Abstract
Background:
We determined how CXC-chemokine signalling and necrosis factor-κB (NF-κB) activity affected heat-shock protein 90 (Hsp90) inhibitor (geldanamycin (GA) and 17-allylamino-demethoxygeldanamycin (17-AAG)) cytotoxicity in castrate-resistant prostate cancer (CRPC).
Methods:
Geldanamycin and 17-AAG toxicity, together with the CXCR2 antagonist AZ10397767 or NF-κB inhibitor BAY11-7082, was assessed by 3-(4, 5-Dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide assay in two CRPC lines, DU145 and PC3. Flow cytometry quantified apoptotic or necrosis profiles. Necrosis factor-κB activity was determined by luciferase readouts or indirectly by quantitative PCR and ELISA-based determination of CXCL8 expression.
Results:
Geldanamycin and 17-AAG reduced PC3 and DU145 cell viability, although PC3 cells were less sensitive. Addition of AZ10397767 increased GA (e.g., PC3 IC20: from 1.67±0.4 to 0.18±0.2 nM) and 17-AAG (PC3 IC20: 43.7±7.8 to 0.64±1.8 nM) potency in PC3 but not DU145 cells. Similarly, BAY11-7082 increased the potency of 17-AAG in PC3 but not in DU145 cells, correlating with the elevated constitutive NF-κB activity in PC3 cells. AZ10397767 increased 17-AAG-induced apoptosis and necrosis and decreased NF-κB activity/CXCL8 expression in 17-AAG-treated PC3 cells.
Conclusion:
Ansamycin cytotoxicity is enhanced by inhibiting NF-κB activity and/or CXC-chemokine signalling in CRPC cells. Detecting and/or inhibiting NF-κB activity may aid the selection and treatment response of CRPC patients to Hsp90 inhibitors.
Similar content being viewed by others
Main
There has been considerable interest in the clinical application of inhibitors of heat-shock protein 90 (Hsp90), particularly in cancer therapeutics (Smith et al, 1998; Maloney and Workman, 2002; Isaacs et al, 2003; Workman, 2004; Solit and Rosen, 2006). Heat-shock protein 90 is a molecular chaperone protein, the function of which is to ensure the correct folding of a well-defined group of client proteins, many of which have been shown to have a role in tumourigenesis (Jolly and Morimoto, 2000). Depending on its conformation, Hsp90 recruits various co-chaperones to assemble two distinct complexes, one of which favours proteasome-dependent degradation of the client protein and one that favours stabilisation (Meyer et al, 2003). Several classes of Hsp90 inhibitors have been developed, but the majority of research to date has been conducted exploiting the ansamycin class of inhibitors, of which the natural product geldanamycin (GA) and its synthetic analogue, 17-allylamino-demethoxygeldanamycin (17-AAG), are the best-known molecules. Geldanamycin and 17-AAG stabilise an Hsp90 conformation that recruits co-chaperones to target Hsp90 client proteins for proteasomal degradation (Mimnaugh et al, 1996; Roe et al, 1999). Both inhibitors have shown preclinical activity in a range of human cancer models, but GA was too toxic in animal testing to progress into the clinic. Furthermore, recent phase I clinical trials with 17-AAG or its primary metabolite, 17-dimethylaminoethylamino-17-demethoxygeldananmycin (17-DMAG), have determined tolerable toxicity with these agents and reported prolonged stable disease in treated patients (Maloney and Workman, 2002; Sausville et al, 2003; Pacey et al, 2006; Ramanthan et al, 2007; Solit et al, 2007; Pacey et al, 2009).
17-Allylamino-demethoxygeldanamycin has been shown to exhibit activity in a number of prostate cancer (CaP) models (Solit et al, 2002; Solit and Rosen, 2003). Although many CaP patients initially respond to therapy, a significant proportion of patients relapse after radiation therapy and/or androgen ablation therapy, leading to the acquisition of a castration-resistant, metastatic disease. Treatment options for patients with castration-resistant, metastatic CaP are very limited, principally because of the intrinsic chemoresistance acquired by cells during disease progression on therapy. Therefore, the potential to use Hsp90 inhibitors in this disease setting is an exciting and important prospect; treatment responses to 17-DMAG have been reported in two patients with castrate-resistant prostate cancer (CRPC) for 16 and 33 months in a phase I trial (Pacey et al, 2009).
CXCL8 (also known as interleukin-8) is a CXC chemokine that modulates the function of target cells through activation of two receptors, CXCR1 and CXCR2, which have a similar affinity for CXCL8 but otherwise exhibit markedly different selectivity for related CXC chemokines (Waugh and Wilson, 2008). Increased expression of CXCL8, CXCR1 and CXCR2 genes has been detected in CaP tissue through the exploitation of in situ hybridisation (Uehara et al, 2005) and/or immunohistochemistry (Murphy et al, 2005; Huang et al, 2005a), whereas increased levels of CXCL8 have been detected in the serum of patients with pathologically confirmed CaP (Veltri et al, 1999). Therefore, CaP cells and tumour stromal cells are subject to an increased CXC-chemokine signalling stimulus within the tumour microenvironment, underpinning a range of tumour-promoting functions (Waugh and Wilson, 2008; Waugh et al, 2008). In the context of CaP, CXCL8 expression correlates with increased angiogenesis, tumourigenicity and lymph node metastasis in vivo (Inoue et al, 2000; Kim et al, 2001). We, along with others, have shown that CXCL8 signalling contributes to the transition of a disease to a castration-resistant state (Araki et al, 2007; Seaton et al, 2008). Furthermore, we have shown that CXC-chemokine signalling (including CXCL8) modulates the sensitivity of CaP cells to environmental stresses such as hypoxia and chemotherapy agents, including the DNA-damage agents oxaliplatin and etoposide (Maxwell et al, 2007; Wilson et al, 2008a).
17-Allylamino-demethoxygeldanamycin has been shown to enhance the cytotoxicity of several conventional chemotherapeutic drugs in representative cell-based models of colorectal cancer and CaP (Munster et al, 2001; Rakitina et al, 2003; Vasilevskaya and O’Dwyer, 2005). The capacity of 17-AAG to reduce the activation of NF-κB has been proposed as a potential mode of action in sensitising cancer cells to oxaliplatin and 5-FU (Rakitina et al, 2003). However, the relevance of constitutive or ligand-induced NF-κB activity in directly regulating the sensitivity of cancer cells to Hsp90 inhibitors has not been studied extensively. Increased NF-κB activity has been reported in CaP cell lines and tissue (Fradet et al, 2004; Sweeney et al, 2004; Li et al, 2005; Huang et al, 2005b). Therefore, as Hsp90 inhibitors hold promise in treating CRPC, the objective of this study was to determine whether the intrinsic levels of NF-κB activity and/or constitutive CXC-chemokine signalling may correlate with and modulate the efficacy of Hsp90-targeted therapies in CRPC cells.
Materials and methods
Cell culture
PC3 and DU145 cells were sourced and cultured as previously described (MacManus et al, 2007; Maxwell et al, 2007).
Chemical and reagents
Chemicals were sourced from Sigma-Aldrich (St Louis, MO, USA), unless otherwise stated. BAY11-7082 was purchased from Calbiochem (La Jolla, CA, USA). AZ10397767 ((1R)-5-[[(3-chloro-2-fluorophenyl)methyl]thio]-7-[[2-hydroxy-1-methylethyl]amino]thiazolo[4,5-d]pyrimidin-2(3H)-one) was kindly provided by Dr Simon Barry and Dr David Blakey (AstraZeneca, Alderley Park, Cheshire, UK) (Walters et al, 2007).
3,3′-dihexyloxacarbocyanine iodide and propidium iodide staining
Cells were seeded into 24-well plates (1 × 105 cells per well) in RPMI 1640 medium and allowed to attach overnight. The CXCR2 antagonist AZ10397767 (20 nM) was added to the cells in conjunction with 17-AAG (1 nM or 1 μ M). Plates were incubated in a humidified chamber at 37°C with 5% CO2 for 72 h; thereafter, 3,3′-dihexyloxacarbocyanine iodide (DiOC6(3)) (40 nM) was added and the plates were incubated for a further 15 min. Propidium iodide (PI) (20 μg ml−1) was added, plates were returned to the incubator for 10 min and cells were collected (floating and adherent cells removed by trypsin). The cells were washed once in PBS and re-suspended in 500 μl PBS and analysed by flow cytometry (Beckman Coulter, Buckinghamshire, UK). Plots of FL1 (DiOC6(3)) vs FL4 (PI) were divided into quadrants to assess the percentage of cells living, cells undergoing necrosis and cells at early and late stages of apoptosis (Lecoeur et al, 2008).
Quantitative real-time PCR
RNA was harvested and prepared for analysis by quantitative real-time (qPCR) as previously described (Wilson et al, 2008a). The cDNA (50 ng) was mixed with primers (2 nM), sterile water and SYBR Green PCR mastermix (Finnzymes Diagnostics, Espoo, Finland). The primer sequences were as follows: 18s: forward: 5′-CATTCGTATTGCGCCGCT-3′, reverse: 5′-CGACGGTATCTGATCGTC-3′; HSP90: forward: 5′-AAAGCCCATCTGGACCAGAA-3′, reverse: 5′-AGCACGTCGTGGGACAAATA-3′. Primers for CXCL8 have been described previously. Standard cycling procedures were used with an annealing temperature of 55°C and an amplification temperature of 95°C. Specific amplicon formation with each primer pair was confirmed by melt curve analysis, and gene expression was quantified relative to an 18 s housekeeping gene.
Immunoblotting
Protein was prepared, resolved and blotted as described previously (Murphy et al, 2005; MacManus et al, 2007). Membranes were washed in Tris-buffered saline/0.1% Tween-20 (TBS-T), then blocked for 1 h at room temperature in 5% bovine serum albumin/TBS-T (BSA/TBS-T). Expression of Hsp90 was detected using an anti-human Hsp90 Ab (Cell Signaling Technology Inc, Danvars, MA, USA) at 1 : 1000 dilution in 5% BSA/TBS-T. The membranes were washed thrice in TBS-T and then incubated with a rabbit horse-radish peroxidase (HRP)-labelled secondary antibody (GE Healthcare UK Ltd, Buckinghamshire, UK). After three washes in TBS-T, the bands were detected using enhanced chemiluminescence (ECL plus reagents, Amersham Biosciences, Amersham, UK). Membranes were re-probed to ensure equal loading with GAPDH antibody (Biogenesis, Dorset, UK).
3-(4, 5-Dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide cell viability assays
Cells were seeded into 96-well plates (3 × 103 cells per well) in RPMI 1640 medium and allowed to attach overnight. Serial dilutions of 17-AAG or GA were added to the cells alone or in combination with AZ10397767 (20 nM). Plates were incubated in a humidified chamber at 37°C with 5% CO2 for 72 h; thereafter, 50 μl 3-(4, 5-Dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide (MTT) (2 mg ml−1) was added and the plates were returned to the incubator for 4 h. Medium and any non-metabolised MTT was aspirated from the wells and formazan crystals were dissolved in 100 μl dimethyl sulphoxide. Absorbance was read at 570 nm using a microplate reader (Molecular Devices, Wokingham, UK). Data were plotted using a nonlinear regression curve fitting algorithm (GraphPad Prism 4.0, La Jolla, CA, USA).
Luciferase reporter assays
The detection of NF-κB-driven transcriptional activity in unstimulated cells was determined using the NF-κB-LUC-pGL3 plasmid as previously described (Wilson et al, 2008a).
Statistical analysis
Student's t-test was used to compare means where appropriate. All tests were two-tailed.
Results
Inhibition of constitutive CXC-chemokine signalling confers cell-specific ansamycin-induced cytotoxicity in CRPC cells
Our experiments were conducted on two representative models of CRPC, the PC3 and DU145 cell lines. 3-(4, 5 -Dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide assays demonstrated that PC3 cells were differentially sensitive to GA and 17-AAG, with GA exhibiting greater activity (Figure 1A and B; Table 1). In contrast, DU145 cells were equally sensitive to these two agents (Figure 1C and D; Table 1). Interestingly, the DU145 cell line was also found to be markedly more sensitive to these ansamycin-based compounds in comparison with PC3 cells; GA was 17-fold more potent in DU145 cells, whereas the potency of 17-AAG was 275-fold greater in DU145 cells compared with PC3 cells.
Inhibition of CXC-chemokine signalling sensitises PC3 but not DU145 cells to ansamycin antibiotics, geldanamycin (GA) and 17-AAG. Survival curves representing cell viability in PC3 (A and C) cells and DU145 (B and D) cells, as measured by MTT assay, conducted after a 72 h exposure to increasing concentrations of either GA or 17-AAG. The consequence of inhibiting CXC-chemokine signalling on the effect of these compounds on cell viability was determined by co-administration of the CXCR2 antagonist AZ10397767 (AZ767) at a final concentration of 20 nM. Values are expressed as the mean±s.e.m. of five separate experiments.
We previously showed that inhibition of CXCR2 signalling can increase the sensitivity of CaP cells to conventional cytotoxic chemotherapeutic agents and death receptor ligands (Wilson et al, 2008a, 2008b). Therefore, we determined whether blockade of constitutive CXC-chemokine signalling using the CXCR2 receptor antagonist, AZ10397767, sensitised PC3 and DU145 cells to GA and 17-AAG. AZ10397767 was administered to cells concurrently at a concentration of 20 nM, exploiting its selectivity to block CXCR2 signalling. Addition of AZ10397767 to PC3 cells enhanced the cytotoxicity of both Hsp90 inhibitors, increasing the potency (IC50) of GA and of 17-AAG by three-fold and 3.5-fold, respectively (Table 1). However, analysis of data using nonlinear regression illustrated that the augmentation of 17-AAG cytotoxicity in PC3 cells was more striking at lower concentrations, wherein the calculated IC20 value was observed to have increased 68-fold after co-administration of AZ10397767 with 17-AAG. In marked contrast, the inhibition of CXCR2 signalling did not increase the cytotoxicity of either GA or 17-AAG in DU145 cells.
Inhibition of CXCR2 signalling potentiates 17-AAG-cytotoxicity through promotion of increased apoptosis and necrosis in CRPC cells
Experiments were conducted to determine the mechanism through which the inhibition of CXCR2 signalling may increase the sensitivity of PC3 cells to 17-AAG. Cultured PC3 cells demonstrate low levels of apoptosis (3–4% of total cells) and necrosis (1–2% of total cell population) under normal culture conditions. Administration of AZ10397767 on its own had a minimal effect on the basal level of necrosis detected in PC3 cells, whereas it had a modest effect in increasing the level of apoptosis (Figure 2A and B). Administration of 1 nM 17-AAG alone failed to induce apoptosis (Figure 2A) but selectively increased the level of necrosis detected in PC3 cells (Figure 2B). Co-administration of AZ10397767 with low-dose 17-AAG increased the level of apoptosis (P<0.01) but not necrosis in PC3 cells. The level of apoptosis detected from the combination of both drugs was similar to the effect of administering AZ10397767 alone. Administration of high concentrations of 17-AAG revealed the induction of both apoptosis and necrosis in PC3 cells. The levels of Hsp90-inhibitor-induced apoptosis and necrosis were increased when AZ10397767 was co-administered with 1 μ M 17-AAG; the increase in necrosis after addition of AZ10397767 was significant (P<0.05), whereas the increase in apoptosis bordered on statistical significance. These results suggest that this Hsp90-targeted agent is cytotoxic to PC3 cells by promoting both necrotic and apoptotic cell death, mechanisms that seem to be selectively induced in response to low and high concentrations of 17-AAG, respectively. Our results suggest that inhibition of CXCR2 signalling increases the efficacy of 17-AAG-induced apoptosis across the entire concentration–response curve, whereas it increases necrosis only at higher concentrations of 17-AAG.
Inhibition of CXC-chemokine signalling increases the ability of 17-AAG to induce both apoptosis and necrosis in PC3 cells. (A) Bar graphs representing flow cytometric analysis of PC3 cells stained with DiOC6(3) and propidium iodide to assess the consequence of inhibition of CXCR2 receptor signalling to the induction of apoptosis (A) and necrosis (B) by 72 h exposure to 17-AAG (1 nM or 1 μ M). This was determined by co-administration of the CXCR2 antagonist AZ10397767 at a final concentration of 20 nM. Values are expressed as the mean±s.e.m. of five separate experiments, *P<0.05; **P<0.01.
Inhibition of constitutive NF-κB activity enhances sensitivity of PC3 cells to 17-AAG
Initial experiments were designed to confirm the level of constitutive NF-κB activity in DU145 and PC3 cells. Using an NF-κB-specific luciferase reporter assay, we determined a 3.2-fold higher luciferase activity in transfected PC3 cells relative to transfected DU145 cells (P<0.01) (Figure 3A). Furthermore, qPCR-based determination of CXCL8 mRNA confirmed a marked elevation in the expression of this NF-κB-transcriptional target in PC3 cells relative to DU145 cells (P<0.001) (Figure 3B). We previously confirmed an equivalent expression of CXCR1 and CXCR2 receptors in these cell lines (Murphy et al, 2005).
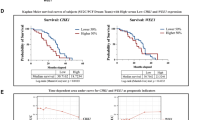
Inhibition of NF-κB signalling sensitises PC3 but not DU145 cells to 17-AAG. (A) Bar graph comparing the NF-κB transcriptional activity in PC3 and DU145 cells. This was determined using an NF-κB-driven luciferase activity in transiently transfected PC3 and DU145 cells. Cells were co-transfected with either NF-κB luciferase reporter (2 μg) or pGL3 basic vector (2 μg), and with Renilla luciferase reporter (0.02 μg), and incubated for 72 h before collection and analysis. Transfection efficiencies were adjusted relative to Renilla readouts and luciferase activities were normalised to pGL3 values. Values are expressed as the mean±s.e.m. of six separate experiments, **P<0.01. (B) Bar graph comparing IL-8 expression levels in PC3 and DU145 cells. Real-time PCR analysis of IL-8 mRNA transcript levels was used for this comparison. Values are expressed as the mean±s.e.m. of five separate experiments, ***P<0.001. (C and D) Survival curves representing cell viability in PC3 cells (C) and DU145 cells (D), as measured by MTT assay, conducted after a 72 h exposure to increasing concentrations of 17-AAG. The consequence of inhibiting NF-κB signalling on the effect of these compounds on cell viability was determined by co-administration of the NF-κB antagonist BAY-11-7082 (BAY) at a final concentration of 10 nM. Values are expressed as the mean±s.e.m. of five separate experiments, *P>0.05; **P<0.01. (E) Bar graph illustrating relative changes in CXCL8 mRNA transcript levels in PC3 cells after treatment with BAY-11-7082 for 6 h. Values are expressed as the mean±s.e.m. of five separate experiments, **P<0.01. (F) Bar graph illustrating the change in CXCL8 secretion detected by specific ELISA after treatment with BAY-11-7082 for 6 h. Values are expressed as the mean±s.e.m. of four separate experiments, *P<0.05.
3-(4, 5-Dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide assays were established to determine the relationship of constitutive NF-κB activity and the differential sensitivity of PC3 and DU145 cells to 17-AAG. Constitutive NF-κB activity was inhibited using a final concentration of 0.1 μ M BAY11-7082, chosen on the basis that this concentration of drug exhibited limited toxicity of its own to these CRPC cells. As before, increasing concentrations of 17-AAG resulted in a concentration-dependent decrease in PC3 cell viability. At each concentration used, the cytotoxicity of 17-AAG was enhanced in the presence of 0.1 μ M BAY11-7082 (Figure 3C), promoting a leftwards and parallel displacement of the concentration–response curve and equating it to a 4.1-fold increase in IC50 for 17-AAG in these cells. As seen before with AZ10397767, the presence of BAY11-7082 was shown to sensitise cells to low concentrations of 17-AAG (e.g., 10 nM 17-AAG). In contrast, administration of BAY11-7082 had no effect in potentiating the cytotoxicity of 17-AAG in DU145 cells (Figure 3D). This supports our hypothesis that constitutive NF-κB activity may account in part for the reduced sensitivity of PC3 cells to Hsp90 inhibitors.
The effect of adding BAY11-7082 on the endogenous levels of CXCL8 in CRPC cells was also confirmed by qPCR and ELISA. Administration of BAY11-7082 was shown to reduce the endogenous mRNA transcript level of vehicle-treated controls for CXCL8 to 30±8.3% (P<0.01) within 6 h (Figure 3E). Similarly, the rate of CXCL8 secretion from PC3 cells was similarly decreased after a 6 h exposure to BAY11-7082 (P<0.05) (Figure 3F). Therefore, these experiments establish a link between elevated constitutive NF-κB activity and increased endogenous CXCL8 expression in the PC3 cell line.
Further experiments were conducted to characterise how the co-administration of AZ10397767 with 17-AAG effected NF-κB transcriptional activity in PC3 cells. Using an NF-κB luciferase reporter assay, administration of AZ10397767 for 24 h was shown to induce a small but not statistically significant increase in NF-κB transcriptional activity in PC3 cells. In contrast, neither concentration (1 nM or 1 μ M) increased the activity of this transcription factor. However, co-administration of AZ10397767 with 1 nM 17-AAG was observed to decrease NF-κB transcriptional activity in PC3 cells (P<0.05) (Figure 4A). This result was further supported by analysis of CXCL8 mRNA expression, used in this context as a readout of NF-κB activity (again determined 24 h after the addition of drugs). By itself, the administration of AZ10397767 was shown to reduce the expression of CXCL8 mRNA to 73% of that determined in control cells (Figure 4B). Treatment with 1 nM 17-AAG and 1 μ M 17-AAG promoted concentration-dependent decreases in the constitutive CXCL8 mRNA levels determined in cells. The addition of AZ10397767, together with 1 nM 17-AAG, had a pronounced effect in reducing CXCL8 mRNA expression (P<0.01). No further decrease in CXCL8 mRNA levels was observed by the addition of AZ10397767 with the higher concentration of 17-AAG. This suggests that the addition of AZ10397767 to low concentrations of 17-AAG results in the maximal repression of NF-κB activity that can be exerted by these compounds in PC3 cells.
Effects of drug treatment on NF-κB activity in PC3 cells. (A) Bar graph illustrating the effects of 17-AAG and/or AZ10397767 administration on NF-κB transcriptional activity in PC3 cells. Drug-induced changes in NF-κB-driven luciferase activity were measured and adjusted, as previously described (legend to Figure 3), 24 h after addition of drugs. Values are expressed as the mean±s.e.m. of five separate experiments, **P<0.01. (B) Bar graph representing real-time PCR analysis of CXCL8 mRNA transcript levels in PC3 cells after 24 h exposure to 17-AAG (1 nM or 1 μ M). Cells were pre-treated for 4 h with 20 nM AZ10397767 or vehicle control to assess the effect on cellular IL-8 expression, used here as a readout of constitutive NF-κB transcription. Values are expressed as the mean±s.e.m. of five separate experiments, *P<0.05, **P<0.01.
CXC-chemokine signalling induces Hsp90 expression in CRPC cells through increased Hsp90 gene transcription
Our data indicate that elevated NF-κB activity and CXCL8 expression correlate with reduced sensitivity of PC3 cells to 17-AAG and that inhibition of either NF-κB or CXCR2 signalling increases the sensitivity of PC3 cells to this Hsp90 inhibitor. The induction of CXC-chemokine signalling is a well-characterised response of cells to stress. Therefore, we used qPCR assays and immunoblotting experiments to determine whether CXCL8 signalling regulated Hsp90 expression in CRPC cells. Addition of exogenous CXCL8, at a concentration of 3 nM, to both PC3 and DU145 cells resulted in a time-dependent increase in the expression of Hsp90 mRNA transcripts in both cell lines (Figure 5A, left and right panels). Although Hsp90 mRNA levels were increased in both cell lines, there was an apparent difference in the temporal regulation of Hsp90 transcripts between the two cell lines; stimulation with CXCL8 was shown to induce rapid increases in the transcription of the Hsp90 gene (2–4 h) in DU145 cells, whereas significant changes were only detected in PC3 cells 16 h after treatment with CXCL8.
Interleukin-8 induces Hsp90 gene transcription in CRPC cells. (A) Bar graphs representing real-time PCR analysis of Hsp90 mRNA transcript levels in PC3 (left panel) and DU145 (right panel) cells after stimulation with 3 nM rh-IL-8 for the indicated times. Values are expressed as the mean±s.e.m. of four and five independent experiments, respectively; *P<0.05; **P<0.01; ***P<0.001. (B and C) Bar graphs illustrating qPCR data for Hsp90 transcript levels in PC3 cells (left panels) and DU145 cells (right panels). Cells were pre-treated for 4 h with either the CXCR2 antagonist AZ10397767 at a final concentration of 20 nM (B) or BAY-11-7082 at a final concentration of 5 μ M (C), before stimulation with 3 nM rh-IL-8 for 24 h. Data shown are shown as mean±s.e.m., calculated from six independent experiments, *P<0.05; **P<0.01; ***P<0.001.
The link of CXCR2 and NF-κB signalling in underpinning CXCL8-promoted transcription of the Hsp90 gene in the two CRPC cell lines was investigated in a further series of experiments. Cells were stimulated with 3 nM CXCL8 in the absence and presence of 20 nM AZ10397767 for 24 h before analysis of Hsp90 mRNA transcript levels. Administration of AZ10397767 attenuated the CXCL8-induced increase in Hsp90 mRNA transcript levels in both PC3 and DU145 cells (Figure 5B, left and right panel). In addition, attenuation of NF-κB activity, effected by the co-administration of 5 μ M BAY11-7082, blocked the CXCL8-promoted increases in Hsp90 mRNA transcript levels in PC3 cells and DU145 cells (Figure 5C, left and right panel).
Administration of rh-CXCL8 was also shown to result in an increased Hsp90 expression at the protein level in DU145 cells, with peak increases in expression detected 4 and 6 h after stimulation (Figure 6B). In contrast, addition of CXCL8 failed to potentiate the protein expression of Hsp90 in PC3 cells under these experimental conditions (Figure 6A). PC3 cells exhibit higher levels of constitutive CXCL8 expression than do DU145 cells (Figure 3B), which may explain our inability to observe CXCL8-induced potentiation of Hsp90 protein expression in these cells. To test this, AZ10397767 and BAY11-7082 were administered to PC3 and DU145 cells for 16 h to determine whether the inhibition of constitutive CXC chemokine or NF-κB signalling in these cells altered Hsp90 expression. Densitometry analysis of immunoblots confirmed that, relative to internal controls, addition of AZ10397767 reduced the endogenous expression of Hsp90 to 70 and 45% in PC3 and DU145 cells, respectively, compared with that detected in vehicle-treated controls. Addition of the NF-κB inhibitor reduced endogenous expression of Hsp90 to ∼80% of untreated controls in either cell line (Figure 6C and D).
Interleukin-8 signalling regulates Hsp90 expression in DU145 cells. Immunoblots illustrating the expression of Hsp90 in cell lysates extracted from (A) PC3 and (B) DU145 cells stimulated with 3 nM rh-IL-8 for indicated times. Equal protein loading was confirmed by re-probing the membranes for GAPDH. (C) Immunoblot detecting levels of Hsp90 expression in the absence and presence of the CXCR2 inhibitor AZ10397767 (20 nM) and BAY11-7082 (5 μ M), administered to both PC3 and DU145 cells for 16 h. (D) Bar graph presenting densitometry analysis of the immunoblots presented in (C) above. The ratio of Hsp90/GAPDH expression is presented as a percentage of the ratio detected in controls.
Discussion
Our results identify a central role of NF-κB activity in modulating the response of CRPC cells to treatment with ansamycin-based Hsp90 inhibitors. Comparison of the relative potencies of GA- and 17-AAG cytotoxicity in the two CRPC cell lines reveals a reduced sensitivity of PC3 cells to each of the Hsp90-targeted therapeutic compounds, correlating with the elevated level of constitutive NF-κB transcriptional activity detected in these cells. Pharmacological inhibition of this constitutive NF-κB activity in these cells using BAY11-7082 resulted in an increased sensitisation of cells to 17-AAG. In contrast, addition of BAY11-7082 to the more sensitive DU145 cells had no effect on the potency of 17-AAG, consistent with the reduced activity of NF-κB detected in this cell line. Previous pre-clinical and clinical observations have suggested that Hsp90 inhibitors may be most effective when used as ‘chemomodulators’, exploiting their reported capacity to reduce NF-κB activity to sensitise metastatic cancer cells to chemotherapeutic and biological agents such as oxaliplatin and TRAIL (Rakitina et al, 2003). The data presented in this paper indicate that the efficacy of Hsp90 inhibitors themselves is enhanced when combined with direct inhibitors of NF-κB activity.
The relevance of NF-κB activity in determining the reduced sensitivity to ansamycin-based inhibitors of Hsp90 may be two-fold. First, NF-κB activity is known to confer a cell survival advantage through regulation of antiapoptotic gene expression. Thus, silencing of NF-κB activity will reduce the expression of known antiapoptotic proteins and may concurrently reduce the transcription and expression of other Hsp90-client proteins, many of which are critical to the survival of cells with oncogenic transformation. Our studies also show that the inhibition of NF-κB activity reduces chemokine-induced increases in mRNA transcript levels for Hsp90 in the PC3 cell line, indicating that NF-κB contributes to the transcriptional regulation of the Hsp90 gene in CRPC cells. Consequently, the elevated NF-κB activity in PC3 cells may define a multifaceted resistance that functionally antagonises Hsp90-directed therapeutic agents, initially through a promotion of compensatory survival signaling, and then through underpinning the increased expression of Hsp90 in these cells.
We have shown that exposure to chemotherapy agents induces NF-κB-driven CXC-chemokine signalling in CRPC cells (Wilson et al, 2008a, 2008b). These studies also characterise that CXC-chemokine signalling is coupled to NF-κB transcriptional activity and thus potentiates chemotherapy-induced activation of this transcription factor and downstream antiapoptotic gene expression (Wilson et al, 2008a, 2008b). Inhibition of this stress-induced CXC-chemokine signalling results in the sensitisation of CaP cells to chemotherapy and chemotherapy-induced apoptosis (Maxwell et al, 2007; Wilson et al, 2008a). In this study, we have shown that pharmacological inhibition of CXCR2 signalling results in a cell-dependent sensitisation of PC3 cells but not DU145 cells to the Hsp90 inhibitors, GA and 17-AAG. The capacity of AZ10397767 to increase ansamycin cytotoxicity in PC3 cells, especially at lower concentrations of 17-AAG, seems to be related to the reduced levels of constitutive NF-κB activity detected in PC3 cells receiving these compounds in combination. This was exemplified by direct measurements of NF-κB luciferase activity and by using analysis of CXCL8 gene transcription as a readout of NF-κB activity; co-administration of AZ10397767 with 1 nM 17-AAG attenuated transcriptional activity and reduced the level of constitutive CXCL8 mRNA transcripts detected relative to that in untreated cells or those treated with 17-AAG alone. Accordingly, we propose on the basis of this and previously published studies that the blockade of CXCR2 signalling using AZ10397767 (i) acts initially to inhibit the CXC-chemokine-promoted activation of NF-κB and (ii) as a consequence of that action, will promote a secondary response, suppressing NF-κB-promoted regulation of CXCL8 and anti-apoptotic gene expression. Consequently, the capacity to perturb NF-κB activity and selectively increase apoptosis levels provides a primary mechanism of action that explains the capacity of AZ10397767 to sensitise PC3 cells to Hsp90 inhibitors, especially at low concentrations of ansamycin compounds. The lower level of NF-κB activity detected in DU145 cells is consistent with the inability of either the CXCR2 receptor antagonist or the NF-κB inhibitor to potentiate the response of these cells to 17-AAG or GA.
We have also shown that CXC-chemokine signalling modulates the transcription of the Hsp90 gene in CRPC cells through a CXCR2-, NF-κB-mediated pathway. Interestingly, CXCL8-promoted Hsp90 gene regulation was biphasic in DU145 cells, suggesting that the regulation of this gene may be promoted through the action of multiple and temporally regulated transcription factors in this cell line. Administration of BAY11-7082 reversed the CXC-chemokine-promoted induction of Hsp90 mRNA transcripts in both cell lines, measured 24 h after the addition of stimulus, indicating that this later phase of transcriptional regulation is probably dependent on chemokine-promoted NF-κB activity. However, the transcription factor(s) underpinning the early increase in Hsp90 gene transcription in DU145 cells remain to be determined. Although an increased Hsp90 gene transcription was evident from qPCR analysis, immunoblotting experiments illustrated only quantitative increases in Hsp90 expression in CXCL8-stimulated DU145 cells. Transient blockade of constitutive CXC-chemokine signalling using the CXCR2 antagonist did reveal decreases in endogenous Hsp90 expression in both cells, confirming the importance of this receptor in regulating the transcription and expression of this chaperone protein. Therefore, as the CXCR2 antagonist reduces Hsp90 expression in both PC3 and DU145 cells, these data suggest that the sensitising effect of AZ10397767 on the cytotoxicity of Hsp90 inhibitors is more likely explained by the inhibition of constitutive NF-κB activity, as opposed to a direct modulation of Hsp90 expression.
Understanding the cellular response to Hsp90-targeted therapeutics is complex and multifaceted, given the extensive list of client proteins and pathways that are regulated by this protein. The underlying genetic dysfunction of tumour cells is likely to have a marked impact in determining the response of cells to Hsp90 inhibitors. For example, a functional retinoblastoma (Rb) protein has previously been shown to be required to promote ansamycin-mediated G1 arrest and apoptosis in breast cancer cells. Cells with defective Rb were subsequently shown to undergo mitotic arrest before the induction of apoptosis (Munster et al, 2001). In this study, we showed that cells with increased NF-κB activity are less sensitive to ansamycins and that inhibiting the constitutive activity of this transcription factor can sensitise CRPCs to 17-AAG. This observation may be important for consideration in future strategies aimed at exploiting Hsp90 inhibitors in the treatment of metastatic CaP, as nuclear distribution and increased NF-κB activity have been characterised in a significant proportion of advanced CaP cases (Fradet et al, 2004; Sweeney et al, 2004). It is already widely accepted that future clinical development of Hsp90 inhibitors is likely to see these agents being exploited in combination therapy as opposed to their use in monotherapy. Therefore, co-administration with agents that directly perturb NF-κB activity may provide a useful strategy to sensitise tumours to Hsp90-targeted therapy. Furthermore, analysis of diagnostic biopsy tissue for evidence of elevated NF-κB activity may prove to be a useful test to predict those tumours that are unlikely to show clinical response to ansamycin-based inhibitors.
In conclusion, these studies add to a series of studies illustrating the linkage of CXC-chemokine signalling to the development of chemoresistance in CaP cells. We have shown that constitutive NF-κB and/or CXC-chemokine signalling decreases the efficacy of Hsp90 inhibitors in a CRPC cell line that exhibits elevated activity and expression of these entities. This raises the prospect that elevated CXC-chemokine expression detected in patient serum and/or NF-κB activity in diagnostic biopsy specimens may serve as predictive biomarkers of tumour response to the Hsp90 inhibitors that are used in treating this disease.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Araki S, Omori Y, Lyn D, Singh RK, Meinbach DM, Sandman Y, Lokeshwar VB, Lokeshwar BL (2007) Interleukin-8 is a molecular determinant of androgen-independence and progression in prostate cancer. Cancer Res 67: 6854–6862
Fradet V, Lessard L, Begin LR, Karakiewicz P, Masson AM, Saad F (2004) Nuclear factor-kappaB nuclear localization is predictive of biochemical recurrence in patients with positive margin prostate cancer. Clin Cancer Res 10: 8460–8464
Huang J, Yao JL, Zhang L, Bourne PA, Quinn AM, di Sant’Agnese PA, Reeder JE (2005a) Differential expression of Interleukin-8 and its receptors in the neuroendocrine and non-neuroendocrine compartments of prostate cancer. Am J Pathol 166: 1807–1815
Huang YT, Pan SL, Guh JH, Chang YL, Lee FY, Kuo SC, Teng CM (2005b) YC-1 suppresses constitutive nuclear factor-kappaB activation and induces apoptosis in human prostate cancer cells. Mol Cancer Ther 4: 1628–1635
Inoue K, Slaton JW, Eve BY, Kim SJ, Perrotte P, Balbay MD, Yano S, Bar-Eli M, Radinsky R, Pettaway CA, Dinney CP (2000) Interleukin-8 expression regulates tumourigenicity and metastases in androgen-independent CaP. Clin Cancer Res 6: 2104–2119
Isaacs JS, Xu W, Neckers L (2003) Heat shock protein 90 as a molecular target for cancer therapeutics. Cancer Cell 3: 213–217
Jolly C, Morimoto RI (2000) Role of the heat shock response and molecular chaperones in oncogenesis and cell death. J Natl Cancer Inst 92: 1564–1572
Kim SJ, Uehara H, Karashima T, McCarty M, Shih N, Fidler IJ (2001) Expression of interleukin-8 correlates with angiogenesis, tumourigenicity and metastasis of human CaP cells implanted orthotopically in nude mice. Neoplasia 3: 33–42
Lecoeur H, Melki MT, Saidi H, Gougeon ML (2008) Analysis of apoptotic pathways by multiparametric flow cytometry: application to HIV-infection. Methods Enzymology 442: 51–82
Li Y, Ahmed F, Ali S, Philip PA, Kucuk O, Sarkar FH (2005) Inactivation of nuclear factor kappaB by soy isoflavone genistein contributes to increased apoptosis induced by chemotherapeutic agents in human cancer cells. Cancer Res 65: 6934–6942
MacManus CF, Pettigrew J, Seaton A, Wilson C, Maxwell PJ, Berlingeri S, Purcell C, McGurk M, Johnston PG, Waugh DJ (2007) Interleukin-8 signaling promotes translational regulation of cyclin D in androgen-independent prostate cancer cells. Mol Cancer Res 5: 737–748
Maloney A, Workman P (2002) Hsp90 as a new therapeutic target for cancer therapy: the story unfolds. Exp Opin Biol Ther 2: 3–24
Maxwell PJ, Gallagher R, Seaton A, Wilson C, Scullin P, Pettigrew J, Stratford IJ, Williams KJ, Johnston PG, Waugh DJ (2007) HIF-1 and NK-κB-mediated upregulation of CXCR1 and CXCR2 expression promotes cell survival in hypoxic CaP cells. Oncogene 26: 7333–7345
Meyer P, Prodromou C, Hu B, Vaughan C, Panaretou B, Piper WP, Pearl LH (2003) Structural and functional analysis of the middle segment of Hsp90: implications of ATP hydrolysis and client protein and cochaperone interactions. Mol Cell 11: 647–658
Mimnaugh EG, Chavany C, Neckers L (1996) Polyubiquitination and proteasomal degradation of the p185c-erbB-2 receptor protein tyrosine kinase induced by geldanamycin. J Biol Chem 271: 22796–22801
Munster PN, Basso A, Solit D, Norton L, Rosen N (2001) Modulation of Hsp90 function by ansamycins sensitises breast cancer cells to chemotherapy-induced apoptosis in an RB-and schedule dependent manner. Clin Cancer Res 7: 2228–2236
Murphy C, McGurk M, Pettigrew J, Santinelli A, Mazzucchelli R, Johnston PG, Montironi R, Waugh DJ (2005) Non-apical and cytoplasmic expression of interleukin-8, CXCR1 and CXCR2 correlates with cell proliferation and microvessel density in prostate cancer. Clin Cancer Res 11: 4117–4127
Pacey S, Banerji U, Judson I, Workman P (2006) Hsp90 inhibitors in the clinic. Handb Exp Pharmacol 172: 331–358
Pacey SC, Wilson R, Walton M, Eatock M, Zetterlund H, Arkenau H, Beecham R, Raynaud F, Workman P, Judson I (2009) A phase I trial of the HSP90 inhibitor, alvespimycin (17-DMAG) administered weekly, intravenously, to patients with advanced, solid tumours. Proc Am Soc Clin Onc (In press)
Rakitina TV, Vasilevskaya IA, O’Dwyer PJ (2003) Additive interaction of oxaliplatin and 17-allylamino-17-demethoxygeldanamycin in colon cancer cells lines results from inhibition of nuclear factor κB signalling. Cancer Res 63: 8600–8605
Ramanthan RK, Egorin MJ, Eiseman JL, Ramdingam S, Friedland D, Agarwala SS, Ivy SP, Potter DM, Chatta G, Zukowski EG, Stoller RG, Naret C, Guo J, Belani CP (2007) Phase I and pharmacodynamic study of 17-(allylamino)-17-demethoxygeldanamycin in adult patients with refractory advanced cancers. Clin Cancer Res 13: 1769–1774
Roe SM, Prodromou C, O’Brien R, Ladbury JE, Piper PW, Pearl LH (1999) The structural basis for inhibition of the Hsp90 molecular chaperone by the anti-tumour antibiotics radicicol and geldanamycin. J Med Chem 42: 260–266
Sausville EA, Tomaszewski JE, Ivy P (2003) Clinical development of 17-allylamino, 17-demethoxygeldanamycin. Curr Cancer Drug Targets 3: 377–383
Seaton A, Scullin P, Maxwell PJ, Wilson C, Pettigrew J, Gallagher R, O’Sullivan JM, Johnston PG, Waugh DJJ (2008) Interleukin-8 signalling promotes androgen independent growth of CaP cells via induction of androgen receptor expression and activation. Carcinogenesis 29: 1148–1156
Smith DF, Whitesell L, Katsanis E (1998) Molecular chaperones: biology and prospects for pharmacological intervention. Pharmacol Rev 50: 493–513
Solit DB, Rosen N (2003) Hsp90 as a therapeutic target in CaP. Semin Oncol 30: 709–716
Solit DB, Ivy SP, Kopil C, Sikorski R, Morris MJ, Slovin SF, Kelly WK, DeLaCruz A, Curley T, Heller G, Larson S, Schwartz L, Egorin MJ, Rosen N, Scher HI (2007) Phase I trial of 17-allylamino-17-demethoxygeldanamycin in patients with advanced cancer. Clin Cancer Res 13: 1775–1782
Solit DB, Zheng FF, Drobnjak M, Munster PN, Higgins B, Verbel D, Heller G, Tong W, Cordon-Cardo C, Agus DB, Scher HI, Rosen N (2002) 17-allylamino-17-demethoxygeldanamycin induces the degradation of androgen receptor and HER-2/neu and inhibits the growth of CaP xenografts. Clin Cancer Res 8: 986–993
Solit SB, Rosen N (2006) Hsp90: a novel target for cancer therapy. Curr Top Med Chem 6: 1205–1214
Sweeney C, Li L, Shanmugam R, Bhat-Nakshatri P, Jayaprakasan V, Baldridge LA, Gardner T, Smith M, Nakshatri H, Cheng L (2004) Nuclear factor-kappaB is constitutively activated in prostate cancer in vitro and is overexpressed in prostatic intraepithelial neoplasia and adenocarcinoma of the prostate. Clin Cancer Res 10: 5501–5507
Uehara H, Troncoso P, Johnston D, Bucana CD, Dinney C, Dong Z, Fidler IJ, Pettaway CA (2005) Expression of interleukin-8 gene in radical prostatectomy specimens is associated with advanced pathologic stage. Prostate 64: 40–49
Vasilevskaya IA, O’Dwyer PJ (2005) 17-Allylamino-17-demethoxygeldanamycin overcomes TRAIL resistance in colon cancer cell lines. Biochem Pharm 71: 580–589
Veltri RW, Miller MC, Partin AW, Poole EC, O’Dowd GJ (1999) Interleukin-8 serum levels in patients with benign prostatic hyperplasia and CaP. Cancer 91: 2322–2328
Walters IA, Austin C, Austin R, Bonnert R, Cage P, Christie M, Ebden M, Gardiner S, Grahames C, Hill S, Hunt F, Jewell R, Lewis S, Martin I, Nicholls D, Robinson D (2007) Structure-activity relationships of a series of thiazolopyrimidine-based CXCR2 antagonists. Bioorg Med Chem Lett 18: 798–803
Waugh DJ, Wilson C (2008) The Interleukin-8 signaling pathway in cancer. Clin Cancer Res 14: 6735–6741
Waugh DJ, Wilson C, Seaton A, Maxwell PJ (2008) Multi-faceted roles for CXC-chemokines in prostate cancer progression. Front Biosci 13: 4594–4604
Wilson C, Seaton A, Purcell C, Oladipo B, Pettigrew J, Maxwell PJ, Scullin P, O’Sullivan JM, Wilson RH, Johnston PG, Waugh DJJ (2008a) Chemotherapy-induced CXC-chemokine/CXC-chemokine receptor signaling in metastatic prostate cancer cells confers resistance to oxaliplatin through potentiation of nuclear factor-kappaB transcription and evasion of apoptosis. J Pharmacol Exp Ther 327: 746–759
Wilson C, Wilson T, Johnston PG, Longley DB, Waugh DJJ (2008b) Interleukin-8 signaling attenuates TRAIL and chemotherapy-induced apoptosis through transcriptional regulation of c-FLIP in prostate cancer cells. Mol Cancer Ther 7: 2649–2661
Workman P (2004) Combinatorial attack on multistep oncogenesis by inhibiting the Hsp90 molecular chaperone. Cancer Lett 206: 149–157
Acknowledgements
This work was supported by grants from the Association for International Cancer Research (AICR-04–516); and the Northern Ireland HPSS R&D Office (Grants RRG9.14 (DJJW). We gratefully acknowledge Drs Simon T Barry and David Blakey of AstraZeneca (Alderley Park, Cheshire) for provision of AZ10397767.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Seaton, A., Maxwell, P., Hill, A. et al. Inhibition of constitutive and cxc-chemokine-induced NF-κB activity potentiates ansamycin-based HSP90-inhibitor cytotoxicity in castrate-resistant prostate cancer cells. Br J Cancer 101, 1620–1629 (2009). https://doi.org/10.1038/sj.bjc.6605356
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6605356
Keywords
This article is cited by
-
Cathepsin K regulates the tumor growth and metastasis by IL-17/CTSK/EMT axis and mediates M2 macrophage polarization in castration-resistant prostate cancer
Cell Death & Disease (2022)
-
HSP90 inhibitor PU-H71 increases radiosensitivity of breast cancer cells metastasized to visceral organs and alters the levels of inflammatory mediators
Naunyn-Schmiedeberg's Archives of Pharmacology (2020)