Abstract
Aim
To compare the safety and effectiveness of trypan blue capsule staining under air vsunder viscoelastic.
Methods
A total of 52 consecutive patients planned for phacoemulsification of white mature cataract were randomly assigned to trypan blue staining under air or under viscoelastic. Perioperative changes in best-corrected visual acuity (BCVA), central corneal thickness (CCT), and endothelial cell density (ECD) were compared between the two groups. The differences in operating and phacoemulsification times, staining pattern, and complications between the two groups were also recorded.
Results
Phacoemulsification of white mature cataract was performed in 50 (96%) eyes. The median preoperative BCVA was hand movement. No significant differences in the baseline characteristics were found between the two groups. At 3 months after phacoemulsification, the median BCVA improved to 0.8. The mean CCT returned to preoperative level by 1 month postoperatively and the mean ECD loss was 11.9% 3 months postoperatively. No significant differences in median BCVA, mean phacoemulsification and operation times, mean CCT, and mean ECD were found between the two groups.
Conclusions
Trypan blue staining of the anterior lens capsule under air or under viscoelastic were similarly effective and safe methods for the phacoemulsification of white mature cataract.
Similar content being viewed by others
Introduction
In the last decade, phacoemulsification has become the standard management of cataract in developed countries. However, phacoemulsification of white cataract poses particular challenge to the cataract surgeon as the continuous curvilinear capsulorhexis (CCC) is more difficult to complete due to loss of red reflex, increase in intralenticular pressure, and occasional leakage of lens matter from the anterior capsule puncture site. An intact complete CCC is critical to minimize the risk of capsular tear and to ensure stable in-the-bag intraocular lens (IOL) implantation.1 Various dyes include fluorescein,2, 3, 4 indocyanine green,2, 5, 6, 7, 8 and trypan blue,2, 9, 10, 11, 12, 13, 14, 15, 16 have been used for capsular staining to facilitate CCC. Different staining techniques, including subcapsular injection, staining under an air bubble, and staining under viscoelastic material, have been attempted.
Melles et al9 initiated the use of trypan blue to stain the anterior capsule under air. This allowed the formation of a ‘dye lake’ and prevented the dye dilution by aqueous. Capsular staining under air, however, was criticized as time-consuming and it may be difficult to reform the anterior chamber with a single air bubble.11 An alternative staining technique without the use of an air bubble was suggested by Yetik et al11 and involves injection of dispersive viscoelastic. The underside of the injection cannula was used to spread the dye mechanically to obtain homogenous stain. A shorter operating time and less corneal oedema in the early postoperative period were reported with this technique. Unfortunately, the study did not have a control group for comparison.11 This technique of staining under viscoelastic was also assessed by Ernus et al12 and the postoperative outcomes were similar to the fellow eye with senile cataract undergoing phacoemulsification without staining.
In order to evaluate the safety and effectiveness of trypan blue staining under air vs under viscoelastic, we conducted a randomized controlled trial to compare the two techniques. This study also aimed to provide supplementary information in the use of trypan blue in phacoemulsification of white cataract by reporting the perioperative changes in visual acuity, central corneal thickness (CCT), and endothelial cell count.
Patients and methods
Study design
This is a prospective randomized controlled trial carried out in Hong Kong Eye Hospital from February to August 2004. Patients were randomized to undergo trypan blue staining under an air bubble (air group) or under a dispersive viscoelastic (sodium chondrotin sulphate 4%–sodium hyaluronate 3%, Viscoat, Alcon, Fort Worth) (viscoelastic group) at the commencement of surgery. Allocation concealment was ensured by using a centralized computer-generated randomization table. Inclusion criteria included patients aged 18 years or older with mature white cataract listed for phacoemulsification. Mature white cataract was defined as totally opacified lens matter with the absence of red reflex. Patients with a history of trypan blue sensitivity, corneal dystrophy, glaucoma, or suspected retinal detachment on ultrasonography were excluded. Informed consent was obtained in all patients and the study was approval by an institutional ethics committee.
All eligible patients received preoperative examination including best-corrected visual acuity (BCVA), slit-lamp examination, applanation tonometry, B-scan ultrasonography, specular microscopy (NonCon Robo SP-8000, Konan Inc., Japan), and ultrasound pachymetry (EchoScan US-1800, Nidek Inc., Japan).
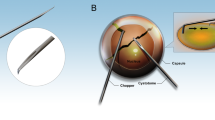
Surgical technique
All cataract operations were performed by a single surgeon (TL) under retrobulbar anesthesia. For patients allocated to the air group, an air bubble was injected into the anterior chamber using a 27-gauge cannula through a paracentesis. Trypan blue 0.06% solution (0.1–0.2 ml) (VisionBlue, DORC, Netherlands) was then injected on the anterior capsule with a 27-gauge cannula (Figure 1a). After 5 s, trypan blue solution was aspirated from the anterior chamber with bimanual irrigation and aspiration. For patients assigned to the viscoelastic group, the anterior chamber was filled with dispersive viscoelastic (sodium chondrotin sulphate 4%–sodium hyaluronate 3%, Viscoat, Alcon, Fort Worth) through the paracentesis and 0.1–0.2 ml of trypan blue solution was painted onto the anterior capsule with a 27-gauge cannula through two paracentesis (Figure 1b). The anterior chamber was then irrigated with BSS and excessive trypan blue–viscoelastic mixture was aspirated.
After capsular staining, the anterior chamber was refilled with viscoelastic and a superior clear corneal wound was constructed. The homogeneity of capsule staining was documented with intraoperative photography. CCC was performed with forceps and hydrodissection was carried out in all cases to ensure free rotation of the nucleus. Phacoemulsification was performed using stop-and-chop technique (Legacy Series 20000, Alcon). Nucleus density was graded intraoperatively by the surgeon on initial sculpting as 1+: soft; 2+: medium; 3+: hard; and 4+: very hard. The maximum phacoemulsification power setting ranged from 40 to 65%. A foldable hydrophobic acrylic IOL (AcrySof® MA30 or MA60, Alcon) was implanted and the ultrasound and total operating times were noted.
Follow-up examinations
Postoperatively, patients received a tapering course of topical prednisolone acetate 1% (Pred Forte, Allergan) and levofloxacin 0.5% (Cravit, Santen, Tokyo) for 6 weeks. Patients were assessed on day 1, 1 week, 1 month, and 3 months after the operation. Postoperative examination included BCVA, slit-lamp examination, applanation tonometry, fundal examination, and ultrasound pachymetry. Specular microscopy was performed at the 1- and 3-month visits. The CCT at each visit was calculated from the mean of five ultrasound pachymetry measurements and the endothelial cell density (ECD) was measured by taking an average of two measurements. Examinations were carried out by masked observers not aware of the patients' assigned group.
Outcome measures and statistical analysis
The primary outcome measures included the changes in mean CCT and ECD. The BCVA, operating and phacoemulsification times, staining pattern, and complications between the two groups were compared. The mean CCT was used to determine the sample size. For detecting a 5% difference in CCT between the two groups, with α=0.05 and power=80%, the calculated sample size was 25 eyes in each group. Statistical analyses were carried out with SPSS 11.5. Categorical variables were compared using the χ2 test and continuous variables for the two groups were compared using the two-tailed t-test or Mann–Whitney U-test. A P-value ≤0.05 was considered statistically significant.
Results
Preoperative demographics
A total of 52 eyes of 52 patients with white mature cataract were recruited during the study period. In total, 26 eyes (50%) were assigned to the air group and 26 (50%) eyes to the viscoelastic group. A total of 32 patients (64.0%) were male and 18 (36.0%) were female. The mean age of the patients was 65.7 years (range 46–80 years). There was no significant difference in age and sex between the air group and the viscoelastic group (Table 1).
The preoperative BCVA was equal or worse than 1/60 in all of patients and the median preoperative BCVA was hand movement. Visual acuity was light perception in seven eyes (13.5%), hand movement in 36 eyes (69.2%), finger counting in five eyes (9.6%) and 1/60 in four eyes (7.6%). There was no significant difference between the two groups in terms of median preoperative visual acuity (Mann–Whitney U-test, P=1.00), nucleus hardness (Mann–Whitney U-test, P=0.23) and mean preoperative IOP (two-tailed t-test, P=0.60).
Intraoperative data
Phacoemulsification was performed in 50 (96%) of the 52 eyes with one eye in each group requiring conversion to extracapsular cataract extraction due to radial tear during CCC. These cases were excluded from subsequent analyses. No significant difference in the uniformity of staining between the two groups was found (Fisher exact test, P=0.42) (Table 2). The mean operating and phacoemulsification times were 25 min (range, 10–35 min) and 1.9 min (range, 0.6–4.0 min), respectively. There were no significant differences in the mean operating and phacoemulsification times between the two groups (Mann–Whitney U-test, P=0.90 and 0.21, respectively). There were significant differences between the phacoemulsification time and hardness of the nucleus (Kruskal–Wallis H-test, P=0.003) but no significant difference existed between the total operating time and the nucleus hardness (Kruskal–Wallis H-test, P=0.24).
Postoperative visual outcomes
The median postoperative BCVA on the first day after the operation was 0.5 and improved to 0.7 at 1 week postoperatively. At the month 3 follow-up, the median final BCVA was 0.8 (range, 0.3–1.0), with 47 (94%) eyes having a final BCVA of 0.6 or better. No significant differences in the median postoperative BCVA between the air and viscoelastic groups were observed at all follow-up intervals (Table 3).
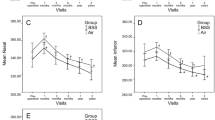
Change in mean CCT
The mean preoperative CCT was 547 μm (range, 469–620 μm) with no significant difference between the two groups (two-tailed t-test, P=0.14). On day 1 after the operation, the mean CCT for the air group and the viscoelastic group were 651 μm (+17.5%) and 629 μm (+16.5%), respectively. By the end of the first week, the mean increase in CCT reduced to 38 μm (+6.9%) and 44 μm (+8.1%), respectively. There were no significant differences in the mean CCT and change in mean CCT during the follow-up period (Table 4).
Change in ECD
The mean preoperative ECD for the 50 eyes was 2482 cells/mm2 (range, 1824–3558 cells/mm2). At 1 and 3 months postoperatively, the mean ECD reduced to 2210 (−11.0%) cells/mm2 and 2186 (−11.9%) cells/mm2, respectively. The reductions in mean ECD after surgery were statistically significant (two-tailed t-test, P=0.001). For the air group, the mean ECD reduced to 2196 (−10.5%) and 2128 (−13.3%) cells/mm2 at month 1 and month 3, respectively. Similarly, there was also a reduction in ECD in the viscoelastic group with mean ECD of 2223 (−11.4%) cells/mm2 and 2244 (−10.6%) cells/mm2 at month 1 and month 3, respectively. The differences in the mean ECD, mean change in ECD during the perioperative period, mean proportion of hexagonal cells, and mean coefficient of variation between the two groups were not statistically significant (Table 5).
Complications
As described previously, two eyes required conversion to extracapsular cataract extraction due to radial tear associated with increased intralenticular pressure. One (2%) eye in the air group developed rupture of the posterior capsule during cortex removal. Anterior vitrectomy with sulcus IOL placement was performed without further complication and the patient had a final BCVA of 0.8.
Discussion
Phacoemulsification of white mature cataracts with trypan blue capsule staining has increased the safety and success of the surgery. It has been confirmed histologically that trypan blue selectively stains the basement membrane of the anterior lens capsule.17 Originally, Melles et al9 stained the anterior capsule under an air bubble. Yetik et al11 advocated trypan blue capsule staining under a dispersive viscoelastic, claiming that staining with an air bubble resulted in longer surgery and more oedematous cornea in the early postoperative period. The results of our randomized controlled trial showed that both techniques were equally safe, fast, and effective. The mean operative time did not differ between the two groups. Postoperative serial measurements at day 1, 1 week, 1 month, and 3 months including BCVA and changes in CCT and ECD were also not statistically different between the two groups.
In our series, two (4%) patients developed peripheral extension of the CCC and required conversion to extracapsular cataract extraction. Chakrabarti and Singh18 retrospectively reported the outcomes of phacoemulsification in eyes with white cataract without the use of dye. As a result of the poor visibility, a complete capsulorhexis could not be achieved in 28.3% of patients. Vasavada et al19 performed phacoemulsification of white mature cataracts using a two-stage capsulorhexis technique. A small capsulorhexis was initially made, followed by phacoemulsification. The CCC was then enlarged before IOL implantation. Complete capsulorhexis was achieved in 96%, which was similar to that of our study. With the use of trypan blue, CCC was successful in 96.2–100% as reported in various studies.9, 10, 12, 14
In our study, the mean increase in CCT on day 1 was 17.0%. By the end of the first week, the mean increase in CCT has reduced to 7.5% and almost returned to preoperative CCT by 1 month. Vasavada et al19 performed phacoemulsification of white mature cataracts and postoperatively, the mean corneal thickness increased by 14.3% on day 1 and returned to normal between 1 and 3 months. Ermis et al12 noted an increase in corneal thickness of 12.8% (range, 537–606 μm) on the day after phacoemulsification of white mature cataract using trypan blue staining under viscoelastic. The subsequent CCT at 1 week, 1 month, and 3 months were 575, 555, and 544 μm, respectively, and were comparable to our study.
Corneal thickness, however, has been found to insufficiently reflect the degree of surgical trauma and endothelial status.20 A study comparing the corneal thickness and endothelial density before and after phacoemulsification showed no correlation between the two parameters. Corneal thickness does not reflect endothelial cell loss unless the physiological threshold has been breached. The mean loss of endothelial cells after phacoemulsification was reported to be 16% by Ventura et al.19 However, the nucleus density of the cataracts was not stated. Vasavada et al20 noted a mean cell loss of 18.6% six months after phacoemulsification of white mature cataracts. It was 7.3% as reported by Van Dooren et al16 12 months after phacoemulsification of submature cataract with the use of trypan blue 0.06%, with no significant difference compared with the control eyes with no staining. For phacoemulsification of white cataract together with the use of trypan blue, the mean central endothelial cell loss was 8.5%.10 However, ECD was only available in 71.2% of subjects. In our study, the mean ECD loss at the end of 3 months was 11.9% and no significant difference was found between the air and the viscoelastic groups.
Both the staining techniques under air or under viscoelastic have advantages and disadvantages (Table 6). A reported disadvantage of the staining under air technique is that the anterior chamber becomes unstable and easily collapses with insertion of the cannula. This situation was occasionally encountered during the study and several injections of air to maintain the anterior chamber may be required. It has been suggested that a small amount of high-density viscoelastic agent injected at the incision may help to maintain the anterior chamber.2 The drawback of staining under viscoelastic is the potential for the trypan blue dye at the viscoelastic-anterior capsule interface to obscure the visibility for CCC. This can be prevented by a viscoelastic exchange, but may add extra cost to the surgery due to an extra volume of viscoelastic was sometimes required. Besides staining under air or viscoelastic, other modifications of the staining procedure have been attempted. Kayikicioglu et al13 mixed trypan blue 0.4% with sodium hyaluronate 1% and injected it onto the anterior capsule under the air bubble. Toprak et al14 devised a modified air cannula to increase coverage area to facilitate staining. However, with application of trypan blue through two paracentesis as in our study, adequate coverage of the anterior capsule with trypan blue can be achieved when staining under viscoelastic.
Other than the difficulty in performing a complete CCC, another challenge in phacoemulsification of white cataract is the difficulty in assessing the nucleus hardness preoperatively as it is often camouflaged by the white cortex. The density of the nucleus correlates with the need for increased ultrasound energy and fluid use and subsequent endothelial trauma. Up to 50% of patients were found to have very hard nucleus in a study of phacoemulsification of white mature cataracts.19 In this study, 34.6% of eyes were found to have nucleus hardness of 3+ or above and significantly longer phacoemulsification times were required for these cases.
There are several limitations to our study. Firstly, the assessment of the nucleus hardness was not masked and biases might have been introduced during grading of the nuclear density. Secondly, the exact phacoemulsification power used during surgery was not known and comparison of phacoemulsification times alone may be misleading. Finally, there might have been some surgical trauma to the endothelium during the operation and the long-term effects on endothelium were not evaluated in this study.
With the use of trypan blue for capsular staining, phacoemulsification of white mature cataract can be performed with good surgical and visual outcomes. Both trypan blue staining of the anterior lens capsule under air or under viscoelastic appeared to be safe and effective methods, the choice of procedure may therefore rest on the surgeons' preference.
References
Gimbel HV, Neuhann T . Development, advantages and methods of the continuous circular capsulorhexis technique. J Cataract Refract Surg 1990; 16: 31–37.
Pandey SK, Werner L, Escobar-Gomez M, Roig-Melo EA, Apple DJ . Dye-enhanced cataract surgery. Part 1: anterior capsule staining for capsulorhexis in advanced/white cataract. J Cataract Refract Surg 2000; 26: 1052–1059.
Hoffer KJ, McFarland JE . Intracameral subcapsular fluorescein staining for improved visualization during capsulorhexis in mature cataracts. J Cataract Refract Surg 1993; 19: 566.
Fritz WL . Fluorescein blue, light-assisted capsulorhexis for mature or hypermature cataract. J Cataract Refract Surg 1998; 24: 19–20.
Horiguchi M, Miyake K, Ohta I, Ito Y . Staining of the lens capsule for circular continuous capsulorhexis in eyes with white cataract. Arch Ophthalmol 1998; 116: 535–537.
Pandey SK, Werner L, Apple DJ . Staining the anterior capsule. J Cataract Refract Surg 2001; 27: 647–648.
Yi DH, Sullivan BR . Phacoemulsification with indocyanine green versus manual expression extracapsular cataract extraction for advanced cataract. J Cataract Refract Surg 2002; 28: 2165–2169.
Guo S, Caputo A, Wagner R, DeRespinis P . Enhanced visualization of capsulorhexis with indocyanine green staining in pediatric white cataract. J Pediatr Ophthalmol Strabismus 2003; 40: 268–271.
Melles GR, de Waard PW, Pameyer JH, Beekhuis WH . Trypan blue capsule staining to visualize the capsulorhexis in cataract surgery. J Cataract Refract Surg 1999; 25: 7–9.
Jacob S, Agarwal A, Agarwal A, Agarwal S, Patel N, Lal V . Trypan blue as an adjunct for safe phacoemulsification in eyes with white cataract. J Cataract Refract Surg 2002; 28: 1819–1825.
Yetik H, Devranoglu K, Ozkan S . Determining the lowest trypan blue concentration that satisfactorily stains the anterior capsule. J Cataract Refract Surg 2002; 28: 988–991.
Ermis SS, Ozturk F, Inan UU . Comparing the efficacy and safety of phacoemulsification in white mature and other types of senile cataracts. Br J Ophthalmol 2003; 87: 1356–1359.
Kayikicioglu O, Erakgun T, Guler C . Trypan blue mixed with sodium hyaluronate for capsulorhexis. J Cataract Refract Surg 2001; 27: 970.
Toprak AB, Erkin EF, Guler C . Trypan blue staining of the anterior capsule under an air bubble with a modified cannula. Ophthalmic Surg Lasers Imaging 2003; 34: 236–238.
Bhartiya P, Sharma N, Ray M, Sinha R, Vajpayee RB . Trypan blue assisted phacoemulsification in corneal opacities. Br J Ophthalmol 2002; 86: 857–859.
Van Dooren BT, De Waard PW, Poort-van Nouhuys H, Beekhuis WH, Melles GR . Corneal endothelial cell density after trypan blue capsule staining in cataract surgery. J Cataract Refract Surg 2002; 28: 574–575.
Singh AJ, Sarodia UA, Brown L, Jagjivan R, Sampath R . A histological analysis of lens capsules stained with trypan blue for capsulorrhexis in phacoemulsification cataract surgery. Eye 2003; 17: 567–570.
Chakrabarti A, Singh S . Phacoemulsification in eyes with white cataract. J Cataract Refract Surg 2000; 26: 1041–1047.
Vasavada A, Singh R, Desai J . Phacoemulsification of white mature cataracts. J Cataract Refract Surg 1998; 24: 270–277.
Ventura AC, Walti R, Bohnke M . Corneal thickness and endothelial density before and after cataract surgery. Br J Ophthalmol 2001; 85: 18–20.
Author information
Authors and Affiliations
Corresponding author
Additional information
Financial Interest and Support: Nil
This paper was presented in part in the XXII Congress of the ESCRS, Paris, September 2004
Rights and permissions
About this article
Cite this article
Wong, V., Lai, T., Lee, G. et al. A prospective study on trypan blue capsule staining under air vs under viscoelastic. Eye 20, 820–825 (2006). https://doi.org/10.1038/sj.eye.6702032
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702032
Keywords
This article is cited by
-
Comparison of trypan blue and Brilliant Blue G for staining of the anterior lens capsule during cataract surgery: short-term results
International Ophthalmology (2019)
-
Cataract
Nature Reviews Disease Primers (2015)
-
Trypan blue dye for anterior segment surgeries
Eye (2011)