrations of 276, 552, and 1104 ng/mL. After completion of dialysis, the concentrations of anlotinib in the dialysate and plasma samples were measured. The unbound fraction in plasma (fu) was calculated using the following equation:

where Cu is the concentration (ng/mL) of anlotinib in the dialysate compartment after completion of dialysis and Ct is the concentration (ng/mL) of anlotinib in the plasma compartment after completion of dialysis. To understand the proteins responsible for the binding in human plasma, anlotinib, at the concentrations 100, 200, 400, and 800 ng/mL, was assessed in solutions of the isolated human plasma proteins albumin (600 μmol/L), α1-acid glycoprotein (10 μmol/L), γ-globulins (80 μmol/L), high density lipoproteins (10 μmol/L), low density lipoproteins (1 μmol/L), and very low density lipoproteins (0.1 μmol/L) using the equilibrium dialysis method. Imatinib was used as a control. The total binding constant (nK; L/μmol) was calculated using the following equation6:

where Ct is the concentration (ng/mL) of anlotinib in the solution of the isolated human plasma protein(s) after completion of dialysis, Cu is the concentration (ng/mL) of anlotinib in the dialysate compartment after completion of dialysis, and [P] is the protein concentration in the solution of the isolated human plasma protein(s). An nKα1-acid-glycoprotein/nKalbumin ratio (nK ratio) was used to indicate comparative binding to α1-acid glycoprotein and to albumin; an nK ratio of <7.7 was not considered to be large enough for a tyrosine kinase inhibitor to compensate the high excess of plasma concentration of albumin (600 μmol/L) over α1-acid glycoprotein (20 μmol/L)7.
Membrane permeability of anlotinib was assessed using Caco-2 cell monolayers. Caco-2 cells were cultured as previously described8. Caco-2 cell monolayers exhibited a transepithelial electrical resistance value of >400 Ω·cm2. The applicability of the cell monolayers was also evaluated using antipyrine (control compound of high membrane permeability), atenolol (control compound of low membrane permeability), rhodamine 123 (probe substrate of MDR1), sulfasalazine [probe substrate of multidrug resistance-associated protein 2 (MRP2)], estrone-3-sulfate (probe substrate of BCRP), verapamil (specific inhibitor of MDR1), MK571 (specific inhibitor of MRP2 and BCRP), and novobiocin (specific inhibitor of BCRP) before use. Bidirectional transport experiments were conducted in triplicate at 10 μmol/L for anlotinib in Hanks' balanced salt solution. After incubation at 37 °C, samples were collected from the receiver side at 60 min. Samples were also collected from the donor side at the last sampling time to determine recovery of anlotinib and the control compounds. The apparent permeability coefficient (Papp) expressed in cm/s was calculated using the following equation:

where ΔQ/Δt is the linear appearance rate of the test compounds on the receiver side in μmol/s; A is the surface area of the cell monolayer in cm2; and C0 is the initial concentration of the test compound on the donor compartment in μmol/L. According to our in-house Caco-2 cell monolayer data, compounds with Papp values <0.2×10−6, 0.2×10−6–2.8×10−6, and >2.8×10−6 cm/s were defined to be of low, intermediate, and high permeability, respectively9. An efflux ratio (Papp,B-A/Papp,A-B) was used to implicate possible involvement of transporter-mediated efflux, and an efflux ratio (EfR) >3 was considered to be a positive result.
Aqueous solubility of anlotinib in different media, including hydrochloric acid buffer at pH 1.7, acetate buffer at pH 4.6, and phosphate buffer at 6.5, was determined by an equilibrium shake flask thermodynamic solubility method10. Anlotinib was added to 2–5 mL of buffer media in a vial, which was shaken for 48 h at 37 °C. Undissolved anlotinib was separated by centrifugation. The concentration of anlotinib in the supernatant was measured in triplicate.
LogD values of anlotinib at pH 1.7, 4.6, and 6.5 in octanol/buffer solution system were measured by a shake-flask method10. After agitation for 36 h, concentration of anlotinib in the organic phase and the aqueous phase was measured in triplicate.
In vitro metabolism studies
To identify the human P450 isoforms that could mediate oxidation of anlotinib, a variety of cDNA-expressed human P450 enzymes (CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP2E1, CYP3A4, and CYP3A5), fortified with NADPH, were incubated with 2 μmol/L anlotinib at 37 °C for 60 min. The incubation was performed in duplicate and the enzyme concentration was 50 pmol P450/mL. After centrifugation at 3000×g for 10 min, the resulting supernatants were analyzed by liquid chromatography/mass spectrometry.
To compare interspecies difference in P450-mediated oxidation of anlotinib, the compound at the final concentration 2 μmol/L were incubated with rat liver microsomes, dog liver microsomes, and human liver microsomes in presence of NADPH. The incubations were performed in duplicate at 37 °C for 3, 7.5, 15, 30, or 60 min. The incubation conditions were the same as those described by Hu et al11. The interspecies differences were characterized with respect to metabolic stability and metabolite formation.
In vitro assessment of inhibitory effects of anlotinib on the activity of human drug metabolizing enzymes and that of human drug transporters
Potential for anlotinib to inhibit human P450 enzyme activity was evaluated using cDNA-expressed CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP3A4, and CYP3A5. 3-Cyano-7-ethoxycoumarin, 7-ethoxy-4-trifluoromethylcoumarin, dibenzylfluorescein, 7-methoxy-4-trifluoromethylcoumarin, 3-[2-(N,N-diethyl-N-methylamino)ethyl]-7-methoxy-4-methylcoumarin, 7-benzyloxy-trifluoromethylcoumarin, and midazolam were used as probe substrates for CYP1A2/CYP2C19, CYP2B6, CYP2C8, CYP2C9, CYP2D6, CYP3A4, and CYP3A5, respectively, and the concentrations of these probe substrates in incubation mixtures were 5.0/25.0, 2.5, 1.0, 75.0, 1.5, 50.0, and 2.0 μmol/L, respectively. Initially, anlotinib, at 100 μmol/L in incubation mixture, was assessed in triplicate for its inhibitory effects on P450 enzymes' activity. When demonstrating >50% inhibition, the half maximal inhibitory concentration (IC50) of anlotinib was determined for the P450 enzymes. Each incubation mixture consisted of anlotinib, the cDNA-expressed P450 enzyme, and the associated probe substrate. The negative control mixture contained 0.2% methanol in place of anlotinib, whereas the positive control mixture contained a positive inhibitor in place of anlotinib. Positive control inhibitors for CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, and CYP3A4/CYP3A5 were furafylline, tranylcypromine, quercetin, sulfaphenazole, tranylcypromine, quinidine, and ketoconazole, respectively. The incubation mixture was equilibrated for 10 min before initiating the reaction by adding an NADPH-generating system, which comprised 3.3 mmol/L magnesium chloride, 3.3 mmol/L of glucose-6-phosphate, 0.5 U/mL glucose-6-phosphate dehydrogenase, and 1.3 mmol/L NADP. Incubation times were 10, 15, 30, 40, and 45 min for the CYP3A5-, CYP1A2-, CYP2B6-/CYP2C19-/CYP2D6-/CYP3A4-, CYP2C8-, and CYP2C9-mediated reactions, respectively. Enzymatic reactions were terminated with an equal volume of ice-cold acetonitrile, except for CYP2C8 using an equal volume of 2 mol/L sodium hydroxide solution to terminate the reaction followed by incubation at 37 °C for 2 h. A SpectraMax M2 microplate reader (Molecular Devices, Sunnyvale, CA, USA) was used to measure the fluorescent metabolites of the probe substrates at the selected excitation/emission wavelengths, ie, 410/460, 409/530, 485/538, and 390/460 nm/nm, for 3-cyano-7-hydroxycoumarin, 7-hydroxy-4-trifluoromethyllcoumarin, fluorescein, and 7-hydroxycoumarin/3-[2-(N,N-diethylamino)ethyl]-7-hydroxy-4-methylcoumarin, metabolites of the probe substrates for CYP1A2/CYP2C19, CYP2B6/CYP2C9/CYP3A4, CYP2C8, and CYP2D6, respectively. A liquid chromatography/mass spectrometry-based method was used to analyze 1'-hydroxymidazolam, the metabolite of the probe substrate midazolam for CYP3A5.
Potential for anlotinib to inhibit human UGT enzyme activity was evaluated using cDNA-expressed UGT1A1, UGT1A3, UGT1A4, UGT1A6, UGT1A9, UGT2B7, and UGT2B15. β-estradiol, 4-methylumbelliferone, trifluoperazine, and senkyunolide I were used as probe substrates for UGT1A1, UGT1A3/UGT1A6/UGT1A9/UGT2B7, UGT1A4, and UGT2B15, respectively, and the concentrations of these probe substrates in incubation mixtures were 20, 1000/100/10/300, 40, and 20 μmol/L, respectively. Initially, anlotinib, at 100 μmol/L in incubation mixture, was assessed in triplicate for its inhibitory effects on UGT enzymes' activity. When demonstrating >50% inhibition, the half maximal inhibitory concentration (IC50) of anlotinib was determined for the UGT enzymes. Each incubation mixture consisted of anlotinib, the cDNA-expressed UGT enzyme, alamethicin, and the associated probe substrate. The negative control mixture contained 0.2% methanol in place of anlotinib, whereas the positive control mixture contained a positive inhibitor in place of anlotinib. Positive control inhibitors for UGT1A1/UGT1A9, UGT1A3, UGT1A4, UGT1A6, and UGT2B7/UGT2B15 were niflumic acid, atazanavir, hecogenin, phenylbutazone, and diclofenac, respectively. The incubation mixture was equilibrated for 5 min before initiating the reaction by adding UDPGA. Incubation times were 30, 75, 20, 15, 120, and 20 min the UGT1A1-/UGT1A6-, UGT1A3-, UGT1A4-, UGT1A9-, UGT2B7-, and UGT2B15-mediated enzymatic reactions, respectively. These reactions were stopped by adding two volumes of ice-cold methanol followed by centrifugation at 1000×g for 10 min. The supernatants were analyzed, by liquid chromatography/mass spectrometry, to determine the quantity of the formed glucuronides, ie, E3G, 4-MUG, TFPG, and senkyunolide I-7-O-β-glucuronide for UGT1A1, UGT1A3/UGT1A6/UGT1A9/UGT2B7, UGT1A4, and UGT2B15, respectively.
To evaluate potential for anlotinib to inhibit human transporter activity, human organic anion-transporting polypeptide (OATP) 1B1, OATP1B3, human organic cation transporter (OCT) 2, human organic anion transporter (OAT) 1 and OAT3 plasmids and the empty vector were introduced separately into the HEK-293 cells with Lipofectamine 2000 transfection reagent (Invitrogen, Carlsbad, CA, USA) as previously described12,13. Initially, anlotinib, at 100 μmol/L in incubation mixture, was assessed for its inhibitory effects on activity of OATP1B1, OATP1B3, OCT2, OAT1, and OAT3, and the probe substrates used were estradiol-17β-D-glucuronide, para-aminohippuric acid, tetraethylammonium, and estrone-3-sulfate, respectively, with a concentration of 10 μmol/L in incubation mixtures for all. When demonstrating >50% inhibition, the IC50 of anlotinib was determined for the transporter. All experiments were run in triplicate. Concentrations of the probe substrates in the cells after incubation were determined by liquid chromatography/mass spectrometry.
Inhibitory effects of anlotinib on activity of human MDR1, MRP1, and BCRP were evaluated using membrane vesicles expressing the transporters and ginsenoside Rg1, estradiol-17β-D-glucuronide, and methotrexate, both at 10 μmol/L in incubation mixtures, were used as probe substrates, respectively. Initially, anlotinib, at 100 μmol/L in incubation mixture, was assessed for its inhibitory effects on activity of the transpoters. When demonstrating >50% inhibition, the IC50 of anlotinib was determined for the transporter. The details of vesicular transport methods with the probe substrates were described by Jiang et al12, and all experiments were run in triplicate. Quantity of the probe substrates trapped inside the vesicles after incubation was determined by liquid chromatography/mass spectrometry.
LC-MS-based bioanalytical assays
An Applied Biosystems Sciex API 4000 Q Trap mass spectrometer (Toronto, Ontario, Canada), interfaced via a Turbo V ion source with a Waters Acquity UPLC separation module (Milford, MA, USA), was used for analysis of unchanged and metabolized anlotinib in biological matrices. The chromatographic separation was achieved on a 5.0 μm Agilent Eclipse Plus C18 column (50 mm×2.1 mm id; Agilent, Chadds Ford, PA, USA). The mobile phase, delivered at 0.25 mL/min, consisted of acetonitrile/water (1:99, v/v, containing 5 mmol/L formic acid; solvent A) and acetonitrile/water (99:1, v/v, containing 5 mmol/L formic acid; solvent B). For quantification analysis, a gradient program was used, which consisted of 0–2 min from 5% B to 80% B, 2–3 min at 80% B, and 3–7 min at 5% B. For metabolite detection and characterization, a binary gradient method was used, ie, 0–10 min from 5% B to 25% B, 10–13 min from 25% B to 100% B, and 13–18 min at 5% B.
For quantification of anlotinib in various biological matrices, the instrument parameters for mass spectrometry were optimized in the positive ion mode to maximize generation of protonated ions for anlotinib and the internal standard vardenafil and to yield their characteristic product ions. The precursor-to-product ion pairs used for multiple-reaction-monitoring of anlotinib and the internal standard were m/z 408→339 (the optimized collision energy, 23 V) and 489→151 (69 V), respectively. Matrix-matched calibration curves were constructed using weighted (1/X) linear regression of the peak area of anlotinib to internal standard (Y) against the corresponding nominal anlotinib concentration (X, ng/mL). The assays were validated according to the China FDA guidance on bioanalytical validation (2014; http://www.sda.gov.cn/WS01/CL1616/101019.html) to demonstrate their reliability and reproducibility for the intended use. The assay's lower limits of quantification of anlotinib were 0.2–11.6 ng/mL. The intra-batch accuracy and precision were 85.2%–108.8% and 1.7%–16.0%, respectively, while inter-batch values were 99.0%–101.6% and 1.6%–5.3%, respectively.
Detection of anlotinib metabolites in biological matrices was facilitated by using the PALLAS MetabolExpert 3.7 software (CompuDrug International, Sedona, AZ, USA) and Accelrys metabolite database (version 2015.1; San Diego, CA, USA) to predict possible metabolic pathways of anlotinib and to generate a list of its phases I and II metabolite candidates with information regarding molecular mass gains and losses between metabolites and the parent compound. The detected anlotinib metabolites were initially characterized according to their fragmentation profiles compared with that of the parent compound or their diagnostic fragment ions or neutral losses. In addition, characterization of in vivo oxidized metabolites of anlotinib was also based on comparing their liquid chromatograph/mass spectrometry profiles with those of the respective in vitro metabolites formed by simulating the in vivo metabolic reactions using the same parent compound purified anlotinib, human P450 enzymes, and the cofactor NADPH.
For quantification of anlotinib in biological matrices, the samples were extracted with ethyl acetate. After centrifugation, the ethyl acetate extracts were reduced to dryness under a stream of N2 gas and the resulting residues were reconstituted in 50% methanol before analysis. For detection and characterization of anlotinib metabolites in biological matrices, the samples were precipitated with methanol. After centrifugation, the supernatants were applied to analysis.
Data processing
Plasma pharmacokinetic parameters of anlotinib were determined using non-compartmental analysis with Kinetica software (version 5.0; Thermo Scientific, Philadelphia, PA, USA). The maximum concentration (Cmax) and the time taken to achieve the peak concentration (Tpeak) after oral dose were obtained directly from the data without interpolation. The area under the concentration-time curve up to the last measured point in time (AUC0-t) was calculated using the trapezoidal rule. The total plasma clearance (CLtot,p) was estimated by dividing the dose by the AUC0-∞, and the distribution volume at steady state (VSS) was estimated by multiplying the CLtot,p by the mean residence time (MRT). The t1/2 was calculated using the relationship 0.693/ke. Oral bioavailability (F) was calculated by dividing the AUCoral by the AUCintravenous. Dose proportionality was assessed using the regression of log-transformed data (the Power Model), and the criteria was calculated according to a method by Smith et al.14. The fractions of dose excreted into urine (fe-U), feces (fe-F), and into bile (fe-B) were established using the relationships Cum.Ae-U/Dose, Cum.Ae-F/Dose, and Cum.Ae-B/Dose, respectively. IC50 values, in μmol/L, for inhibiting activity of a certain drug metabolizing enzyme or transporter were calculated using GraFit software (version 5.0; Erithacus Software, Surrey, UK). All data are expressed as the mean±standard deviation. Statistical analysis was performed using IBM SPSS Statistics software (version 19.0; IBM, Somers, NY, USA). A P value <0.05 was considered statistically significant.
Results
Plasma pharmacokinetics of anlotinib in rats and in dogs
Mean plasma concentrations of anlotinib over time after a single dose of anlotinib in rats and dogs are shown in Figure 1; the plasma pharmacokinetic parameters of anlotinib are summarized in Table 1. After oral administration, levels of systemic exposure to anlotinib, i.e., plasma maximum concentration (Cmax) and area under the plasma concentration-time curve up to 24 h (AUC0-24 h), in female rats tended to be greater than those in male rats at the tested dose range 1.5–6 mg/kg, while gender differences in plasma Cmax and AUC0-24 h of anlotinib were not significant in dogs at the dose range 0.5–2 mg/kg. The plasma Cmax and AUC0-24h increased as the anlotinib dose increased in an over-proportional manner in rats and dogs (Table 2). Anlotinib was highly bound in rat, dog, and human plasma with unbound fractions in plasma (fu) of 2.9%, 4.0%, and 7.3%, respectively. These fu values were independent of total plasma concentration of anlotinib, suggesting that such total concentration of anlotinib is a good measure of the changes in its unbound concentration in plasma for the species. As shown in Table 3, anlotinib exhibited binding affinity for α1-acid glycoprotein similar to imatinib, another tyrosine kinase inhibitor. However, it exhibited substantially higher affinity for albumin than imatinib. Unlike imatinib with an nKα1-acid-glycoprotein/nKalbumin ratio of 92.0, such a ratio for anlotinib was 0.9 (<7.7), suggesting the high excess of plasma concentration of albumin (600 μmol/L) over α1-acid glycoprotein (20 μmol/L) could not be compensated for circulating anlotinib in humans. It is worth mentioning that anlotinib exhibited notably higher affinity for plasma lipoproteins, particularly for low density lipoproteins and very low density lipoproteins, than for albumin and α1-acid glycoprotein. After oral administration, anlotinib was rapidly absorbed from the gastrointestinal tract in rats and dogs (Figure 1). Dogs tended to exhibit greater oral bioavailability (F) of anlotinib than rats. Terminal half-lives (t1/2) of anlotinib in rats and dogs after intravenous administration were comparable with the respective t1/2 values after oral administration. Dogs exhibited a longer mean t1/2 of anlotinib than rats. This t1/2 difference appeared to be attributed mainly to interspecies difference in total plasma clearance (CLtot,p). Anlotinib's mean apparent volume of distribution at steady state (VSS) in rats was 40 times as much as the rat volume of total body water and the value of VSS in dogs was 12 times as much as the dog volume of total body water15, suggesting the compound was distributed widely into various body fluids and tissues. In rats that received an intravenous dose of anlonitib, only small amounts of the unchanged compound were excreted into urine, bile, and feces (Table 1), suggesting that metabolism was the major elimination route of anlotinib.
Mean plasma concentrations of anlotinib over time in male rats (A), female rats (B), male dogs (C), and female dogs (D) after an oral or intravenous dose of anlotinib.
Intestinal absorption-related properties of anlotinib
Intestinal absorption of a drug is a combined result of its solubility in gastrointestinal fluids, membrane permeability, and substrate specificity to efflux system of the intestinal epithelia. Anlotinib exhibited pH-dependent aqueous solubility, ie, >1 g/mL at pH 1.7 (the stomach), 114 μg/mL at pH 4.6 (the duodenum), and 0.89 μg/mL at pH 6.5 (the jejunum and the ileum). The solubility values of anlotinib at pH 1.7 and 4.6 were greater than the compound's minimum solubility necessary to achieve adequate intestinal absorption at the dose 6 mg/kg, but the solubility value at pH 6.5 was lower than the minimum solubility. The minimum solubility was deduced according to a bar chart, by Lipinski, that depicts the minimum solubility for compounds with low, medium, and high permeability at doses of 0.1, 1, and 10 mg/kg16. Anlotinib exhibited good membrane permeability across Caco-2 cell monolayers, expressing MDR1, MRP2, and BCRP, with a mean apparent permeability coefficient (Papp) of 3.5×10−6 cm/s. The compound exhibited a mean efflux ratio (EfR) of 0.91±0.22, suggesting that its transport across the cell monolayer did not affected by the apical efflux transporters in Caco-2 cells (Supplementary Figure S1). Physicochemical properties of anlotinib (predicted using ACD/Percepta; Toronto, Ontario, Canada), ie, molecular mass (407 Da; favorable value, <500 Da), hydrogen-bonding capacity (HBA+HBD, 6+3; <12), topological polar surface area (TPSA, 82.4 Å2; <140 Å2), and molecular flexibility (NROTB, 6; <10), supported its good membrane permeability. Measured LogD values were −0.89 at pH 1.7, 2.10 at pH 4.6, and 2.38 at pH 6.5 (favorable range, 0–5).
Tissue distribution of anlotinib in rats and tumor-bearing mice
Levels of various tissue exposures to anlotinib (measured using associated tissue homogenate samples) in rats and tumor-bearing mice after an oral dose of the compound were significantly higher than the associated systemic exposure level (Figure 2). In rats, the lung exhibited the highest exposure level, which was 197 times as high as the systemic exposure level. Meanwhile, the rat liver, kidneys, and heart also exhibited high exposure levels, which were 49, 54, and 32 times as much as the systemic exposure level. Anlotinib penetrated the rat brain, with a brain homogenate AUC0-24h level comparable to the associated plasma level. In tumor-bearing mice, the level of tumor tissue exposure to the compound increased as the dose increased; it was 13 times as high as the systemic exposure level.
Tissue distribution of anlotinib in male rats (A), female rats (B), and female tumor-bearing mice (C–E) after an oral dose of anlotinib (3 mg/kg for rats, 0.75, 1.5, and 3 mg/kg for tumor-bearing mice).
Metabolism of anlotinib
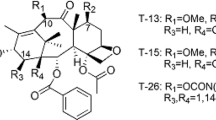
Because neither hepatobiliary nor renal excretion of unchanged compound was the main elimination route, metabolites of anlotinib in rat and dog samples were detected and characterized. As a result, a total of 12 anlotinib metabolites (M1–M12) were detected in the plasma, bile, urine, and feces samples of rats after dosing (Table 4). Eight of the metabolites, ie, M2, M4, M5, M6, M8, M9, M10, and M11, were found in plasma. All these metabolites occurred in rat bile and urine samples, except for M7 and M11, which occurred only in rat bile samples. In dogs, a total of 5 metabolites of anlotinib were detected in plasma samples; they were M4, M8, M9, M10, and M11. After liquid chromatography/mass spectrometry-based characterization of these metabolites, metabolic pathways of anlotinib were proposed (Figure 3). The major metabolic pathways of anlotinib in rats were probably the hydroxylation to form M10 and M11 and the dealkylation to form M8. The metabolites M10 and M11 were two major plasma metabolites of anlotinib in rats, while M8 was further glucuronized to form M6, a major plasma and biliary metabolite of anlotinib. To further characterize these metabolic pathways, in vitro metabolism studies were performed for anlotinib. As a result, multiple human cytochrome P450 enzymes, ie, CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP2E1, CYP3A4, and CYP3A5, were found to be able to mediate the oxidation of anlotinib to form M10, M11, and M8 (Figure 4A). Among these enzymes were CYP3A4 and CYP3A5 that exhibited the greatest metabolic capabilities. As shown in Figure 4B, the metabolites M10, M11, and M8 were also detected in samples of anlotinib after being incubated with NADPH-fortified rat liver microsomes, dog liver microsomes, and human liver microsomes under the same conditions. The total amounts of metabolites formed were different for the tested liver microsomes of different species, suggesting the highest oxidation rate by rat liver microsomes followed by dog liver microsomes, and then by human liver microsomes.
Proposed metabolic pathways of anlotinib. P450, cytochrome P450 enzymes; NADPH, reduced β-nicotinamide adenine dinucleotiden phosphate; NADP, β-nicotinamide adenine dinucleotide phosphate; UGT, uridine 5′-diphosphoglucuronosyltransferase; UDPGA, uridine 5′-diphosphoglucuronic acid; UDP, uridine 5′-diphosphate; SULT, sulfotransferase; PAPS, 3′-phosphoadenosine-5′-phosphosulphate; PAP, 3′-phosphoadenosine-5′-phosphate; Glu, glucuronosyl.
Human cytochrome P450 enzymes mediating in vitro oxidation of anlotinib (A) and comparative metabolic capabilities of liver microsomes of different species in mediating the metabolism (B–E). For the enzyme identification using cDNA-expressed human P450 enzymes, the substrate anlotinib and enzyme concentration were 2 μmol/L and 50 pmol P450/mL, respectively, with an incubation time of 60 min. The metabolites formed were expressed as relative abundance, with the most abundant M10 being 100% after incubation with CYP3A4. For the metabolic capability comparison using rat liver microsomes (B), dog liver microsomes (C), and human liver microsomes (D), the substrate anlotinib and enzyme concentration were 2 μmol/L and 0.5 mg protein/mL, respectively, with incubation times of 3, 7.5, 15, 30, and 60 min. The metabolites formed were expressed as relative abundance, with the most abundant M10 being 100% after incubation with rat liver microsomes for 30 min. Panel (E) shows comparative relative total abundance of M4, M5, M8, M9, M10, and M11 formed from anlotinib after incubation with NADPH-fortified rat liver microsomes, dog liver microsomes, and human liver microsomes. The chemical structures of formed metabolites were shown in Figure 3. Quantification of the oxidized metabolites was achieved using the calibration curve of anlotinib.
In vitro inhibitory activity of anlotinib on drug metabolism enzymes and transporters
As shown in Table 5, anlotinib exhibited, in vitro, significant potency to inhibit CYP3A4 and CYP2C9 with IC50 values of <1 μmol/L; such inhibitory potency towards CYP2C19, CYP2C8, UGT1A1, UGT1A4, UGT1A9, and UGT2B15 was moderate, with IC50 values of 1–10 μmol/L. This tyrosine kinase inhibitor exhibited low inhibitory potency in vitro towards human CYP2B6, CYP2D6, UGT1A6, UGT2B7, OATP1B1, OAT3, OCT2, MDR1, and BCRP with values of IC50 greater than 10 μmol/L. No significant inhibitory potency of anlotinib was found towards human CYP1A2, CYP3A5, OATP1B3, OAT1, and MRP1. Anlotinib was not an in vitro substrate of OATP1B1, OATP1B3, OAT1, OAT3, OCT2, MDR1, and BCRP (Supplementary Table S1).
Discussion
Anlotinib is a new and promising tyrosine kinase inhibitor that is likely to provide an additional medication to cancer therapy. Like many approved tyrosine kinase inhibitors, anlotinib exhibited pH-dependent hydrophilicity and lipophilicity. The compound was well soluble in acidic environment and had good membrane permeability measured at pH 7.4. Its aqueous solubility at pH 6.5 appeared to be too low to provide adequate absorption in the jejunum and the ileum. However, levels of systemic exposure to anlotinib in rats and dogs did not increase in any down-proportional manner as the oral dose increased to the highest levels. This suggested that the stomach and duodenum were probably the major absorption sites for oral anlotinib. In clinical practice, the gastrointestinal absorption of many tyrosine kinase inhibitors, including crizotinb, dasatinib, erlotinib, gefitinib, lapatinib, and pazopanib, can be substantially altered by concomitant administration of acid suppressive drugs, such as antacids, proton-pump inhibitors, and H2-antagonists17. A similar scenario is expected to take place with (for/in) anlotinib and, if possible, coadministration of this tyrosine kinase inhibitor with acid-suppressive drugs should be avoided. Rats and dogs exhibited an interspecies difference in oral bioavailability (F) of anlotinib. Because of the passive diffusion-based intestinal absorption (suggested by the Caco-2 data), the extensive hepatic uptake but limited hepatobiliary excretion (suggested by the rat data in Table 1), and the interspecies difference in extent of P450-mediated oxidation (suggested by the in vitro metabolism data in Figure 4), the F difference probably resulted mainly from the interspecies difference in the first-pass enterohepatic metabolic clearance. Absolute F of anlotinib has not been assessed in cancer patients3, because intravenous anlotinib was not available for the human study. Based on the interspecies differences in the in vitro metabolism (Figure 4), the human oral bioavailability of anlotinib was estimated at 41%–77%, which was higher than, or at least as high as, the dog oral bioavailability.
Consistent with its rapid intestinal absorption, anlotinib exhibited comparable values of terminal half-lives (t1/2), after intravenous and oral administration, in rats and dogs, suggesting that the t1/2 for oral administration reflected the compound's elimination rate during the terminal phase, rather than the absorption rate. In other words, flip-flop pharmacokinetics did not exist for orally administered anlotinib in rats and dogs. The t1/2 of anlotinib was significantly longer in dogs than in rats. Anlotinib exhibited, in both rats and dogs, large values of VSS, which were 40 and 12 times as much as the volumes of total body water of rat and dog, respectively15. Therefore, the preceding t1/2 difference between rats and dogs was mainly attributed to the interspecies difference in CLtot,p (Table 1). In vivo and in vitro pharmacokinetics and metabolism data suggested that cytochrome P450-mediated oxidation was the major elimination pathway of anlotinib and controlled the CLtot,p. Consistent with comparative metabolic capabilities of hepatic P450 mediating its oxidation: rat>dog>human, anlotinib exhibited, in patient volunteers with advanced refractory solid tumors, a very long t1/2 (96±17 h)3, which was also related to a large VSS and a slow CLtot,p. Anlotinib has a significantly longer t1/2 in cancer patients than most tyrosine kinase inhibitors approved to date (3–60 h)18. Based on this pharmacokinetic characteristic, a “two-week on/one-week off” dosage regimen was designed to achieve efficacy and safety in anlotinib-based cancer therapy3.
In rats and in tumor-bearing mice, total (unbound plus bound) concentrations of anlotinib in various tissues, including the tumor tissue, were significantly higher than the associated total (unbound plus bound) plasma concentrations. The higher total levels of tissue exposure to anlotinib were in agreement with large apparent volumes of distribution in the animals; this resulted from binding competition between the tissues and the plasma. Such binding competition is expected to take place in humans as well. The high total levels of tissue exposure do not imply high intracellular concentrations of unbound anlotinib in the tissues. The therapeutic intracellular unbound concentration of anlotinib in the tumor tissue is equal to the unbound plasma concentration under the distribution equilibrium condition. Accordingly, a change in unbound concentration of anlotinib in plasma has a large effect on its intracellular unbound concentration. Anlotinib was highly bound in human plasma with a fu of 7%; this binding was predominantly to albumin and lipoproteins, with other plasma proteins playing only a minor role. Affinity of anlotinib for lipoproteins, particularly for low density lipoproteins and very low density lipoproteins, was substantially higher than its affinity for albumin and α1-acid glycoprotein. While anlotinib exhibited affinity for α1-acid glycoprotein comparable to that of imatinib (Gleevec), influence of α1-acid glycoprotein on pharmacokinetics of anlotinib is probably limited. Unlike anlotinib, imatinib exhibited affinity for α1-acid glycoprotein substantially higher than its affinity for albumin, with an nK ratio of 92. Such an nK ratio for anlotinib was 1. The plasma protein α1-acid glycoprotein is mainly synthesized and metabolized in the liver and also expressed in malignant cells and its level may be elevated significantly in patients with malignant tumors7,19. Varying level of α1-acid glycoprotein could interfere with measurement of the plasma concentration of imatinib, rendering such concentration unreliable as surrogate marker of tumor intracellular concentration20,21. Although many approved tyrosine kinase inhibitors, such as axitinib (Inlyta), lapatinib (Tykerb), and vemurafenib (Zelboraf) (fu, <1%), are highly bound in human plasma, little evidence is available to support their interactions with other highly bound drugs17. This is probably because proteins other than albumin and α1-acid glycoprotein also significantly contribute to binding of these tyrosine kinase inhibitors in plasma. Like anlotinib, imatinib was found to have high affinity for lipoproteins, which contribute significantly to its binding in plasma (Table 3). Lipoproteins might also significantly contribute to binding of other tyrosine kinase inhibitors, also basic molecules, in plasma.
Multiple human P450 isoforms could mediate anlotinib's oxidative metabolism that governed its clearance from the systemic circulation, albeit CYP3A4 and CYP3A5 exhibiting the greatest in vitro metabolic capabilities. This suggests that significant alteration of the anlotinib metabolism in the liver via enzyme inhibition by coadministered drug(s) requires affecting the concerted action of multiple P450 enzymes, rather than affecting the function of a single enzyme. In other words, circulating anlotinib has a low propensity to be a victim of hepatic drug interactions by inhibiting the P450 enzymes. Given that the positioning of the intestine as the first site of exposure of xenobiotics to the body's metabolic system and that CYP3A represents the largest piece (82%) of the intestinal P450 pie22,23, inhibition of intestinal CYP3A during absorption probably results in increased systemic exposure to anlotinib. In addition, induction of the P450 enzymes, particularly CYP3A and CYP2C, may result in decreased systemic exposure to anlotinib. Meanwhile, anlotinib was found to be a potent in vitro inhibitor of CYP3A4 (IC50, 0.1 μmol/L) and CYP2C9 (0.9 μmol/L). Based on its multiple-dose human plasma pharmacokinetics3, drug interaction indices, as calculated by unbound plasma Cmax/IC50, were 0.16 for CYP3A4 and 0.02 for CYP2C9, suggesting that circulating anlotinib also had a low propensity to precipitate drug interactions on these P450 isoforms. CYP3A4 and CYP3A5 have similar substrate specificity and exhibit high (84%) amino acid sequence identity24,25. Despite being the substrate of CYP3A4 and CYP3A5 with comparable in vitro metabolic capabilities, anlotinib exhibited very much different inhibitory potency against these P450 isoforms (IC50, >100 μmol/L for CYP3A5). These data also suggested that inhibition of CYP3A4 by anlotinib had limited influence on pharmacokinetics of this tyrosine kinase inhibitor.
The majority of approved tyrosine kinase inhibitors are reported to cause hepatotoxicity that requires careful patient management to maintain treatment benefit without harm26,27. Some tyrosine kinase inhibitors, such as erlotinib (Tarceva) and sorafenib (Nexavar), have been observed to cause hyperbilirubinemia28,29. Since UGT1A1-mediated hepatic glucuronidation plays a key role in clearance of bilirubin from the systemic circulation, deficiency of this enzyme results in elevated serum level of total bilirubin30,31. Due to growing recognition of the importance of drug-bilirubin interactions, many tyrosine kinase inhibitors were assessed with respect to their inhibition of UGT1A1 activity32,33,34,35,36. Anlotinib inhibited UGT1A1-mediated β-estradiol glucuronidation, a surrogate for UGT1A1-mediated bilirubin glucuronidation, with an IC50 of 4.0 μmol/L; the UGT1A1 inhibition by anlotinib appeared less potent than those by erlotinib (IC50, 0.7 μmol/L, against N-3-carboxy propyl-4-hydroxy-1,8-naphthalimide glucuronidation)36 and sorafenib (0.1 μmol/L, against 4-methylumbelliferone glucuronidation)35. In addition, unbound Cmax values of anlotinib, erlotinib, and sorafenib at their respective clinically relevant doses were 0.02, 0.21, and 0.06 μmol/L, respectively3,17,26. Although the extent of UGT1A1 inhibition that is required to precipitate hyperbilirubinemia is unclear, anlotinib is believed to have a lower propensity to cause hyperbilirubinemia than erlotinib and sorafenib. In the phase I clinical trial to evaluate safety, pharmacokinetics, and efficacy of anlotinib, only mild total bilirubin elevation was reported in 33% (Grade 1) and 5% (Grade 2), of patients with advanced refractory solid tumors, while no incidence of severe hyperbilirubinemia (Grades 3–5) was reported3.
Development of multidrug resistance is a leading cause of cancer treatment failure; the molecular basis of such resistance involves transporter-mediated drug efflux, kinase domain mutations, DNA damage repair, activation of alternative signaling pathways, and evasion of cell death37. Increasing data suggest that MDR1 and BCRP are two transporters significantly contributing to resistance to tyrosine kinase inhibitors38. Combination drug therapy has been suggested to offer advantages for treatment of drug-resistant cancers. Although inhibitors of MDR1 and BCRP can be explored to overcome resistance to tyrosine kinase inhibitors that are substrates of these transporters in tumors, such drug combinations might enhance toxicity of these tyrosine kinase inhibitors by elevating their concentrations in normal tissues that express the transporters. Similarly, combinations of tyrosine kinase inhibitor that potently inhibit the transporter activity with cytotoxic anticancer drugs that are the transporter substrates might also yield desired pharmacokinetic drug interactions in tumor tissues but undesired ones in the normal tissues as well. Accordingly, the ideal tyrosine kinase inhibitor should not be a substrate or modulator of the ABC transporters38. Anlotinib was found not to be a substrate of MDR1 and BCRP, suggesting that it has a low propensity to develop intrinsic or acquired resistance arising from drug efflux from tumor cells. Meanwhile, anlotinib was not a potent inhibitor of these transporters as well, suggesting that coadministered drugs in anlotinib-including combinations are more likely to exert synergistic or additive pharmacodynamic effect as well as exhibit pharmacokinetic compatibility (ie, without any pharmacokinetic drug interactions) in the treatment of drug-resistant cancers.
Anlotinib exhibits multiple pharmacokinetic characteristics similar to those of many approved tyrosine kinase inhibitors, including good gastrointestinal absorption with pH-dependent water solubility and membrane permeability, high binding in plasma, and large apparent volume of distribution. Also, P450-mediated oxidation is a key factor governing anlotinib's oral bioavailability, clearance from the systemic circulation, terminal half-life, and associated interspecies differences. Compared with many approved tyrosine kinase inhibitors, anlotinib appears to have a low propensity to precipitate drug interactions via inhibition of many major drug metabolizing enzymes and transporters at its clinically relevant dose. Acid-suppressive drugs and intestinal CYP3A4 modulating drugs may interact with anlotinib. Anlotinib has a low propensity to cause hyperbilirubinemia and to develop resistance arising from transporter-mediated efflux from tumor cells. In human plasma, anlotinib is predominantly bound to albumin and lipoproteins; influences of varying levels of albumin and lipoproteins on pharmacokinetics of anlotinib and on its tumor intracellular concentration remain to be investigated in cancer patients.
Author contribution
Chuan LI, Feng CHEN and Wei NIU designed the research; Feng CHEN, Wei NIU, Chen-chun ZHONG, Jun-ling YANG, Wei-wei JIA, Li LI, Chen CHENG, Fei-fei DU, Su-ping ZHANG, Cheng-ying XIE, Na-ting ZHANG, Olajide E OLALEYE, Feng-qing WANG, Fang XU, Li-guang LOU, and Dong-ying CHEN performed the research; Chuan LI, Wei NIU, Chen-chun ZHONG, and Feng CHEN analyzed data; and Chuan LI and Wei NIU wrote the paper.
References
Krause DS, Van Etten RA . Tyrosine kinases as targets for cancer therapy. N Engl J Med 2005; 353: 172–87.
Arora A, Scholar EM . Role of tyrosine kinase inhibitors in cancer therapy. J Pharmacol Exp Ther 2005; 315: 971–9.
Sun YK, Niu W, Du F, Du CX, Li ST, Wang JW, et al. Safety, pharmacokinetics, and antitumor properties of anlotinib, an oral multi-target tyrosine kinase inhibitor, in patients with advanced refractory solid tumors. J Hematol Oncol 2016; 9: 105.
Han BH . Efficiency and safety of anlotinib hydrochloride as 3rd line treatment or beyond in patients with advanced NSCLC in ALTER-003 study, a randomized, double-blind, placebo-controlled Phase III trial in China. The American Society of Clinical Oncology Annual Meeting, Chicago, IL, USA, June 2–6, 2017, Abstract 182187.
Guo B, Li C, Wang GJ, Chen LS . Rapid and direct measurement of free concentrations of highly protein-bound fluoxetine and its metabolite norfluoxetine in plasma. Rapid Commun Mass Spectrom 2006; 20: 39–47.
Li J, Brahnmer J, Messersmith W, Hidalgo M, Baker SD . Binding of gefitinib, an inhibitor of epidermal growth factor receptor-tyrosine kinase, to plasma proteins and blood cells: in vitro and in cancer patients. Invest New Drugs 2006; 24: 291–7.
Zsila F, Fitos I, Bencze G, Kéri G, Őrfi L . Determination of human serum α1-acid glycoprotein and albumin binding of various marketed and preclinical kinase inhibitors. Curr Med Chem 2009; 16: 1964–77.
Dai JY, Yang JL, Li C . Transport and metabolism of flavonoids from Chinese herbal remedy Xiaochaihu-tang across human intestinal Caco-2 cell monolayers. Acta Pharmacol Sin 2008; 29: 1086–93.
Li L, Zhao YS, Du FF, Yang JL, Xu F, Niu W, et al. Intestinal absorption and presystemic elimination of various chemical constituents present in GBE50 extract, a standardized extract of Ginkgo biloba leaves. Curr Drug Metab 2012; 13: 494–509.
Kerns EH, Di L . Drug-like properties: concepts, structure design and methods: from ADME to toxicity optimization. 1st ed. Burlington: Academic Press; 2008. p 283 (equilibrium shake flask thermodynamic solubility method), p 267–8 (shake flask method for lipophilicity).
Hu ZY, Yang JL, Cheng C, Huang YH, Du FF, Wang FQ, et al. Combinatorial metabolism notably affects human systemic exposure to ginsenosides from orally administered extract of Panx notoginseng roots (Sanqi). Drug Metab Dispos 2013; 41: 1457–69.
Jiang RR, Dong JJ, Li XX, Du FF, Jia WW, Xu F, et al. Molecular mechanisms governing different pharmacokinetics of ginsenosides and potential for ginsenoside-perpetrated herb-drug interactions on OATP1B3. Br J Pharmacol 2015; 172: 1059–73.
Jia WW, Du FF, Liu XW, Jiang RR, Xu F, Yang JL, et al. Renal tubular secretion of tanshinol: molecular mechanisms, impact on its systemic exposure, and propensity for dose-related nephrotoxicity and for renal herb-drug interactions. Drug Metab Dispos 2015; 43: 669–78.
Smith BP, Vandenhende FR, DeSante KA, Farid NA, Welch PA, Callaghan JT, et al. Confidence interval criteria for assessment of dose proportionality. Pharm Res 2000; 17: 1278–83.
Davies B, Morris T . Physiological parameters in laboratory animals and humans. Pharm Res 1993; 10: 1093–5.
Lipinski CA . Drug-like properties and the causes of poor solubility and poor permeability. J Pharmacol Toxicol Methods 2000; 44: 235–49.
van Leeuwen RWF, van Gelder T, Mathijssen RHJ, Ajansman FG . Drug-drug interactions with tyrosine-kinase inhibitors: a clinical perspective. Lancet Oncol 2014; 15: e315–26.
van Erp NP, Gelderblom H, Guchelaar HJ . Clinical pharmacokinetics of tyrosine kinase inhibitors. Cancer Treat Rev 2009; 35: 692–706.
Lee SY, Lim JW, Kim YM . Effect of alpha-1-acid glycoprotein expressed in cancer cells on malignant characteristics. Mol Cell 2001; 11: 341–5.
Widmer N, Decosterd LA, Csajka C, Leyvraz S, Duchosal MA, Rosselet A, et al. Population pharmacokinetics of imatinib and the role of α1-acid glycoprotein. Br J Clin Pharmacol 2006; 62: 97–112.
Apperley JF . Part I: mechanisms of resistance to imatinib in chronic myeloid leukaemia. Lancet Oncol 2007; 8: 1018–29.
Kaminsky LS, Zhang QY . The small intestine as a xenobiotic-metabolizing organ. Drug Metab Dispos 2003; 31: 1520–5.
Paine MF, Hart HL, Ludington SS, Haining RL, Rettie AE, Zeldin DC . The human intestinal cytochrome P450 “PIE”. Drug Metab Dispos 2006; 34: 880–6.
Thummel KE, Wilkinson GR . In vitro and in vivo drug interactions involving human CYP3A. Annu Rev Pharmacol Toxicol 1998; 38: 389–430.
Aoyama T, Yamano S, Waxman DJ, Lapenson DP, Meyer UA . Fischer Vpperley, et al . Cytochrome P-450 hPCN3, a novel cytochrome P-450 IIIA gene product that is differentially expressed in adult human liver. cDNA and deduced amino acid sequence and distinct specificities of cDNA-expressed hPCN1 and hPCN3 for the metabolism of steroid hormones and cyclosporine. J Biol Chem 1989; 264: 10388–95.
Shah RR, Morganroth J, Shah DR . Hepatotoxcity of tyrosine kinase inhibitors: clinical and regulatory perspectives. Drug Saf 2013; 36: 491–503.
Spraggs CF, Xu CF, Hunt CM . Genetic characterization to improve interpretation and clinical management of hepatotoxcity caused by tyrosine kinase inhibitors. Pharmacogenomics 2013; 14: 541–54.
Jakacki RI, Hamilton M, Gilbertson RJ, Blaney SM, Tesak J, Krailo MD, et al. Prediatric phase I and pharmacokinetic study of erlotinib followed by the combination of erlotinib and temozolomide: a children's oncology group phase I consortium study. J Clin Oncol 2008; 26: 4921–7.
Abou-Alfa GK, Amadori D, Santoro A, Figer A, De Greve J, Lathia C, et al. Safety and efficacy of sorafenib in patients with hepatocellular carcinoma (HCC) and Child-Pugh A versus B cirrhosis. Gastrointest Cancer Res 2011; 4: 40–4.
Bosma PJ, Goldhoorn B, Bakker C, Oude Elferink RP, Chowdhury JR, Chowdhury NR, et al. Bilirubin UDP-glucuonosyltransferase 1 is the only relevant bilirubin glucuronidating isoform in man. J Biol Chem 1994; 269: 17960–4.
Tukey RH, Strassburg CP . Human UDP-glucuonosyltransferases: metabolism, expression, and disease. Annu Rev Pharmacol Toxicol 2000; 40: 581–616.
Liu Y, Ramirez J, House L, Ratain M . Comparison of the drug-drug interactions potential of erlotinib and gefitinib via inhibition of UDP-glucuronosyltransferases. Drug Metab Dispos 2010; 38: 32–9.
Ai L, Zhu LL, Yang L, GE GB, Cao YF, Liu Y, et al. Selectivity for inhibition of nilotinib on the catalytic activity of human UDP-glucuronosyltransferases. Xenobiotica 2014; 44: 320–5.
Zhang N, Liu Y, Jeong H . Drug-drug interaction potentials of tyrosine kinase inhibitors via inhibition of UDP-glucuronosyltransferases. Sci Rep 2015; 5: 17778.
Miners JO, Chau N, Rowland A, Burns K, McKinnon RA, Mackenzie PI, et al. Inhibition of human UDP-glucuronosyltransferase enzymes by lapatinib, pazopanib, regorafenib and sorafenib: implications for hyperbilirubinemia. Biochem Pharmacol 2017; 129: 85–95.
Cheng XW, Lv X, Qu HY, Li DD, Hu MM, Guo WZ, et al. Comparison of the inhibition potentials of icotinib and erlotinib against human UDP-glucuronosyltransferase 1A1. Acta Pharm Sin B 2017; 7: 657–64.
Holohan C, Schaeybroeck SV, Longley DB, Johnston PG . Cancer drug resistance: an evolving paradigm. Nat Rev Cancer 2013; 13: 714–26.
Shukla S, Chen ZS, Ambudkar SV . Tyrosine kinase inhibitors as modulators of ABC transporter-mediated drug resistance. Drug Resist Update 2012; 15: 70–80.
Author information
Authors and Affiliations
Corresponding authors
Supplementary information
Supplementary Information
Supplementary Figure and Table (DOC 84 kb)
Rights and permissions
About this article
Cite this article
Zhong, Cc., Chen, F., Yang, Jl. et al. Pharmacokinetics and disposition of anlotinib, an oral tyrosine kinase inhibitor, in experimental animal species. Acta Pharmacol Sin 39, 1048–1063 (2018). https://doi.org/10.1038/aps.2017.199
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2017.199
Keywords
This article is cited by
-
Cross-species comparison in nonclinical pharmacokinetics of lenvatinib by a simple HPLC with ultraviolet detection
Scientific Reports (2023)
-
Reactive oxygen species mediate anlotinib-induced apoptosis via activation of endoplasmic reticulum stress in pancreatic cancer
Cell Death & Disease (2020)
-
A phase I study investigation of metabolism, and disposition of [14C]-anlotinib after an oral administration in patients with advanced refractory solid tumors
Cancer Chemotherapy and Pharmacology (2020)
-
Anlotinib: a novel multi-targeting tyrosine kinase inhibitor in clinical development
Journal of Hematology & Oncology (2018)