Abstract
Aim:
To investigate the potential antagonistic activity of the antidiabetic agent glybenclamide for the human platelet thromboxane A2 receptor (abbreviated as TPR).
Methods:
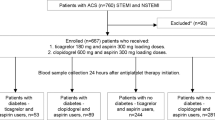
Platelets were obtained from healthy donors. Aggregation studies were performed in a model 700 aggregometry system. Radioactivity was counted in a Beckman LS 6000 liquid scintillation counter and calcium imaging was performed using an LS50B PerkinElmer Fluorescence Spectrometer.
Results:
It was found that glybenclamide: 1) inhibited aggregation induced by the TPR agonist U46619 (IC50=2.3±0.31 μmol/L) and by the thromboxane A2 precursor arachidonic acid (IC50=2.6±0.24 μmol/L); 2) displaced SQ29,548 from its binding sites on platelets; 3) lacked any detectable effects on aggregation stimulated by ADP, or the thrombin receptor activating-peptide 4; 4) blocked calcium mobilization induced by U46619, but not by ADP; and 5) failed to raise cAMP levels.
Conclusion:
The findings indicate that glybenclamide exerts inhibitory effects on platelets by interacting with TPR. Thus, glybenclamide or a rationally designed derivative has the potential to serve as an antithrombotic agent.
Similar content being viewed by others
Introduction
Platelet activation is a complex process with independent, yet overlapping pathways for activation1, 2, 3, 4, 5, 6. One such pathway is triggered by an arachidonic acid derivative, known as thromboxane A2 (TXA2), which acts by interacting7, 8, 9 with a seven-transmembrane receptor (abbreviated as TPR). The TXA2 pathway has been shown10, 11, 12 to play an essential role in hemostasis, and in the development of thrombotic disorders; making it a target for therapeutic interventions. Based on these considerations, therapeutic strategies have focused on either modulating the synthesis of TXA213, 14, or interfering with its receptor binding. While, the former has been successfully targeted by the platelet COX-1 inhibitor aspirin, this therapeutic agent is associated with undesirable adverse effects (such as gastric ulcers)15, 16, and resistance17. Regarding TPR antagonists; while many were developed18, 19, 20, 21, none of them is currently available for clinical use. Thus, there is still considerable interest in developing TPR antagonists.
To this end, estimates indicate that it may require 15 years to bring a new drug into the market, with a cost of hundreds of millions of dollars22. Furthermore, despite all efforts, only 20-30 drugs receive approval by the Food and Drug Administration (FDA) in the USA in any given year23. One solution to these limitations is to discover new uses for currently prescribed drugs; the “repurposing old drugs for new uses” approach24, 25, 26. Based on these considerations, we elected to undertake a similar approach in our pursuit of a TPR antagonist. Thus, we searched for drugs that share structural similarity with a TPR antagonist, namely SQ29,54820. We noticed significant similarity between the antidiabetic sulfonylurea glybenclamide27, and SQ29,548, particularly with regard to the latter's pharmacophores28. Consequently, we hypothesized that glybenclamide exhibits TPR antagonistic activity. In this connection, given that sulfonylureas were pursued as antiplatelet agents, and although none of these studies was comprehensive, others have also investigated the antiplatelet effects of antidiabetics of the sulfonylurea class; including glybenclamide. For example, it was found that glybenclamide did not inhibit platelet aggregation induced by thrombin, but suppressed (calcium) Ca2+ release from internal Ca2+ stores induced by the same agent29. These data are contradictory since Ca2+ mobilization is known to play an essential role in thrombin-dependent platelet activation30. Other studies have shown that glybenclamide inhibited both the cyclooxygenase and 12-lipoxygenase pathways in platelets29, but in a later study the authors contradicted their own findings with regard to the inhibition of the lipoxygenase pathway31. Another study on the vasculature, showed that glybenclamide acts by interacting with TPRs32, thereby contradicting the finding that glybenclamide inhibits the cyclooxygenase pathway. In summary, there are clear inconsistencies concerning the biological effects of glybenclamide on platelet function. While the reasons for these apparent discrepancies are not known, they may derive from variations in the experimental conditions/platelet preparations, inconsistency in the dose used in the various experimental approaches, or inherent differences in the potency of the ligands employed. Finally, in line with the principles of drug rediscovery, it is noteworthy that aspirin itself was initially used as an analgesic33, 34, before its antiplatelet activity was discovered13, 14.
Based on these considerations, we investigated two aspects of glybenclmaide's biology: (1) its functional effects on three different pathways of activation in human platelets; and (2) the potential mechanism by which it produces these effects (eg, TPR-dependent mechanism of action).
Materials and methods
Reagents
U46619, arachidonic acid, SQ29,548 and PGI2 were from Cayman Chemical (Ann Arbor, MI). ADP, stir bars and other disposables were from (Chrono-Log; Havertown, PA). 3H]SQ29,548 was purchased from PerkinElmer Life Sciences (Shelton, CT). Glybenclamide, Protease activated receptor 4 (PAR4) activating peptide (TRAP4; AYPGKF-NH2), phosphodiesterase inhibitor Ro20-1724, protein kinase A, protein kinase A inhibitor, Cellosolve, isoflurane and indomethacin were from Sigma Aldrich (St Louis, MO). 3H]cAMP was from Amersham Biosciences (Piscataway, NJ), and cold cAMP from Assay Designs (Ann Arbor, MI). The Adenylate cyclase inhibitor SQ22536 was from Enzo Life Sciences International, Inc (formerly BIOMOL international; Plymouth Meeting, PA). Sodium citrate (3.8% w/v) solution, 60 mL syringes, 50 mL conical tubes were obtained from Fisher Scientific (Hanover Park, IL). The Fura2/AM dye and Pluronic F-127 were from Molecular Probes (Eugene, OR). Human platelets were from healthy volunteers who denied taking any medication in the last 10 days prior to collection. Note: volunteers gave their informed consent before they were allowed to donate blood.
Human platelet functional studies
Blood was withdrawn by venipuncture of the cephalic vein into a 60 mL syringe (Kendall) from human volunteers. Coagulation was inhibited by addition of 3.8% w/v sodium citrate solution in a ratio of 9 parts blood to 1 part citrate. Blood was then spun at 160×g for 10 min in a 50 mL centrifuge tube. Resultant supernatant was carefully pipetted out and then recentrifuged at least once to sediment out nucleated cells, forming platelet rich plasma (PRP). Platelet poor plasma (PPP) was prepared by spinning blood at 2000×g for 15 min. PRP was diluted with PPP to adjust platelet count to 2×108−3×108 platelets/mL. All aggregation experiments were performed after incubation with 10 μmol/L indomethacin for 2 min to prevent thromboxane A2 generation, except when arachidonic acid was used as the aggregating agonist. The control traces were obtained by the addition of vehicle, U46619, arachidonic acid, ADP, or TRAP4 to PRP after establishing baseline light transmission for at least 1 min. The effect of these agents was measured using the turbidimetric method35 with a model 700 whole blood lumi-aggregometer (Chronolog Corporation; Havertown, PA). The aggregation traces were captured using the Aggrolink8 software (Chronolog Corporation; Havertown, PA).
Human platelet function inhibition studies
For the inhibition of platelet function studies, PRP was incubated with 1–10 μmol/L glybenclamide, 150 nmol/L or 1 μmol/L SQ29,548 or vehicle controls for 5 min prior to stimulation with 1 μmol/L U46619, 0.5 mmol/L arachidonic acid, 15 μmol/L ADP, or 40 μmol/L TRAP4. Furthermore, the reversal of inhibition was performed after first incubating with the adenylate cyclase inhibitor (300 μmol/L) SQ22536 for 45 min, then adding 1 nmol/L PGI2, or 10 μmol/L glybenclamide before stimulation with 1 μmol/L U46619 or 0.5 mmol/L arachidonic acid.
Displacement binding in intact platelets.
Resuspended platelets were prepared as previously descri-bed36, 37. The platelet suspension (1×109 platelets/mL) was incubated with 1 nmol/L 3H]SQ29,548 at RT for 10 min, and then increasing concentrations of the displacing ligand glybenclamide (0.035−30 μmol/L) were added for an additional 45 min. Next, the 3H]SQ29,548 bound platelets were captured by running through 0.45 micron Millipore filters over a vacuum suction unit. The filters were then washed once and counted for radioactivity in a Beckman LS 6000 liquid scintillation counter. To calculate the non-specific binding, the same concentration of radioligand was competed against 1000-fold excess of unlabeled SQ29,548.
Assay of platelet adenosine 3', 5'-cyclic monophosphate (cAMP)
Human PRP (500 μL) samples were collected in an eppendorf tube and treated with vehicle, (1 nmol/L) PGI2, or (10 μmol/L) glybenclamide. Next, the phosphodiesterase inhibitor RO20-1724 (100 μmol/L) was added, and platelets were spun down and immediately frozen in liquid nitrogen. The platelet pellet was then resuspended, sonicated, boiled for 4 min, spun down, and the supernatant was transferred to a new tube. The concentration of cAMP in the supernatant was measured as previously described38. The standard curve samples were prepared by adding known concentrations of unlabeled cAMP to the supernatant obtained from vehicle treated platelets.
Platelet calcium mobilization
Platelets were isolated from blood, washed, and then suspended in Tyrode's buffer without calcium. Platelets were then loaded with Fura-2/AM (5 μmol/L) in the presence of Pluronic F-127 (0.2 μg/mL; Molecular Probes) for 30 min at 37 °C. Next, platelets were washed once and resuspended in Tyrode's buffer containing 0 or 1 mmol/L Ca2+. Platelets were then activated with U46619 (1 μmol/L), arachidonic acid (0.5 mmol/L), ADP (15 μmol/L) or TRAP4 (40 μmol/L), in the presence or absence of glybenclamide (10 μmol/L). Calcium measurements were done by alternating excitation between 340 and 380 nm, and measuring fluorescence/emission at 509 nm using an LS 50B Fluorescence Spectrometer (PerkinElmer).
Data analysis
All experiments were performed at least three times, with blood obtained from at least three different donors. Data were analyzed using GraphPad PRISM statistical software (San Diego, CA). The displacement binding curve was generated using non-linear regression analysis, with a one site competition model, whereas the standard cAMP curve was generated by applying linear regression. Results were compared using unpaired 2-tailed Student's t test, with P<0.05 considered to be statistically significant. IC50 values are represented as mean±SEM.
Results
Glybenclamide inhibits TPR-/U46619-induced platelet aggregation
Given the structural similarity between glybenclamide and SQ29,548 (Figure 1), and in order to investigate whether the oral sulfonylurea glybenclamide (an antidiabetic agent) has the capacity to inhibit platelet TPR signaling, platelet aggregometry experiments were performed. Our initial studies demonstrated that addition of TXA2 mimetic U46619 (1 μmol/L) to human PRP produced a typical shape change and aggregation response (Figure 2A). Furthermore, it was also found that 1 μmol/L of glybenclamide produced a significant inhibition of the U46619-induced platelet activation (Figure 2A; 1 μmol/L trace). This inhibitory effect of glybenclamide was found to be concentration-dependent (Figure 2A; 1–10 μmol/L traces and inset), with an IC50 = 2.3±0.31 μmol/L. This finding demonstrates that glybenclamide has the capacity to block platelet aggregation, and that the underlying mechanism perhaps involves TPRs. To test this notion, the next set of experiments investigated the effects of glybenclamide on a separate agonist, namely the TXA2 precursor arachidonic acid, which also triggers platelet aggregation by activating TPRs.
Effect of glybenclamide on human platelet aggregation stimulated by the TPR agonist U46619, and the TXA2 precursor arachidonic acid. (A) Indomethacin-treated PRP was stimulated with 1 μmol/L U46619 in the absence or presence of increasing concentrations of glybenclamide (1–10 μmol/L) to generate a concentration-dependent inhibition curve (inset shows quantification of the glybenclamide concentration-dependent inhibition curve of U46619-induced aggregation response). (B) PRP was stimulated with 0.5 mmol/L arachidonic acid in the absence or presence of increasing concentrations of glybenclamide (1-10 μmol/L) to generate a concentration-dependent inhibition curve (inset shows quantification of the glybenclamide concentration-dependent inhibition curve of arachidonic acid-induced aggregation response). Each aggregation curve is representative of multiple traces obtained from three separate platelet preparations, from three different blood donors (bP<0.05, n=3).
Glybenclamide inhibits TPR-/arachidonic acid-induced platelet aggregation
Similar to U46619, it was found that glybenclamide exerted concentration-dependent (1–10 μmol/L) inhibition on platelet activation stimulated by 0.5 mmol/L arachidonic acid (Figure 2B), with an IC50=2.6±0.24 μmol/L. These data further suggest that the underlying mechanism by which glybenclamide inhibits platelets is through TPR blockade. To confirm the interaction with platelet TPRs, displacement binding studies between glybenclamide and a well-characterized radiolabeled TPR antagonist (ie, 3[H]SQ29,548) were performed.
Glybenclamide displaces [3H]SQ29,548 from its TPR binding sites
If glybenclamide exerts its inhibitory effects via TPR antagonism, then it would be expected to displace TPR ligands from their binding sites. Using radioligand displacement studies, it was found that glybenclamide, indeed, had the capacity to completely displace 3H]SQ29,548 from its binding sites on platelets (Figure 3), demonstrating an interaction with TPRs. While this finding clearly indicates that the mechanism by which glybenclamide inhibits platelets involves TPR antagonism, it does not rule out the potential for generalized inhibitory effects on platelet, through a cAMP-dependent mechanism. To test this possibility, we examined the effects of glybenclamide on platelet aggregation mediated by TPR-independent mechanisms (ie, ADP and the thrombin receptor activating peptide 4 [TRAP4]).
Displacement binding curve of 3H]SQ29,548 by glybenclamide in intact platelets. Binding displacement of 1 nmol/L 3H]SQ29,548 with increasing concentrations of glybenclamide (0.035–30 μmol/L). Results are the average of at least three different experiments, from blood obtained from three separate donors.
Glybenclamide is devoid of inhibitory effects on ADP-induced platelet aggregation
If cAMP indeed contributes to the inhibitory effects of glybenclamide on platelet function, one would expect glybenclamide blockade of platelet aggregation in response to all agonists, eg, ADP and TRAP4. Our results demonstrated that pretreating platelets with glybenclamide (1 μmol/L) did not produce any detectable effects on platelet aggregation in response to 15 μmol/L ADP (data not shown). Moreover, even at a concentration as high as 10 μmol/L, which completely blocked aggregation by U46619 or arachidonic acid (Figure 2A and 2B, respectively), glybenclamide appeared to be devoid of any inhibitory effects on platelet aggregation by ADP (Figure 4A). This finding suggests that the mechanism by which glybenclamide inhibits platelet aggregation is cAMP independent. This was further confirmed by determining whether glybenclamide inhibits aggregation induced by TRAP4.
Effect of glybenclamide on human platelet aggregation stimulated by ADP, and the thrombin receptor activating peptide 4 (TRAP4). (A) Indomethacin-treated PRP was stimulated with 15 μmol/L ADP in the absence or presence of 10 μmol/L glybenclamide. (B) Indomethacin-treated PRP was stimulated with 40 μmol/L TRAP4 in the absence or presence of 10 μmol/L glybenclamide. Each aggregation curve is representative of multiple traces obtained from three separate platelet preparations, from three different blood donors.
Glybenclamide is devoid of inhibitory effects on TRAP4-induced platelet aggregation
As was the case with the platelet agonist ADP, our results revealed that glybenclamide, even at high concentrations (10 μmol/L) did not exhibit any detectable effects on platelet aggregation triggered by 40 μmol/L TRAP4 (Figure 4B). These data indicate that glybenclamide does not produce broad-spectrum inhibition of platelet aggregation, which is consistent with cAMP-independent mechanisms. To directly examine this notion, we next investigated whether glybenclamide raises platelet cAMP levels.
Glybenclamide does not raise platelet cAMP levels
The finding that glybenclamide exerts inhibitory effects on platelet activation that are specific to TPRs argues against a cAMP-dependent mechanism. This conclusion was confirmed by measuring cAMP levels in response to glybenclamide treatment. Our data indicates that even at 10 μmol/L, glybenclamide did not elevate platelet cAMP levels, as opposed to 1 nmol/L of the control PGI2 (Figure 5A). Furthermore, while the adenylyl cyclase inhibitor SQ22536 (300 μmol/L) did not produce any detectable effects on glybenclamide blockade of U46619- or arachidonic acid-stimulated aggregation (Figure 5B and 5C, respectively), it completely reversed the inhibitory effects of PGI2 on aggregation induced by U46619 (Figure 5D). These data demonstrate that the underlying mechanism of inhibition of platelet activation by glybenclamide does not involve cAMP. We next examined the effect of glybenclamide on calcium mobilization in response to TPR activation.
Effects of glybenclamide and PGI2 on basal platelet cAMP levels; and effects of glybenclamide on human platelet aggregation induced by U46619 or arachidonic acid (compared to the effects of PGI2 on human platelet aggregation induced by U46619) in the presence or absence of the AC inhibitor SQ22536. A) PRP was treated with 10 μmol/L glybenclamide or 1 nmol/L of the control PGI2 before cAMP levels were measured (bP<0.05, n=3). B) PRP was first incubated with or without the AC inhibitor SQ22536 (300 μmol/L) and then stimulated with 1 μmol/L U46619 in the presence or absence of 10 μmol/L glybenclamide. C) PRP was first incubated with or without the AC inhibitor SQ22536 (300 μmol/L) and then stimulated with 0.5 mmol/L arachidonic acid in the presence or absence of 10 μmol/L glybenclamide. D) PRP was first incubated with or without the AC inhibitor SQ22536 (300 μmol/L) and then stimulated with 1 μmol/L U46619 in the presence or absence of 1 nmol/L PGI2. Each aggregation curve is representative of multiple traces obtained from three separate platelet preparations, from three different blood donors.
Glybenclamide inhibits calcium mobilization induced by TPR/ U46619 but not by ADP
Since calcium plays a central role in platelet aggregation downstream of TPR and other G-protein coupled receptors, it is expected that glybenclamide would also inhibit calcium mobilization. Indeed, it was found that glybenclamide (10 μmol/L) abolished calcium mobilization in response to 1 μmol/L U46619 and 0.5 mmol/L arachidonic acid (Figure 6A and not shown, respectively). On the other hand, 10 μmol/L glybenclamide did not produce any effects on calcium mobilization in response to 15 μmol/L ADP or 40 μmol/L TRAP4 (Figure 6B, and not shown, respectively). These data are consistent with glybenclamide's inhibitory effects that are selective for TPR-dependent platelet function. Finally, we sought to compare the inhibitory profile of glybenclamide with that for the classical TPR antagonist SQ29,548.
Effect of glybenclamide on human platelet calcium mobilization stimulated by the TPR agonist U46619, and ADP. (A) Indomethacin-treated PRP was stimulated with 1 μmol/L U46619 in the absence or presence of 10 μmol/L glybenclamide. (B) Indomethacin-treated PRP was stimulated with 15 μmol/L ADP in the absence or presence of 10 μmol/L glybenclamide. Each calcium trace is representative of multiple traces obtained from three separate platelet preparations, from three different blood donors.
Glybenclamide exhibits a platelet-function inhibitory profile that is comparable to that of the classical TPR antagonist SQ29,548
Similar to glybenclamide's effects, it was found that the selective TPR antagonist SQ29,548 (at 150 nmol/L or 1 μmol/L) blocked platelet aggregation stimulated by 1 μmol/L U46619 or 0.5 mmol/L arachidonic acid (Figure 7A, 7B, 7C, and not shown). On the other hand, SQ29,548 (at 150 nmol/L or even 1 μmol/L) was found to be devoid of any inhibitory effects on platelet aggregation triggered by 15 μmol/L ADP, or 40 μmol/L TRAP4 (Figure 7D, Figure 7E, Figure 7F, and not shown). Thus, the inhibitory profile exhibited by glybenclamide on platelet function appears to be identical to that of the classical TPR antagonist SQ29,548, which is in agreement with a TPR-dependent mechanism of action.
Effect of SQ29,548 on human platelet aggregation stimulated by the TPR agonist U46619, the TXA2 precursor arachidonic acid, ADP, and the thrombin receptor activating peptide 4 (TRAP4). A) Indomethacin-treated PRP was stimulated with 1 μmol/L U46619 in the absence or presence of 150 nmol/L SQ29,548. B) Indomethacin-treated PRP was stimulated with 1 μmol/L U46619 in the absence or presence of 1 μmol/L SQ29,548. C) PRP was stimulated with 0.5 mmol/L arachidonic acid in the absence or presence of 150 nmol/L SQ29,548. D) Indomethacin-treated PRP was stimulated with 15 μmol/L ADP in the absence or presence of 150 nmol/L SQ29,548. E) Indomethacin-treated PRP was stimulated with 15 μmol/L ADP in the absence or presence of 1 μmol/L SQ29,548. F) Indomethacin-treated PRP was stimulated with 40 μmol/L TRAP4 in the absence or presence of 150 nmol/L SQ29,548. Each aggregation curve is representative of multiple traces obtained from three separate platelet preparations, from three different blood donors.
In summary, the present studies demonstrate that glybenclamide has the capacity to exert TPR-specific inhibitory effects on human platelet function, as demonstrated by selective blockade of aggregation (and calcium mobilization) by the classical agonists U46619 and arachidonic acid, and displacement of binding of a classical TPR ligand. Our results also provide evidence that cAMP is not involved in the mechanism of inhibition, since glybenclamide lacked any inhibition on aggregation mediated by the agonists ADP and TRAP4, nor did it increase platelet cAMP levels.
Discussion
Given the clear involvement of TXA2/TPR signaling in the pathogenesis of multiple disease processes (eg, thrombosis and asthma) 10, 11, 12, 39, the limitations of aspirin therapy15, 16, and evidence that antagonists are superior to aspirin in certain disease states40, there is an increasing interest in the development of TPR antagonists. Of note, due to a host of reasons, the use of antagonists developed (which were not rationally designed) thus far, has been experimental18, 19, 20, 21, 41. Nonetheless, it is anticipated that recent literature regarding the ligand-binding domain of TPR will aid the discovery of TPR antagonists42, 43.
Historically, conventional drug discovery takes one of two routes44, either the target-centered or compound-centered approach, and each route may take around 15 years. Consequently, there is growing interest in an approach that focuses on investigating new indications for drugs that have already been approved by the FDA (ie, “drug rediscovery”) 24, 25, 26. Aside from their well-characterized pharmacology, such drugs would have a safety profile that has been well defined through many years of clinical experience. To this end, we decided to undertake a similar approach (ie, repurpose a currently approved drug) in our pursuit of agents that possess antagonistic activity against platelet TPRs. Specifically, we searched for drugs that share structural similarity with TPR antagonists. We selected the experimental TPR antagonist with the highest affinity (ie, SQ29,548), and we were particularly interested in compounds that share similarity with the pharmacophores of SQ29,54828. We found that the antidiabetic agent glybenclamide meets this structural requirement as follows (see Figure 1): 1) the functional groups which are anionic at physiological pH (7.4); these are the carboxylic acid group of SQ29,548 and the sulfonylurea of glybenclamide (indicated by the red fonts in the structures); 2) the amide groups (indicated by the pink fonts in the structures); and 3) the aromatic rings (indicated in blue fonts in the structures). On the other hand, glybenclamide appears to lack a chemical group equivalent to the fourth SQ29,548 pharmacophore, ie, the 14-position nitrogen indicated by the grey font in SQ29,548 structure (see Figure 1). Nonetheless, we believe that there is sufficient similarity in their chemistry to confer glybenclamide with the capacity to interact with TPRs. In order to test this notion and to address previous inconsistencies regarding its biological activity, we evaluated the effects of glybenclamide on platelet aggregation mediated via TPR activation. Interestingly, it was found that pre-treating platelets with glybenclamide resulted in significant inhibition in their aggregation response to the agonist U46619, in a concentration dependent manner. Glybenclamide also inhibited the calcium mobilization response triggered by U46619. These findings demonstrate that this antidiabetic drug does indeed have the capacity to block platelet function, presumably via interacting with TPRs. To further test this notion, we examined the effects of glybenclamide on aggregation triggered by the TXA2 precursor arachidonic acid. Our results showed that glybenclamide exerted a concentration-dependent inhibitory effect on aggregation triggered by arachidonic acid. Given the chemical similarity between glybenclamide and the antagonist SQ29,548, this finding appears to be consistent with a TPR-dependent mechanism of action. This notion was further supported by the finding that glybenclamide completely displaced the radiolabeled antagonist SQ29,548 from its platelet TPR binding sites. In addition, these data suggest that glybenclamide does in fact contain a “minimum” number of pharmacophores that are required for interacting with TPR, and possess a three dimensional orientation that allows for this interaction. Nevertheless, without performing molecular modeling studies, it will be difficult to accurately predict which of the proposed chemical groups of glybenclamide serve as pharmacophores, and thereby participate in its interaction process with the ligand binding pocket of TPR. Notably, the concentration needed to produce complete inhibition of platelets by glybenclamide is higher than those for SQ29,548, which suggests that the former has lower affinity for the receptor. It is tempting to speculate that the apparent low affinity of glybenclamide for platelet TPRs is due to: 1 lack of one or more of the established pharmacophores of SQ29,548 (eg, the 14-position nitrogen), which means lower number of TPR amino acid recognition/interaction sites; and/or 2 possessing a three dimensional conformation that is somewhat different from SQ29,548; especially, since glybenclamide is a flexible compound whereas SQ29,548 has a rigid chemistry, and this would impact the manner by which it docks onto the binding pocket; and/or 3 differences in the bonding energies of the two molecules. Therefore, to guide the repurposing of drugs, one should make similar structural comparisons, especially for experimental drugs with well-defined pharmacophores45. Based on these considerations, we believe this may represent a general paradigm that may be extended to other targets/drugs.
In summary, our data thus far provide evidence that glybenclamide exhibits inhibitory effects on platelet function, and indicate that the underlying mechanism is mediated, at least in part, via TPR blockade. However, our data does not exclude the possibility that cAMP, a common inhibitor of platelet function, may contribute to the antiplatelet effects of glybenclamide. If this were the case, then glybenclamide would be expected to also produce inhibitory effects on platelet activation triggered by mechanisms independent of TPRs (eg, ADP or TRAP4). However, our experiments revealed that even when used at a concentration that completely blocked TPR-mediated aggregation, glybenclamide produced no apparent effects on aggregation or calcium mobilization induced by ADP, or TRAP4, nor did it cause cAMP increases. Also, the adenylyl cyclase inhibitor SQ22536 did not reverse the inhibitory effects that glybenclamide exerted on platelet activation by TPRs, whereas it completely reversed those by the control PGI2. These findings further demonstrate that the inhibitory effects exerted by glybenclamide are limited to TPR antagonism. Consistent with our conclusions, control experiments revealed that glybenclamide exhibited a platelet-function inhibitory profile that is similar to that for the TPR antagonist SQ29,548, i.e., selective blockade of platelet aggregation mediated by activation of TPRs, but not by ADP or TRAP4 receptors.
Collectively, our results obtained using human platelets provide evidence that glybenclamide exerts antiplatelets effects that are TPR dependent. Consequently, glybenclamide has the potential to serve as a therapeutic agent, and can be added to the arsenal of interventions available for treating thrombotic disease. Furthermore, based on recent evidence46 of a novel inhibitory function for isoprostanes in platelets, which was shown to prevail under conditions of TPR antagonism, concurrent therapy of a TPR antagonist (eg, glybenclamide) and aspirin might be superior to either therapy alone. Thus, glybenclamide may prove beneficial in combination therapy approaches.
Even if this newly identified biological activity is not adequate for therapy or if the hypoglycemia that may be induced by glybenclamide is an issue, novel glybenclamide derivatives, with antithromboxane receptor activity, may be rationally-designed; as was previously done were a TPR antagonist was derived from the loop diuretic torasemide; which is also a sulfonylurea47. Nevertheless, our findings suggest that the use of glybenclamide should be encouraged in the treatment of diabetic patients with enhanced platelet functions; especially since hypoglycemia would not be a limiting factor. Finally, consistent with our findings, a study on patients diagnosed with type II Diabetes Millets, and treated with glybenclamide for 4 months, revealed that they were protected against thrombosis formation48. Thus, while hypoglycemia could be a limiting factor, glybenclamide appears to produce its protective effects against thrombosis development, at concentrations that are effective for managing Diabetes Millets48. This is an important consideration given the established link between diabetes and thrombotic disorders.
Non standard abbreviations
PRP, platelet rich plasma; PPP, platelet poor plasma; TXA2, thromboxane A2; TPR, thromboxane A2 receptor; TRAP4, thrombin receptor-activating peptide 4; PAR, protease activated receptor.
Author contribution
Fadi T KHASAWNEH: Experimental design, data interpretation/analysis and prepared the manuscript; Wallace J MURRAY: data interpretation/analysis and participated in manuscript preparation; Harold J TING: Performed experiments and manuscript preparation.
References
Baglia FA, Shrimpton CN, Emsley J, Kitagawa K, Ruggeri ZM, Lopez JA, et al. Factor XI interacts with the leucine-rich repeats of glycoprotein Ibalpha on the activated platelet. J Biol Chem 2004; 279: 49323–9.
Born GV . Aggregation of blood platelets by adenosine diphosphate and its reversal. Nature 1962; 194: 927–9.
Brisson C, Azorsa DO, Jennings LK, Moog S, Cazenave JP, Lanza F . Co-localization of CD9 and GPIIb-IIIa (alpha IIb beta 3 integrin) on activated platelet pseudopods and alpha-granule membranes. Histochem J 1997; 29: 153–65.
Du X . Signaling and regulation of the platelet glycoprotein Ib-IX-V complex. Curr Opin Hematol 2007; 14: 262–9.
Landis RC . Protease activated receptors: clinical relevance to hemostasis and inflammation. Hematol Oncol Clin North Am 2007; 21: 103–13.
Reilly M, Fitzgerald GA . Cellular activation by thromboxane A2 and other eicosanoids. Eur Heart J 1993; 14 Suppl K: 88–93.
Halushka PV, Mais DE, Mayeux PR, Morinelli TA . Thromboxane, prostaglandin and leukotriene receptors. Annu Rev Pharmacol Toxicol 1989; 29: 213–39.
Hirata M, Hayashi Y, Ushikubi F, Yokota Y, Kageyama R, Nakanishi S, et al. Cloning and expression of cDNA for a human thromboxane A2 receptor. Nature 1991; 349: 617–20.
Kim SO, Lim CT, Lam SC, Hall SE, Komiotis D, Venton DL, et al. Purification of the human blood platelet thromboxane A2/prostaglandin H2 receptor protein. Biochem Pharmacol 1992; 43: 313–22.
Oates JA, FitzGerald GA, Branch RA, Jackson EK, Knapp HR, Roberts LJ 2nd . Clinical implications of prostaglandin and thromboxane A2 formation (2). N Engl J Med 1988; 319: 761–7.
Patrono C, Ciabattoni G, Davi G . Thromboxane biosynthesis in cardiovascular diseases. Stroke 1990; 21 (12 Suppl): IV130–3.
Ogletree ML . Overview of physiological and pathophysiological effects of thromboxane A2. Fed Proc 1987; 46: 133–8.
Clarke RJ, Mayo G, Price P, FitzGerald GA . Suppression of thromboxane A2 but not of systemic prostacyclin by controlled-release aspirin. N Engl J Med 1991; 325: 1137–41.
Patrono C . Aspirin as an antiplatelet drug. N Engl J Med 1994; 330: 1287–94.
Meijer K, Schulman S . Determinants of bleeding risk in patients on antithrombotic and antifibrinolytic drugs. Semin Thromb Hemost 2008; 34: 762–71.
Schlansky B, Hwang JH . Prevention of nonsteroidal anti-inflammatory drug-induced gastropathy. J Gastroenterol 2009; 44 Suppl 19: 44–52.
Pusch G, Feher G, Kotai K, Tibold A, Gasztonyi B, Feher A, et al. Aspirin resistance: focus on clinical endpoints. J Cardiovasc Pharmacol 2008; 52: 475–84.
Le Breton GC, Venton DL, Enke SE, Halushka PV . 13-Azaprostanoic acid: a specific antagonist of the human blood platelet thromboxane/endoperoxide receptor. Proc Natl Acad Sci U S A 1979; 76: 4097–101.
Nicolaou KC, Magolda RL, Smith JB, Aharony D, Smith EF, Lefer AM . Synthesis and biological properties of pinane-thromboxane A2, a selective inhibitor of coronary artery constriction, platelet aggregation, and thromboxane formation. Proc Natl Acad Sci USA 1979; 76: 2566–70.
Ogletree ML, Harris DN, Greenberg R, Haslanger MF, Nakane M . Pharmacological actions of SQ 29,548, a novel selective thromboxane antagonist. J Pharmacol Exp Ther 1985; 234: 435–41.
Patscheke H, Stegmeier K, Muller-Beckmann B, Sponer G, Staiger C, Neugebauer G . Inhibitory effects of the selective thromboxane receptor antagonist BM 13.177 on platelet aggregation, vasoconstriction and sudden death. Biomed Biochim Acta 1984; 43: S312–8.
DiMasi JA, Hansen RW, Grabowski HG . The price of innovation: new estimates of drug development costs. J Health Econ 2003; 22: 151–85.
Cohen FJ . Macro trends in pharmaceutical innovation. Nat Rev Drug Discov 2005; 4: 78–84.
Aronson JK . Old drugs--new uses. Br J Clin Pharmacol 2007; 64: 563–5.
Chong CR, Sullivan DJ Jr . New uses for old drugs. Nature 2007; 448: 645–6.
McPhie DC . Old drugs, new uses: solving a Hatch-Waxman patent predicament. Food Drug Law J 2004; 59: 155–68.
Dessi P . [Basic pharmacological research on the hypoglycemic action of N-4-[beta-(2-methoxy-5-chlorbenzamide)-ethyl]-benzosulfonyl-N′-cyclohexylu rea (Glybenclamide)]. Acta Diabetol Lat 1969; 6: 206–21.
Jin B, Hopfinger AJ . A proposed common spatial pharmacophore and the corresponding active conformations of some TXA2 receptor antagonists. J Chem Inf Comput Sci 1994; 34: 1014–21.
Ozaki Y, Yatomi Y, Kume S . Effects of oral hypoglycaemic agents on platelet functions. Biochem Pharmacol 1992; 44: 687–91.
Dubois C, Panicot-Dubois L, Gainor JF, Furie BC, Furie B . Thrombin-initiated platelet activation in vivo is vWF independent during thrombus formation in a laser injury model. J Clin Invest 2007; 117: 953–60.
Satoh K, Ozaki Y, Yatomi Y, Kume S . Effects of sulfonylurea agents on platelet arachidonic acid metabolism; study on platelet homogenates. Biochem Pharmacol 1994; 48: 1053–5.
Pfister SL, Pratt PE, Kurian J, Campbell WB . Glibenclamide inhibits thromboxane-mediated vasoconstriction by thromboxane receptor blockade. Vascul Pharmacol 2004; 40: 285–92.
Eagle E, Carlson AJ . Toxicity, antipyretic and analgesic studies on 39 compounds including aspirin, phenacetin and 27 derivatives of carbazole and tetrahydrocarbazole. J Pharmacol Exp Ther 1950; 99: 450–7.
Steiner TJ, Voelker M . Gastrointestinal tolerability of aspirin and the choice of over-the-counter analgesia for short-lasting acute pain. J Clin Pharm Ther 2009; 34: 177–86.
Michal F, Born GV . Effect of the rapid shape change of platelets on the transmission and scattering of light through plasma. Nat New Biol 1971; 231: 220–2.
Hung SC, Ghali NI, Venton DL, Le Breton GC . Specific binding of the thromboxane A2 antagonist 13-azaprostanoic acid to human platelet membranes. Biochim Biophys Acta 1983; 728: 171–8.
Kattelman EJ, Venton DL, Le Breton GC . Characterization of U46619 binding in unactivated, intact human platelets and determination of binding site affinities of four TXA2/PGH2 receptor antagonists (13-APA, BM 13.177, ONO 3708 and SQ 29,548). Thromb Res 1986; 41: 471–81.
Gilman AG . A protein binding assay for adenosine 3':5'-cyclic monophosphate. Proc Natl Acad Sci U S A 1970; 67: 305–12.
Dahlen SE, Kumlin M, Granstrom E, Hedqvist P . Leukotrienes and other eicosanoids as mediators of airway obstruction. Respiration 1986; 50 Suppl 2: 22–9.
Cayatte AJ, Du Y, Oliver-Krasinski J, Lavielle G, Verbeuren TJ, Cohen RA . The thromboxane receptor antagonist S18886 but not aspirin inhibits atherogenesis in apo E-deficient mice: evidence that eicosanoids other than thromboxane contribute to atherosclerosis. Arterioscler Thromb Vasc Biol 2000; 20: 1724–8.
Ghali NI, Kattelman EJ, Hung SC, Schnorf KE, Le Breton GC, Venton DL . Synthesis of [17,18-3H] trans-13-azaprostanoic acid. A labeled probe for the PGH2/TXA2 receptor. Prostaglandins 1984; 27: 865–76.
Khasawneh FT, Huang JS, Turek JW, Le Breton GC . Differential mapping of the amino acids mediating agonist and antagonist coordination with the human thromboxane A2 receptor protein. J Biol Chem 2006; 281: 26951–65.
Turek JW, Halmos T, Sullivan NL, Antonakis K, Le Breton GC . Mapping of a ligand-binding site for the human thromboxane A2 receptor protein. J Biol Chem 2002; 277: 16791–7.
Drews J . Drug discovery: a historical perspective. Science 2000; 287: 1960–4.
Guner OF . History and evolution of the pharmacophore concept in computer-aided drug design. Curr Top Med Chem 2002; 2: 1321–32.
Khasawneh FT, Huang JS, Mir F, Srinivasan S, Tiruppathi C, Le Breton GC . Characterization of isoprostane signaling: evidence for a unique coordination profile of 8-iso-PGF(2alpha) with the thromboxane A(2) receptor, and activation of a separate cAMP-dependent inhibitory pathway in human platelets. Biochem Pharmacol 2008; 75: 2301–15.
Rolin S, Dogne JM, Michaux C, Delarge J, Masereel B . Activity of a novel dual thromboxane A(2)receptor antagonist and thromboxane synthase inhibitor (BM-573) on platelet function and isolated smooth muscles. Prostaglandins Leukot Essent Fatty Acids 2001; 65: 67–72.
Shi MZ, Feng JG, Zheng JJ . A comparison between glibenclamide and glipizide in the treatment of type II diabetes. Zhonghua Nei Ke Za Zhi 1991; 30: 94–7, 126.
Acknowledgements
This work was supported by Intramural Funding Support from the College of Pharmacy at Western University of Health Sciences (to FTK). The authors would like to thank Dr Daniel PEARCE for assistance with blood draws. The authors have no conflicting financial interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ting, H., Murray, W. & Khasawneh, F. Repurposing an old drug for a new use: glybenclamide exerts antiplatelet activity by interacting with the thromboxane A2 receptor. Acta Pharmacol Sin 31, 150–159 (2010). https://doi.org/10.1038/aps.2009.195
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2009.195
Keywords
This article is cited by
-
Thyroxine therapy ameliorates serum levels of eicosanoids in Chinese subclinical hypothyroidism patients
Acta Pharmacologica Sinica (2016)
-
Drug–Drug Coamorphous Systems: Characterization and Physicochemical Properties of Coamorphous Atorvastatin with Carvedilol and Glibenclamide
Journal of Pharmaceutical Innovation (2013)