Abstract
Purpose
To investigate the associated factors of foveoschisis and foveal detachment without macular hole in highly myopic eyes.
Methods
A cross-sectional study of 124 eyes of 68 highly myopic patients was performed. The patients underwent complete ocular examination, fundus photography, and optical coherence tomography (OCT).
Results
Of the 124 eyes, 10 (8%, 10/124) had foveoschisis or foveal detachment without a macular hole on OCT examination. On the basis of univariate analysis, six variables were associated with the pathologic changes, including age over 40 years (P=0.018), spherical equivalent over 10 D (P=0.042), axial length over 31 mm (P=0.001), macular chorioretinal atrophy (P=0.00003), posterior staphyloma (P=0.0003), and vitreoretinal interface factors, including epiretinal membrane, posterior vitreoschisis, and vitreomacular traction (P=0.00002). In the multivariate analysis, three factors were independently associated with foveoschisis and foveal detachment without macular hole in high myopia: axial length, macular chorioretinal atrophy, and vitreoretinal interface factors.
Conclusions
Foveoschisis and foveal detachment without macular hole are sight-threatening disorders in highly myopic eyes. Axial length, macular chorioretinal atrophy, and vitreoretinal interface factors were independently associated with these pathological conditions. Thus, both intraocular and outer ocular wall factors play important roles and merit further study.
Similar content being viewed by others
Introduction
Myopia is a highly prevalent condition, especially in Southeast Asia, with reported rates as high as 80%.1, 2 A previous study in Taiwan found that the prevalence of high myopia (less than −6.0 D) at the age of 18 years was 24% in girls and 18% in boys.3 It often results in sight-threatening ocular pathology. Macular hole with posterior retinal detachment (RD) is a well-known complication of posterior staphyloma in highly myopic eyes.4 There were some highly myopic patients who presented with poor vision without a macular hole or RD, which made it difficult to explain the reason for poor visual acuity based on biomicroscopy. Recent studies using OCT demonstrated asymptomatic macular holes, foveal retinal detachment without a macular hole, and myopic traction maculopathy in highly myopic eyes.5, 6, 7
The management of foveoschisis and foveal detachment without a macular hole in highly myopic eyes remains unclear and inspires much debate. In order to provide the most appropriate management methods, it is important to know the factors associated with these sight-threatening diseases. Early diagnosis and prompt management might be beneficial.
The purpose of this study was to use OCT to identify and evaluate the prevalence of factors associated with foveoschisis and foveal detachment without a macular hole in highly myopic eyes.
Methods
Subjects for this study were prospectively recruited from patients who visited the ophthalmology clinic of Chang Gung Memorial Hospital-Kaohsiung Medical Center, between January 2005 and December 2005. Subjects with the diagnosis of high myopia and meeting eligibility requirements were selected for participation. This study was approved by the hospital's institutional review board and was performed in accordance with the World Medical Association's Declaration of Helsinki. Informed consent was obtained for each subject before enrolment. Patients enrolled in this study underwent a complete ophthalmologic examination, which included best-corrected visual acuity testing with Landolt's C chart, intraocular pressure measurement, slit-lamp examination, dilated slit-lamp examination with stereo biomicroscopy, and indirect ophthalmoscopy. A-scan testing was obtained for the measurement of axial length. OCT-3 was performed on one or both eyes of each subject after pupil dilation. Colour photography and B-scan ultrasonography were obtained for the diagnosis of macular chorioretinal atrophy (diffuse or patchy) and posterior staphyloma.
Highly myopic eyes were defined as having a spherical equivalence (SE) of less than –6 D or an axial length (AXL) greater than 26.5 mm. Exclusion criteria included systemic diseases, previous ocular surgery within 6 months, and glaucoma due to thin retinal thinkness.
The OCT-3 system used in this study (model 3000, software version B 3.0, Carl Zeiss Meditec, Dublin, CA, USA) permits cross-sectional imaging by acquiring a sequence of 128 interferometric axial reflectance profiles (A-scans) of the retina. The OCT-3 fast-scan protocol completed total data acquisition in 1.92 s. To obtain a map of retinal thickness at the macula, six equally spaced intersecting radial scans through the center of the fovea were performed. Each radial scan had a diameter of 6.0 mm and comprised a circular area centred on the fovea. Ophthalmic photographers who were skilled in the use of the OCT-3 system performed all OCT scans through a dilated pupil.
Foveoschisis was defined as separation of the neurosensory retina into two or more layers in the foveal area. Foveal detachment without a hole was defined as retinal detachment confined to the macular area, but without macular hole. Both were combined with or without epiretinal membranes or vitreomacular traction. Vitreoretinal interface factors were defined as including epiretinal membrane (ERM), posterior vitreoschisis (PVS), and vitreomacular traction.
Data were analysed using χ2 test and Fisher's exact test (if the expected value was under 5) for the univariate analysis of factors associated with foveoschisis and foveal detachment without a hole. Probability values of P<0.05 were considered statistically significant. In addition, logistic regression was used to estimate odds ratios (OR) and 95% confidence intervals (CI) for further independent variables. Variables that were significant at the P⩽0.1 level in the univariate analysis were included in backward logistic regression analysis to select the final list of independent variables. All analyses were computed using SPSS software (v10.0, SPSS Inc. Chicago, IL, USA).
Results
One hundred and twenty-four highly myopic eyes from 68 patients were included in this study. Twenty-six patients were male and 42 were female. The mean age was 39 years (range, 15–78 years). The mean SE was −11.45 D (range, −6 to −27 D). The mean AXL was 29.07 mm (range, 25.99–34.07). The BCVA ranged from counting finger to 20/20. Forty-three eyes (35%) had posterior staphyloma and 81 eyes (65%) did not. Thirty-four eyes (27%) had diffuse or patchy chorioretinal atrophy in the macula. Sixteen eyes (13%) had vitreoretinal interface factors, including eight eyes with ERM and the other eight eyes with PVS in the macula.
Out of the 124 eyes, 10 had foveoschisis or foveal detachment without a macular hole on OCT examination. The prevalence was 8% (10/124). The characteristics of these patients are summarized in Table 1. The age of the patients with foveal detachment and foveoschisis ranged from 37 to 73 years (mean, 53 years). Eight of the 10 eyes (80%) were from patients over the age of 40 years. The SE in these eyes ranged from −7.6 to −22.25 D (mean, −14.69 D). Nine of the 10 eyes (90%) had posterior staphyloma. AXL in these eyes ranged from 26.66 to 32.79 mm (mean, 30.06 mm). BCVA in these eyes ranged from 20/1000 to 20/33 (mean, 20/133). Colour fundus photography showed that 9 of 10 eyes had chorioretinal atrophy in the macula, six had diffuse atrophy, and three had patchy atrophy. On OCT, seven of 10 eyes (70%) had foveoschisis. Seven eyes (70%) had vitreoretinal interface factors, including six eyes with ERM and only one eye with PVS and traction.
In the univariate analysis, Table 2 shows the factors associated with foveoschisis and foveal detachment without macular hole in highly myopic eyes. A trend towards higher risk was seen for age over 40 years, SE over 10 D, AXL over 31 mm, macular chorioretinal atrophy, posterior staphyloma, and vitreoretinal interface factors (P=0.018, 0.042, 0.001, 0.00003, 0.0003, and 0.00002, respectively). There was no significant association with sex or laterality of the eye (P=0.739 and 1.745, respectively).
These six associated variables were included in the multivariate analysis. AXL over 31 mm, macular chorioretinal atrophy, and vitreoretinal interface factors were independently associated with higher risk of foveoschisis and foveal detachment without a macular hole in highly myopic eyes (Table 3). AXL over 31 mm was associated with an increased risk of foveoschisis and foveal detachment without a macular hole in highly myopic eyes (adjusted OR 17.7; 95% CI 1.5–216.9, P=0.024). The presence of macular chorioretinal atrophy was associated with increased risk for both conditions (adjusted OR, 13.3; 95% CI, 1.3–138.3, P=0.030). The presence of vitreoretinal interface factors was associated with increased risk (adjusted OR, 37.2; 95% CI, 3.6–380.9, P=0.002).
Discussion
In this study, the prevalence of foveoschisis or foveal detachment without a macular hole was 8% (10/124 eyes) in highly myopic eyes. The reported prevalence rate ranges from 9 to 34% in previous studies in Japan and Italy.5, 7, 8 The reason for the slightly lower prevalence rate in this study could be due to the random inclusion of high-myopia subjects visiting our outpatient clinic for problems other than retinal problems. Our data should be more similar to the general high-myopia group in a hospital-based study.
Our study revealed that macular chorioretinal atrophy, axial length, and vitreoretinal interface factors were the three independent factors associated with foveoschisis and foveal detachment without macular hole in highly myopic eyes. It means that both intraocular and outer ocular wall factors play important roles in developing foveoschisis and foveal detachment in highly myopic eyes.
Baba et al7 also found posterior staphyloma and severe myopic degenerative changes to be the associated factors in their patients. Longer AXL and chorioretinal atrophy had close relationships with posterior staphyloma in high myopia.9, 10, 11 Posterior staphyloma is recognized as an important factor in foveoschisis and foveal detachment without a macular hole.7, 8 Longer AXL, chorioretinal atrophy, and posterior staphyloma represent the outer ocular pouching forces resulting in pathologic changes. Longer AXL increases the eyeball diameter and induces retinal stretching. The stretched retina might be insufficient in contrast to the enlarged sclera and induce the vector force inside. In addition, chorioretinal atrophy within the staphyloma might weaken the adherence between the sensory retina and retinal pigment epithelium (RPE).12 Within the foveal detachment, subretinal fluid is poorly pumped out due to RPE atrophy within the area of chorioretinal atrophy.
In the univariate analysis, factors of older age, higher myopia (>10 D), and posterior staphyloma also showed significant trends of association with foveoschisis and foveal detachment without macular hole. However, these factors were not significant in the final multivariate analysis. The reason might be that the latter two factors were also associated with and interacted with AXL and chorioretinal atrophy of the macula.10 The fact that staphyloma disappears in the multivariate analysis probably means that both staphyloma and chorioretinal atrophy are expressions of the same process and that chorioretinal atrophy is just a more sensitive marker to indicate that the process has reached clinically significant levels. Chorioretinal atrophy and posterior staphyloma were seldom found in children.13 This suggests that ageing and long-term mechanical stretching of the eyeball might be predisposing factors for posterior staphyloma. In our study, only two eyes (2/10) were less than 40-year-old. Preventing progressive thinning of the scleral wall with age is important to prevent the occurrence of foveoschisis and foveal detachment in highly myopic eyes in later life.
Only 3 of 10 eyes with foveoschisis or foveal detachment without a macular hole had vision better than 20/200. The natural course of these diseases would be to develop a macular hole with or without retinal detachment.14 Therefore, management of foveoschisis and foveal detachment without macular hole is necessary. The vitreoretinal interface factors represented inner ocular force and were still the most important independent factors in the final multivariate analysis. The intraocular forces inducing foveoschisis and foveal detachment without macular hole include the epiretinal membrane, vitreomacular traction, residual focal vitreoretinal adhesion, and retinal vessel stiffness.5, 7, 15, 16 There are several reports on the management of releasing intraocular forces, including vitrectomy, residual vitreous cortex removal, with or without internal membrane peeling, and gas tamponade.16, 17 Most of these cases had a favorable outcome after relieving vitreoretinal interface force. However, persistent foveoschisis and macular hole development were still reported in some eyes.18, 19 This indicates that the release of these intraocular forces relieves only a part of the causes of foveoschisis and foveal detachment without a macular hole. Outer ocular forces such as chorioretinal atrophy, posterior staphyloma, and longer AXL should also be considered in the management of these diseases. Posterior scleral buckling might be an alternative or additional choice for treatment.20, 21
One of the limitations of this study was the small number of patients with foveoschisis or foveal detachment without macular hole. In addition, a hospital-based study might not be representative of the general population in the community. Further, a large-scale community-based study is necessary.
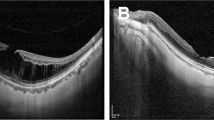
In conclusion, foveoschisis and foveal detachment without macular hole were common in our highly myopic patients. Longer AXL, macular chorioretinal atrophy, and vitreoretinal interface factors were significantly associated with these conditions (Figure 1, Figure 2, Figure 3).
Left eye of a 37-year-old woman with high myopia (−22.25 D) with posterior staphyloma. The fundus picture showed diffuse chorioretinal atrophy in macula. Best-corrected visual acuity was 0.02. The axial length was 32.79 mm. Optic coherence tomography revealed foveoschisis and foveal detachment without macular hole. In addition, the epiretinal membrane was revealed on the surface of the retina.
Right eye of a 54-year-old male with high myopia (−11 D) with posterior staphyloma. The fundus picture showed patchy chorioretinal atrophy in macula. Best-corrected visual acuity was 0.05. The axial length was 29.12 mm. Optic coherence tomography revealed posterior vitreous schisis, foveoschisis, and foveal detachment without macular hole.
References
Lin LL, Shih YF, Tsai CB, Chen CJ, Lee LA, Hung PT et al. Epidemiologic study of ocular refraction among schoolchildren in Taiwan in 1995. Optom Vis Sci 1999; 76: 275–281.
Goh WS, Lam CS . Changes in refractive trends and optical components of Hong Kong Chinese aged 19–39 years. Ophthalmic Physiol Opt 1994; 14: 378–382.
Lin LL, Shih YF, Hsiao CK, Chen CJ, Lee LA, Hung PT . Epidemiologic study of the prevalence and severity of myopia among schoolchildren in Taiwan in 2000. J Formos Med Assoc 2001; 100: 684–691.
Morita H, Ideta H, Ito K, Yonemoto J, Sasaki K, Tanaka S . Causative factors of retinal detachment in macular holes. Retina 1991; 11: 281–284.
Panozzo G, Mercanti A . Optical coherence tomography findings in myopic traction maculopathy. Arch Ophthalmol 2004; 122: 1455–1460.
Coppe AM, Ripandelli G, Parisi V, Varano M, Stirpe M . Prevalence of asymptomatic macular holes in highly myopic eyes. Ophthalmology 2005; 112: 2103–2109.
Baba T, Ohno-Matsui K, Futagami S, Yoshida T, Yasuzumi K, Kojima A et al. Prevalence and characteristics of foveal retinal detachment without macular hole in high myopia. Am J Ophthalmol 2003; 135: 338–342.
Takano M, Kishi S . Foveal retinoschisis and retinal detachment in severely myopic eyes with posterior staphyloma. Am J Ophthalmol 1999; 128: 472–476.
Edge R, Navon S . Axial length and posterior staphyloma in Saudi Arabian cataract patients. J Cataract Refract Surg 1999; 25: 91–95.
Gozum N, Cakir M, Gucukoglu A, Sezen F . Relationship between retinal lesions and axial length, age and sex in high myopia. Eur J Ophthalmol 1997; 7: 277–282.
Steidl SM, Pruett RC . Macular complications associated with posterior staphyloma. Am J Ophthalmol 1997; 123: 181–187.
Grossniklaus HE, Green WR . Pathologic findings in pathologic myopia. Retina 1992; 12: 127–133.
Kobayashi K, Ohno-Matsui K, Kojima A, Shimada N, Yasuzumi K, Yoshida T et al. Fundus characteristics of high myopia in children. Jpn J Ophthalmol 2005; 49: 306–311.
Shimada N, Ohno-Matsui K, Baba T, Futagami S, Tokoro T, Mochizuki M . Natural course of macular retinoschisis in highly myopic eyes without macular hole or retinal detachment. Am J Ophthalmol 2006; 142: 497–500.
Ikuno Y, Gomi F, Tano Y . Potent retinal arteriolar traction as a possible cause of myopic foveoschisis. Am J Ophthalmol 2005; 139: 462–467.
Kobayashi H, Kishi S . Vitreous surgery for highly myopic eyes with foveal detachment and retinoschisis. Ophthalmology 2003; 110: 1702–1707.
Kwok AK, Lai TY, Yip WW . Vitrectomy and gas tamponade without internal limiting membrane peeling for myopic foveoschisis. Br J Ophthalmol 2005; 89: 1180–1183.
Hirakata A, Hida T . Vitrectomy for myopic posterior retinoschisis or foveal detachment. Jpn J Ophthalmol 2006; 50: 53–61.
Sayanagi K, Ikuno Y, Tano Y . Reoperation for persistent myopic foveoschisis after primary vitrectomy. Am J Ophthalmol 2006; 141: 414–417.
Theodossiadis GP, Theodossiadis PG . The macular buckling procedure in the treatment of retinal detachment in highly myopic eyes with macular hole and posterior staphyloma: mean follow-up of 15 years. Retina 2005; 25: 285–289.
Baba T, Tanaka S, Maesawa A, Teramatsu T, Noda Y, Yamamoto S . Scleral buckling with macular plombe for eyes with myopic macular retinoschisis and retinal detachment without macular hole. Am J Ophthalmol 2006; 142: 483–487.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was presented at the 2007 Association for Research in Vision and Ophthalmology (ARVO) Annual Meeting.
The authors have no financial interests in the study.
Rights and permissions
About this article
Cite this article
Wu, PC., Chen, YJ., Chen, YH. et al. Factors associated with foveoschisis and foveal detachment without macular hole in high myopia. Eye 23, 356–361 (2009). https://doi.org/10.1038/sj.eye.6703038
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6703038
Keywords
This article is cited by
-
Postoperative large intraretinal cavity and schisis with paravascular inner break in high myopia
Japanese Journal of Ophthalmology (2023)
-
Observation of macular hole associated with retinoschisis in patients with high myopia
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
Posterior scleral reinforcement for the treatment of myopic traction maculopathy
BMC Ophthalmology (2022)
-
Vitrectomy with internal limiting membrane peeling and gas tamponade for myopic foveoschisis
BMC Ophthalmology (2022)
-
Natural course of myopic traction maculopathy and factors influencing progression and visual acuity
BMC Ophthalmology (2021)