Abstract
Purpose
To investigate intraocular pressure (IOP) and ocular haemodynamics following small incision cataract surgery.
Methods
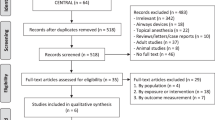
Systemic and ocular haemodynamics, and IOP, were measured pre-operatively and 1 month post-operatively, in 25 eyes of 25 patients (mean age 72.6±7.9 years) scheduled for small incision cataract surgery and intraocular lens implantation; these values were compared to an untreated age-matched healthy group (n=25, mean age 72.3±5.0 years). For each eye, the Ocular Blood Flow Analyser (OBFA, Paradigm Inc., UT, USA) was used to obtain measurements of IOP, pulsatile ocular blood flow (POBF), pulse volume (PV), ocular pulse amplitude (PA), and pulse rate (PR). Systemic blood pressure measurements were obtained at each visit. Pre- and post-operative values for the cataract group were compared using repeated measures analysis of variance, and compared to the normal group using analysis of variance.
Results
Pre-operatively, IOP was significantly higher in the cataract group compared to the age-matched normal control group (P<0.001). Cataract surgery resulted in a significant 16.7% reduction in IOP (P=0.001). Consequently, the post-operative IOP in the cataract group was similar to that of the normal group (P>0.05). Both pre- and post-operative POBF and PV values for the cataract group were significantly lower than for the normal age-matched group (P<0.0125). Small incision cataract surgery led to an 8.3% post-operative increase in POBF (P=0.0118) and 15.5% increase in PV (P<0.001). No changes in PA or PR were evident.
Conclusion These data suggest that cataract patients exhibit higher IOP and reduced ocular perfusion characteristics compared to an age-matched normal healthy group. Following cataract surgery, IOP reduced and ocular pulsatility improved.
Similar content being viewed by others
Introduction
Decreased intraocular pressure (IOP) following cataract extraction with posterior chamber lens implantation has been reported in the mid- to long-term for both normal and glaucomatous eyes.1, 2, 3, 4 This outcome, which has been attributed to a widening of the anterior chamber angle,5, 6, 7, 8 has positive implications for glaucomatous eyes resulting in a reduced requirement for IOP-lowering medication in at least one study.4
Hopkins9 carried out a pilot study investigating ocular haemodynamics in a small group of cataractous eyes and reported a 20–30% decrease in pulsatile ocular blood flow (POBF) compared to normal healthy volunteers. The effect of cataract surgery on ocular haemodynamics has also been considered: Spraul et al10 described a post-operative decrease in POBF and pulse amplitude at 3 days that was not apparent 12 months later, whereas Rainer et al11 reported no change in fundus pulse amplitude, or blood-flow velocities and resistance of the retrobulbar vessels up to 1 month following cataract surgery.
The pulsatile component of ocular blood flow is thought to be primarily choroidal in origin with minimal influence from the retinal and optic nerve head vasculature.12 While there is extensive evidence to suggest that retinal vessels autoregulate in order to maintain constant blood flow when ocular perfusion pressure (OPP) is altered,13 the case for effective autoregulation in the choroid is less convincing. Small increments in IOP have been shown to result in decreased POBF in normal healthy volunteers14, 15 and, to a greater extent, in normal tension glaucoma patients.15 Moreover, Lovasik et al14 have shown that a drop in IOP, through the release of a suction cup, is accompanied by an increase in POBF in normal healthy subjects. While the aforementioned studies reported altered POBF with IOP, others have failed to demonstrate a change and have therefore concluded that the choroid does autoregulate maintaining constant blood flow despite alterations in OPP.16
Given the known IOP reduction associated with cataract surgery and the limited autoregulatory capacity of the choroid, one may expect this combination to yield an improvement in POBF. To investigate this, the pre- and post-operative IOP and ocular haemodynamics of cataract patients undergoing small incision cataract surgery with intraocular lens implantation were compared to an untreated age-matched normal healthy group.
Methods
Subject sample
The study was of a pre- and post-surgical follow-up prospective design, with a normal control group. All procedures conformed to the Tenets of the Declaration of Helsinki and were approved by the research and ethics review board of Birmingham Heartlands and Solihull NHS Trust (UK), and Aston University, Birmingham (UK). Prior to enrolment, each subject gave his or her written informed consent.
In all, 25 eyes (12 right eyes and 13 left eyes) of 25 consecutive patients (mean age 72.6±7.9 years; eight male and 17 female) scheduled for small incision cataract surgery were included in the study. These were compared to a normal healthy control group (n=25) with the same gender and right/left eye distribution, and a similar mean age of 72.3±5.0 years (P>0.05). Cataract patients were included if they were free from cardiac disease, arterial hypertension and hypotension, and diabetes. Cataract patients were free from ocular disorders other than age-related cataract and had a visual acuity score of 6/12 or worse. Healthy volunteers, who were independently assessed by an optometrist for normality, were also free from systemic and ocular disease with a visual acuity score of 6/9 or better. In order to minimise any possible confounding vascular effects, none of the subjects smoked cigarettes or cigars, received nicotine in any form, and all were requested to abstain from caffeine-containing products for 24 h.
Procedures
All systemic and ocular measurements were performed in a single visit for the normal healthy group. The same measurements were obtained both pre-operatively (on the day of surgery) and 1 month post-operatively (after cessation of steroid treatment) for the cataract group. For each subject, measurements were carried out at the same time of day to minimise diurnal fluctuations in IOP and ocular blood flow. At each visit, the Ocular Blood Flow Analyser (OBFA Paradigm, USA) was used to measure IOP, POBF, ocular pulse volume (PV), ocular pulse amplitude (PA), and pulse rate (PR). Pneumotonometry measurements were acquired following topical anaesthesia with one drop of 0.4% benoxinate HCL (Minims®, Chauvin, UK). OBFA measurements were calculated automatically from five acceptable IOP pulses acquired during a 10-s recording. Previous studies reported good agreement between IOP measurements obtained with the OBFA and Goldmann tonometry, and the OBFA has been shown to be reliable for POBF measurements with intraclasss correlation coefficients ranging from 0.88 for intravisit reproducibility to 0.70 for intervisit reproducibility.17
Systemic measurements of systolic and diastolic blood pressure were performed with a standard oscillometric device. Arterial pulse pressure (APP) was calculated as systolic blood pressure−diastolic blood pressure. Mean arterial pressure (MAP) was calculated as diastolic pressure +1/3 arterial pulse pressure. Mean ocular perfusion pressure (OPP) was calculated as 2/3 MAP−IOP.
For the cataract patients, small-incision cataract surgery was performed through a 2.5 mm wide posterior limbal incision after peribulbar block consisting of 5–10 ml of 4% Citanest (Prilocaine hydrochloride 40 mg) and hyaluronidase. Following phacoemulsification, a foldable intraocular lens was inserted in the capsular bag. Cataract patients were then treated postoperatively with Betnesol-N six times daily for 3 weeks.
Statistical analysis
A Student's two-tailed paired t-test was used to compare the mean ages of the two subject groups. For each group, stepwise multiple regression (by the forward step-up method) was used to search for possible effects of the systemic blood pressure variables on POBF, PV, PR, and PA. Stepwise regression analysis revealed no significant effects and consequently covariates were not required for the following statistical models. For the cataract group, repeated measures analysis of variance (REANOVA) was used to compare pre- and post-operative ocular and systemic haemodynamic parameters. Analysis of variance (ANOVA) was then used to compare the pre- and post-operative cataract group data to the normal age-matched group. In each case, a P-value of less than 0.0125 was considered statistically significant (Bonferroni corrected).
Results
No significant difference in age was observed between the normal and cataract group (P>0.05).
Age-matched normal subjects vs pre-operative cataract patients
No significant differences were observed between the systemic blood pressure measurements or OPP for the normal healthy group compared to the pre-operative cataract patients (Table 1). The mean±SD for the OBFA parameters are given in Table 2. Compared to the normal group, IOP was 33.9% higher in the pre-operative cataract patients (P<0.001; Figure 1). In comparison to the age-matched normal subjects, no significant difference was noted for ocular PA or PR, however, POBF and PV was significantly lower in the pre-operative cataract patients (24.8%, P=0.0001 and 32.5%, P<0.0001, respectively; Figures 2 and 3).
Cataract patients: effect of surgery
For the cataract group, a significant decrease in systolic blood pressure and hence MAP was apparent 1 month post-operatively (P=0.011 and 0.005, respectively), however, OPP did not change (P=0.248) (Table 1). Given the change in blood pressure, it was necessary to investigate a possible systemic effect on the ocular haemodynamic parameters, however, stepwise multiple regression analysis did not reveal any significant correlations between the systemic variables and POBF, PV, PR, or PA (P>0.05). IOP showed a significant 16.7% decrease from 16.3±2.9 mmHg pre-operatively to 13.6±2.5 mmHg post-operatively (P=0.005, Figure 1). POBF increased by 8.3% from 13.6±4.1 μl/s pre-operatively to 14.73±4.0 μl/s post-operatively (P=0.012), while PV increased by 14.5% (P<0.001) 1 month post-operatively (Figures 2 and 3). No significant change in ocular PR or PA was noted between the two visits (Table 2).
Age-matched normal subjects vs postoperative cataract patients
No significant differences were observed between the normal healthy group and the cataract patients measured post-operatively for systemic blood pressure or OPP (Table 1). Compared to the normal subject group, no significant difference in IOP was evident in the post-operative cataract patients (P=0.086; Figure 1). Compared to the normal group, POBF was 18.6% lower in the cataract group measured post-operatively (P=0.0025; Figure 2) and PV was 22.3% lower (P=0.005; Figures 2 and 3). No significant difference was noted for ocular PA or PR between the normal group and post-operative cataract values.
Discussion
Overall, IOP was higher, and POBF and PV were lower in the cataract patients measured pre-operatively compared to the normal age-matched healthy group. A significant reduction in IOP occurred following small incision cataract surgery and IOL implantation in the cataract group, and consequently, the post-operative IOP did not differ significantly from the normal age-matched group. While a post-operative improvement in ocular perfusion was apparent in the cataract group, this was still significantly lower when compared to the normal age-matched group. The drop in IOP observed after 1 month following cataract surgery was in agreement with previous investigations in which IOP has been reported to decrease post-operatively in the mid- to long-term.1, 2, 3, 4 A post-operative reduction in systemic blood pressure also occurred, however, patients are generally anxious on the day of their operation and more relaxed post-operatively that may have accounted for the observed change. The reduction in IOP and parallel reduction in systemic blood pressure in the cataract group post-operatively meant that OPP remained stable between visits.
The association between cataract and reduced ocular pulsatility characteristics in this study is supported by previous work from Hopkins,9 who reported a 20–30% reduction in POBF in cataractous compared to healthy eyes, perhaps suggesting a causal link between ocular pulsatility and cataractogenesis. In the present study, ocular PV measured in the cataractous eyes was also substantially lower than that for the normal age-matched group. While this deviation from normal persisted for both OBFA parameters in the cataract group, it was less prominent post-operatively. Reduced ocular perfusion may contribute directly to cataractogenesis, perhaps due to a metabolic imbalance in eyes with compromised perfusion characteristics. However, it is difficult to be certain whether the reduced perfusion observed in this study was a cause or consequence of cataract development. It is also likely that such metabolic effects would be distributed differently across different cataract types; a larger study investigating the metabolic status across various sample groups of cataract patients would be required to explore this. In the present study, as patients were recruited on a consecutive basis as those requiring small incision cataract surgery, while the majority had nuclear sclerosis cataract, co-existing cataract classifications were not excluded.
Although not statistically significant, PA was lower in the cataract group both pre- and post-operatively when compared to the normal age-matched group; a trend in keeping with the reduced pulsatility characteristics of the cataract group. Rainer et al10 found no change in fundus pulse amplitude up to 1 month following cataract surgery and no significant change in ocular pulse amplitude was apparent in this study in the cataract group post-operatively. A previous investigation by our group noted that a change in corneal curvature influenced PA, whereas, IOP remained unaffected.18 Corneal changes have previously been noted following cataract surgery,19, 20, 21 and while small-incision procedures minimise corneal changes, this possibility cannot be ruled out. Corneal curvature was not measured in this study, however, it is conceivable that a post-operative shift in corneal curvature could have masked a change in PA.
The calculation of POBF is dependent on a number of assumptions: blood outflow from the eye is thought to be nonpulsatile and the ocular pressure–volume relationship is presumed to be valid with constants applied for ocular and scleral rigidity. In any study in which there is a change in IOP, the validity of the OBFA parameters are reliant on an accurate pressure–volume relationship. This fundamental relationship has been validated on living human eyes for a range of IOPs;22, 23, 24 furthermore, modern cataract surgery has not been reported to have a significant effect on scleral rigidity.9 Therefore, acknowledging the assumptions of the relationship to be precise and any influence of change in ocular elasticity to be negligible, a post-operative rise in POBF and PV appears to have occurred in the cataract patients in this study that was still significantly below the normal age-matched levels.
The ratio of pulsatile to nonpulsatile flow remains the subject of much discussion with some studies concluding that the steady component is responsible for up to 50% of total flow25 and others reporting that the pulsatile component constitutes as much as 80%.26, 27 In some circumstances, a rise in POBF may represent a shift from non-pulsatile to pulsatile flow, and may not necessarily imply an increase in total ocular blood flow. Given that OPP for the cataract group did not differ significantly from the normal age-matched group, and that the post-operative OPP was similar to the pre-operative OPP level, any subsequent change in ocular perfusion measures could not be attributable to choroidal autoregulatory insufficiency. Instead, a post-operative increase in ocular PV appears to account for the increase in POBF. Further, it might be argued that at lower IOP, the ratio between pulsatile and non-pulsatile flow could be reduced, even in the presence of stable OPP, and in these circumstances one might have expected ocular pulsatility to fall.
This study was carefully controlled to exclude sources of variation known to affect blood flow. All of the subjects were nonsmokers, completely free from cardiac disorders, diabetes and hypertension, and were not receiving any medication known to affect blood flow. The cataract patients had ceased steroid medication before post-operative measurements were taken. In addition, all subjects underwent strict caffeine restrictions and were tested at the same time of day in the sitting position.
The follow-up period of 1 month in this study gave an interpretation of the IOP and haemodynamic postsurgical state of the eye in the mid-term, however, a longer follow-up would be required to determine whether this represented a transient or lasting effect. Given the advanced age of both groups, a small degree of lens opacification could not be ruled out in the control group; however, each control subject was independently assessed for normality with a visual acuity of 6/9 or better. While the reduction in IOP following cataract surgery may have been attributable to opening of the irido-corneal angle, this was not graded and could not, therefore, be correlated with the level of IOP reduction. Moreover, it is conceivable that the lowering of IOP observed for the cataract group may have been the result of other surgery-related characteristics such as irrigation or alteration of the trabecular meshwork. Given the significantly higher pre-operative IOP in the cataract group compared to the untreated age-matched normal control group, a correlation between cataract and IOP may exist. A larger investigation of IOP in cataract patients and normal controls would be required to verify this finding.
In summary, pre-operative cataract patients exhibited a slightly higher IOP and reduced ocular perfusion characteristics compared to an age-matched normal healthy group. A reduction in IOP was accompanied by an improvement in ocular haemodynamics at one month following cataract surgery. The surgical outcome of improved ocular perfusion and decreased IOP will be beneficial to cataractous eyes with or without coexistent glaucoma.
References
Steuhl KP, Marahrens P, Frohn C, Frohn A . Intraocular pressure and anterior chamber depth before and after extracapsular cataract extraction with posterior chamber lens implantation. Ophthalmic Surg 1992; 23: 233–237.
Tennen DG, Masket S . Short- and long-term effect of clear corneal incisions on intraocular pressure. J Cataract Refract Surg 1996; 22: 568–570.
Shingleton BJ, Gamell LS, O'Donoghue MW, Baylus SL, King R . Long-term changes in intraocular pressure after clear corneal phacoemulsification: normal patients versus glaucoma suspect and glaucoma patients. J Cataract Refract Surg 1999; 25: 885–890.
Hayashi K, Hayashi H, Nakao F, Hayashi F . Effect of cataract surgery on intraocular pressure control in glaucoma patients. J Cataract Refract Surg 2001; 27: 1779–1786.
Greve EL . Primary angle closure glaucoma: extracapsular cataract extraction or filtering procedure? Int Ophthalmol 1988; 12: 157–162.
Gunning FP, Greve EL . Uncontrolled primary angle closure glaucoma: results of early intercapsular cataract extraction. Int Ophthalmol 1991; 15: 237–247.
Gunning FP, Greve EL . Lens extraction for uncontrolled angle-closure glaucoma: long term follow-up. J Cataract Refract Surg 1998; 24: 1347–1356.
Obstbaum SA . The lens and angle-closure glaucoma (editorial). J Cataract Refract Surg 2000; 26: 941–942.
Hopkins SD . Ocular haemodynamics in cataractous eyes; a pilot study. Acta Ophthalmol 1989; 191(Suppl): 43–48.
Spraul CW, Amann J, Lang GK . Effect of cataract extraction with intraocular lens implantation on ocular haemodynamics. J Cataract Refract Surg 1996; 22: 1091–1096.
Rainer G, Kriss B, Dallinger S, Menapace R, Findl O, Schmetterer K et al. Effect of small incision cataract surgery on ocular blood flow in cataract patients. J Cataract Refract Surg 1999; 25: 964–968.
Langham ME, Farell MA, O'Brien V . In: Lambrou GN, Greve EL (eds). Non-invasive Measurement of Pulsatile Ocular Blood Flow in the Human Eye. Amsterdam: Kugler and Ghedini Publications, 1989, pp 93–99.
Riva CE, Grunwald JE, Petrig BL . Autoregulation of human retinal blood flow. An investigation with laser Doppler velocimetry. Invest Ophthalmol Vis Sci 1986; 27: 1706–1712.
Lovasik JV, Gagnon M, Kergoat H . A novel noninvasive videographic method for quantifying changes in the chromaticity of the optic nerve head with changes in the intraocular pressure, pulsatile choroidal blood flow and visual neural function in humans. Surv Ophthalmol 1994; 38(Suppl): S35–S51.
Quaranta L, Manni G, Donato F, Bucci MG . The effect of increased intraocular pressure on pulsatile ocular blood flow in low tension glaucoma. Surv Ophthalmol 1994; 38(Suppl): S177–S182.
Mittag TW, Serle J, Schumber R, Brodie, S, Stegman D, Schmidt KG et al. Studies of the ocular pulse in primates. Surv Ophthalmol 1994; 38(Suppl): S183–S190.
Spraul CW, Lang GE, Ronzani M, Högel J, Lang GK . Reproducibility of measurements with a new slit lamp-mounted ocular blood flow tonograph. Graefe's Arch Clin Exp Ophthalmol 1998; 236: 274–279.
Morgan AJ, Harper J, Hosking SL, Gilmartin B . The effect of corenal thickness and corneal curvature on pneumatonometer measurments. Curr Eye Res 2002; 25: 107–112.
Talamo JH, Stark WJ, Gottsch JD, Pratzer K, Cravy TV, Enger C . Natural history of corneal astigmatism after cataract surgery. J Cataract Refract Surg 1991; 17: 313–378.
Hayashi K, Nakao F, Hayashi F . Topographic analysis of early changes in corneal astigmatism after cataract surgery. J Cataract Refract Surg 1993; 19: 43–47.
Long DA, Monica ML . A prospective evaluation of corneal curvature changes with 3.0- to 3.5-mm corneal tunnel phacoemulsification. Ophthalmology 1996; 103: 226–232.
Eisenlohr JE, Langham ME, Maumenee AE . Manometric studies of the pressure volume relationships in living and enucleated eyes of individual human subjects. Br J Ophthalmol 1962; 46: 536–548.
Langham ME . Manometric, pressure-cup, and tonographic procedures in the evaluation in intraocular dynamics. Glaucoma Symposium, Tutzing Castle, Karger, New York, 1967.
Langham ME . Ocular blood flow and vision in healthy and glaucomatous eyes. Surv Ophthalmol 1994; 38(Suppl): S161–S168.
Krakau CET . A model for pulsatile and steady ocular blood-flow. Graefe's Arch Clin Exp Ophthalmol 1995; 233: 112–118.
Langham ME, To'mey KF . A clinical procedure for the measurements of the ocular pulse–pressure relationship and the ophthalmic arterial pressure. Exp Eye Res 1978; 27: 17–25.
Langham ME, Farrell RA, O'Brien V, Silver DM, Schilder P . Blood flow in the human eye. Acta Ophthalmol 1989; 67(S191): 9–13.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no proprietary interest.
Rights and permissions
About this article
Cite this article
Hilton, E., Hosking, S., Gherghel, D. et al. Beneficial effects of small-incision cataract surgery in patients demonstrating reduced ocular blood flow characteristics. Eye 19, 670–675 (2005). https://doi.org/10.1038/sj.eye.6701620
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701620
Keywords
This article is cited by
-
Optical coherence tomography angiography parameters after cataract surgery
International Ophthalmology (2023)
-
Macular vascular density and visual function after phacoemulsification in cataract patients with non-pathological high myopia: a prospective observational cohort study
Graefe's Archive for Clinical and Experimental Ophthalmology (2022)
-
Early changes in retinal microcirculation after uncomplicated cataract surgery using an active-fluidics system
International Ophthalmology (2021)
-
Optical coherence tomography angiography evaluation of the effects of phacoemulsification cataract surgery on macular hemodynamics in Chinese normal eyes
International Ophthalmology (2021)
-
Optic nerve head microvascular changes after phacoemulsification surgery
Graefe's Archive for Clinical and Experimental Ophthalmology (2019)