Abstract
Background:
We investigated, in the panel of 60 human tumour cell lines of the National Cancer Institute (NCI-60), whether the R72P polymorphism of TP53 and the T309G polymorphism of MDM2 were associated to the in vitro cytotoxicity of anticancer agents, extracted from the NCI database. For validation, the same study was performed independently on a second panel of tumour cell lines, JFCR-45.
Methods:
Both SNPs were identified in cell DNA using PCR-RFLP techniques confirmed by direct sequencing and by pyrosequencing. For the analysis of the results, the mutational status of p53 was taken into account.
Results:
In the NCI-60 panel, the TP53 rare-allele frequency was 32% and the MDM2 rare-allele frequency 39%. The MDM2 alleles were distributed according to Hardy–Weinberg equilibrium whereas this was only found, for the TP53 alleles, in p53 non-mutated cell lines. Comparable results were obtained in the JFCR-45 validation set. The TP53 SNP had low impact on anticancer drug cytotoxicity in either panel. In contrast, the MDM2 gene polymorphism had a major impact on anticancer drug cytotoxicity, essentially in p53 non-mutated cell lines. Presence of the rare allele was associated to significantly higher MDM2 protein expression and to increased sensitivity to DNA-interfering drugs. In the JFCR-45 panel, a similar effect of the MDM2 gene polymorphism was observed, but was less dependent on the p53 mutational status.
Conclusions:
We hypothesised that cell lines harbouring the MDM2 G allele presented a lower availability of p53 for DNA repair, translating into higher sensitivity to DNA-damaging agents.
Similar content being viewed by others
Main
Numerous genetic factors influence the cytotoxicity of anticancer drugs and can explain, at least in part, the variability in individual responses to chemotherapy. Using in vitro models of the Centre d’Étude du Polymorphisme Humain, the group of ME Dolan at Chicago has evidenced the genetic components of drug response in non-tumour cells (Huang et al, 2007a, 2007b, 2008). We and others have used the NCI-60 model to show the relationships between the presence of a given polymorphic variation and the in vitro cytotoxicity of many anticancer drugs (Yarosh et al, 2005; Le Morvan et al, 2006; Moisan et al, 2006; Nief et al, 2007). The NCI-60 model consists of a panel of 60 human tumour cell lines of various origins which has served for the primary screening of thousands of potential anticancer drugs (Monks et al, 1991). The free availability of the databases elaborated by the Developmental Therapeutic Program (DTP) of the National Cancer Institute (NCI) allows to establish genotype/phenotype associations on a large number of drugs without performing drug cytotoxicity assays. The fact that the cell lines are of tumour origin adds a special advantage when the polymorphisms studied concern genes encoding drug targets or proteins involved in DNA repair, because the activity of such proteins in the tumour is expected to be important in drug cytotoxicity. On the contrary, polymorphisms in genes responsible for drug metabolism or transport would be more interesting to study in germ-line cells rather than in tumour cells, because they are expected to have a function in drug toxicity in the clinical setting.
The p53–MDM2 pathway is especially important for drug activity. Activation of p53 following exposure to cell stress leads to cell-cycle arrest and/or apoptosis and to DNA repair (Vogelstein et al, 2000). The loss of p53 function by oncogenic mutations provides cancer cells an opportunity to exacerbate their genetic instability and, hence, their tumourigenic and invasive properties (Lee et al, 1994). p53 is especially involved in response to DNA-damaging anticancer agents and TP53 mutations lead to the loss of apoptosis induced by these agents (Lowe et al, 1994). Many studies have tried to relate the occurrence of tumour TP53 mutations to drug activity with conflicting results (for reviews see Brown and Wouters, 1999; Gasco and Crook, 2003; Cimoli et al, 2004). For instance, when drug cytotoxicity is evaluated as inhibiting growth inhibition, cells bearing a TP53 mutation are significantly less sensitive to a wide range of drugs than cells with wild-type TP53; however, when drug cytotoxic activity is evaluated as cloning efficiency inhibition, no difference appears between cells with mutated and wild-type TP53 (Brown and Wouters, 1999). In the clinics, the question has not yet received definitive answers; it appears, however, that a loss of p53 function is frequently associated with resistance to treatment in several malignancies (Gasco and Crook, 2003). However, in a recent study on basal-like breast cancers treated by neo-adjuvant chemotherapy using an alkylating agent (cyclophosphamide), all tumours harbouring a mutated p53 presented a complete pathological response to treatment (Bertheau et al, 2007).
The TP53 gene bears a polymorphism in exon 4, resulting in the replacement of an arginine residue by proline (R72P). This polymorphism has been found with an allele frequency of about 25% in Caucasian populations, giving rise to about 6% variant homozygous subjects. It has been shown that the R common form of p53 is able to induce apoptosis markedly better than does the P variant form in cell lines containing inducible wild-type p53 (Dumont et al, 2003). In in vitro models, the response to anticancer drugs such as cisplatin and doxorubicin appears higher for the R allele than for the P allele (Yarosh et al, 2005). The p53 polymorphic status has been determined in the NCI panel and has been associated with a decrease in drug cytotoxicity of alkylating agents in heterozygous cell lines (Sullivan et al, 2004) as compared to both variant and common homozygous cell lines. In the clinical setting, it has been shown in a series of advanced head and neck cancers that the polymorphism in wild-type p53 influences the clinical outcome of the treatment, with significantly shorter survival in homozygous patients with the P variant allele (Bergamaschi et al, 2003). In contrast, opposite results were obtained for patients with tumours harbouring a mutated form of p53: patients with the P allele had higher response rates than those expressing the R allele. Another example comes from the study of the response of patients with breast cancer to adjuvant tamoxifen; the p53 R72P polymorphism appears as a predictor of tamoxifen response, and the authors suggest that patients with breast cancer lacking the P allele might be candidates for other therapies (Wegman et al, 2006).
An important regulator of p53 activity is MDM2. Exploration of the p53 stress response pathway led to the discovery of a functional polymorphism in the MDM2 intronic promoter (T309G, allele frequency around 30%) (Bond et al, 2004). The variant allele has been shown to have increased affinity to the MDM2 transcriptional activator Sp1, resulting in higher levels of MDM2 protein and subsequent attenuation of the p53 pathway. This polymorphism is associated with accelerated tumour formation in both hereditary and sporadic cancers (for a review see Bond and Levine, 2007) and a meta-analysis recently concluded that variant homozygote G/G was associated with a significantly increased risk of all types of tumours (Hu et al, 2007). Its possible effect on anticancer drug response remains to be established, but a recent study comparing cell lines with different MDM2 genotypes revealed a lower sensitivity of the G/G homozygous variant to topoisomerase II-interfering drugs (Nayak et al, 2007).
Materials and methods
We used in this study two independent sets of human tumour cell lines for which in vitro sensitivity to a panel of anticancer drugs had been established, the NCI-60 collection (Monks et al, 1991) and the JFCR-45 collection (Nakatsu et al, 2005). DNA extracts from 59 of the 60 NCI cell lines of the panel were kindly provided by Dr S Holbeck, Cancer Therapeutic Branch, NCI, Bethesda, MD, USA. One cell line, MDA-N, is no longer available in the panel. DNA extracts were prepared from 42 cell lines of the JFCR-45 collection.
Polymerase chain reactions (PCRs) were performed on genomic DNA using appropriate primers (see below). Polymorphisms were detected in the NCI-60 panel by restriction fragment length polymorphism (RFLP) analysis on PCR products, using appropriate restriction enzymes. Electrophoresis of the PCR products was performed before and after digestion on 10% polyacrylamide gels. The presence of a variation was translated into the occurrence or the disappearance of a restriction site on the PCR product, leading to two shorter products. This technique allowed the unambiguous discrimination between homozygous cell lines with the common-allele, homozygous cell lines with the rare-allele and heterozygous cell lines, for both polymorphisms studied (G466C of TP53, rs1042522 and T309G of MDM2, rs2279744). Sequencing was performed on randomly chosen PCR products from the various genotypes of the variations studied. Concordance with RFLP was obtained in 100% of the cases.
We used the following primers for the G466C variation (R72P) of TP53: sense, 5′-TCCCCCTTGCCGTCCCAA-3′; antisense, 5′-CGTGCAAGTCACAGACTT-3′. The PCR products were then digested by BstUI, which specifically cleaves the common G allele, and subjected to 10% polyacrylamide gel electrophoresis.
For the T309G variation of MDM2, we used the following primers: sense, 5′-GAGTTCAGGGTAAAGGTCAC-3′; antisense, 5′-TCAAGAGGAAAAGCTGAGTC-3′. The PCR products were digested by MspAI, which specifically cleaves the variant G allele, and subjected to 10% polyacrylamide gel electrophoresis.
To confirm these results by a second independent technique, we also identified both polymorphisms by pyrosequencing. The DNA extracts of the JFCR-45 collection were exclusively studied by pyrosequencing. Direct sequencing of the PCR fragments without any further purification was performed on the Pyrosequencer PyroMark ID system (Biotage, Uppsala, Sweden) according to the instructions of the manufacturer. In that case, the primers we used were as follows: for TP53: sense, 5′ dR-Biotin-CACTGAAGACCCAGGTCCAGAT 3′; antisense, 5′-CCGGTGTAGGAGCTGCTGG-3′; MDM2: sense, 5′-CAGGGTAAAGGTCACGGG-3′; antisense, 5′ dR-Biotin-AGGCACCTGCGATCATCC 3′.
After identification of the genotypes of each cell line, the 50% growth-inhibiting concentrations (GIC50) of 136 core drugs vis-à-vis the 59 NCI-60 cell lines, expressed as –log10(GIC50), were extracted from the DTP database (http://dtp.nci.nih.gov). Similarly, the growth-inhibitory concentrations (GI50s) of 53 agents against the cell lines of the JFCR-45 collection were extracted from the original publication (Nakatsu et al, 2005). Drugs were grouped as a function of their known mechanism of action into eight categories (for details see Scherf et al, 2000): alkylating or platinating agents acting on N7 of guanine; other alkylating agents, acting on N2 and O6 of guanine; antimetabolites; antifolates; topoisomerase I inhibitors; topoisomerase II inhibitors; spindle poisons, subdivided into vinca-alkaloid-type and taxane-type mechanisms of action. With each cell line collection independently, it was possible to directly compare the mean GIC50 values of each drug in the various genotypes, and it was also possible to use a paired Student's t-test to analyse the data related to drug classes.
The mutational status of TP53 of the NCI-60 collection was extracted from the NCI database, which integrates the data obtained by O’Connor et al (1997) and those obtained in the more recent study of Ikediobi et al (2006). There are some discrepancies between the two data sets and we chose the second one (Ikediobi et al, 2006) that results from genomic DNA resequencing. The JFCR cell lines had been also characterised for p53 mutational status by Frontier Science Co., Ltd (Ishikari, Hokkaido, Japan) according to the method described by Flaman et al (1995). The expression of MDM2 in the NCI-60 collection was extracted from the DTP database. Numerous different data sets are available, 1 obtained by mRNA dot blots and 20 by Affymetrix microarray analysis. Unfortunately, there were no available data obtained by RT–PCR, which is considered as the reference method to quantify mRNA products. We chose in the database the most recent data set (September 2008 release), which indeed presented good correlations with most other data sets (Affymetrix U133A microarrays generated by Dr E Moler, ref. GC232415). MDM2 expression was also obtained on Affymetrix microarrays in the JFCR-45 collection as described by Kanno et al (2006). Five MDM2 probe sets were available on these arrays; based on expression intensity, we chose the probe 217373_x_at for comparisons of MDM2 expression according to TP53 and MDM2 genotypes.
The χ2-test was used for comparing the distribution of the cell lines among genotypes. Pearson coefficients of correlation were computed for comparing continuous variables (GIC50 and gene expression data). To study the pharmacological parameters as a function of the genotype, we analysed the variances of drug GIC50s values or MDM2 expression for each genotype and calculated the significance of the differences in mean values, using a general linear model taking into account the unbalanced size of the groups. The Bonferroni correction was applied to take into account the number of tests performed. The two cell line collections were studied independently, the NCI-60 collection as a training test and the JFCR-45 collection as a validation test, to decrease the probability of generating falsely positive observations.
Results
Identification of TP53 and MDM2 genotypes
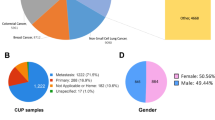
Figure 1 shows some representative electrophoretic profiles of PCR products before and after digestion with the appropriate restriction enzymes. Table 1 lists the 59 NCI cell lines and their genotypic status for the polymorphisms considered, as well as the p53 mutational status extracted from the NCI database. Some discrepancies between our results and those published earlier (Yarosh et al, 2005) were resolved by sequencing the complete exon 4, which confirmed the RFLP results. The results obtained by pyrosequencing were identical to those obtained by RFLP for all 59 cell lines. No special trend appeared concerning the presence or absence of a given genotype as a function of the tissue of origin of the cells. Concerning the TP53 variation (Table 2), there were 35 cell lines with the homozygous common-allele genotype G/G, 10 heterozygous cell lines G/C and 14 with the homozygous rare-allele genotype C/C, giving a rare-allele frequency of 32% if all cell lines were diploid. This distribution was significantly different from the expected Hardy–Weinberg distribution (P<0.001). When considering separately the cell lines with wild-type and mutated p53, it appeared that the frequency of the rare C allele was significantly higher (P=0.026) in cell lines with mutated p53 (38.4%) than in cell lines with wild-type p53 (15.6%). Especially, all the cell lines with the homozygous C/C genotype were found among the p53-mutated cell lines. In addition, the heterozygous cell lines harboured less frequently a p53 mutation than homozygous cell lines. Concerning the MDM2 variation (Table 2), there were 25 cell lines with the homozygous common-allele genotype T/T, 23 heterozygous cell lines T/G and 11 with the homozygous rare-allele genotype G/G, giving a rare-allele frequency of 38% and no significant distortion from a Hardy–Weinberg distribution. The same distribution was exhibited by cell lines with wild-type and mutated p53.
In the JFCR-45 panel, the rare TP53 allele frequency was 25% and the proportion of heterozygous cell lines was also significantly lower than expected from Hardy–Weinberg distribution (Table 2). However, due to the lower number of cell lines, it was not possible to detect a significant difference between the rare-allele frequency in the p53 wild-type and the p53 mutated cell lines. As in the NCI panel, the heterozygous cell lines harboured less frequently a p53 mutation than homozygous cell lines. The rare MDM2 allele frequency was 46% and the genotype distribution not significantly different from expected by the Hardy–Weinberg distribution (Table 2).
Associations between genotypes and gene expression and drug cytotoxicity
We looked for associations between the presence of a given genotype of TP53 and the cytotoxicity of individual drugs of the NCI database. The statistical analysis took into account the fact that multiple comparisons were made. When the whole NCI-60 panel was considered, several significant associations could be found between the TP53 variation and drug activity for some of the 136 drugs, such as fluorouracil, methotrexate, busulfan and cisplatin. The heterozygous cell lines appeared slightly more sensitive to these drugs than the rare-allele homozygous cell lines. Pooling the drugs as a function of their mechanism of action revealed that these differences were significant for alkylating agents (GIC50 ratio=1.4, P=7 × 10−6, Figure 2) and antifolates (GIC50 ratio=1.7, P=2 × 10−5, data not shown). However, these differences were not observed when the mutational status of p53 in the cell line panel was taken into account. Indeed, and independent of the polymorphisms of TP53, one can notice a highly significant difference between cell lines with wild-type and mutated p53: cell lines having a p53 mutation had a significantly lower sensitivity to most drugs than cell lines having no p53 mutation. The mean GIC50 ratio reaches 2 for alkylating agents (P=8 × 10−8, Figure 2) and 3 for antifolates (P=4 × 10−4, data not shown).
Schematic representation of the association between the TP53 genotype of the cell lines of the NCI-60 panel and the cytotoxicity of alkylating agents. The GIC50s of the drugs of this class towards the 60 cell lines, expressed as −log10(GIC50), were normalised to zero, the cytotoxicities higher than the mean with a positive sign and the cytotoxicities lower than the mean a negative sign. Data are means±s.e.m. Cells were either taken all together (left) or as a function of the p53 status (middle and right). White columns, common homozygous cell lines; grey columns, heterozygous cell lines; black columns, variant homozygous cell lines.
No consistent association between MDM2 genotype and cell sensitivity to the 136 core drugs could be evidenced when they were sought in the whole NCI-60 panel. When the drugs were pooled as a function of their mechanism of action, a significant difference could be evidenced for alkylating agents: the cell lines containing a G allele were slightly more sensitive to this class of agents than the common homozygous cell lines (GIC50 ratio=1.3, P=4 × 10−7, Figure 3). However, when the cell lines were analysed separately as a function of the presence or absence of p53 mutations, it appeared that the polymorphism in the MDM2 genes was associated with significant differences in drug cytotoxicity only in cell lines with wild-type functional p53, and not in cell lines harbouring a p53 mutation. In these cell lines, the presence of the rare G allele at position 309 of the MDM2 gene was associated to an important and significant increase in the cytotoxicity of numerous individual DNA-interfering drugs (alkylating agents, inhibitors of topoisomerases I and II) (Table 3). When the drugs were pooled as a function of their mechanism of action, it appeared that the mean GIC50 ratio of alkylating agents in cell lines with no G allele vs cell lines with a G allele reached 2.5 for alkylating agents (P=3.7 × 10−10, Figure 3), 2.2 for topoisomerase I inhibitors (P=5.1 × 10−7, data not shown) and 2.4 for topoisomerase II inhibitors (P=3.8 × 10−7, data not shown). Due to the fact that only two cell lines had a homozygous G/G genotype in the p53 wild-type subset, it was not possible to study them separately from heterozygous cell lines, but it should be noticed that these two cell lines presented the lowest GIC50 values for most DNA-interfering drugs.
Schematic representation of the association between the MDM2 genotypes of the cell lines of the NCI-60 panel and the cytotoxicity of alkylating agents. Same legend as Figure 2.
We also looked for associations between MDM2 expression and polymorphism in the NCI-60 panel. As expected, there was a significantly lower MDM2 expression in cell lines having a mutated p53 than in cell lines having no p53 mutation (expression ratio=1.57, P=1.5 × 10−5). There was no association between MDM2 polymorphism and MDM2 expression in the whole cell line panel; however, when the cell lines with and without a p53 mutation were considered separately, it appeared that, among the cell lines with no p53 mutation, those harbouring at least one G allele at position 309 of MDM2 had a significantly increased MDM2 expression (expression ratio=1.6, P=1.6 × 10−5) (Table 3 and Figure 4, right). This was not observed in p53-mutated cell lines (Figure 4, left). The association between MDM2 expression and anticancer drug cytotoxicity was only weak, despite the fact that MDM2 expression was higher in p53 wild-type cells, which are themselves more sensitive to DNA-damaging drugs. Especially, camptothecin and doxorubicin cytotoxicities were significantly correlated to MDM2 expression in p53 wild-type cells.
MDM2 gene expression as a function of the genotype of the cell lines of the NCI-60 panel. MDM2 expression was extracted from the DTP database (http://dtp.nci.nih.gov); the data set chosen originates from experiments on Affymetrix U133A microarrays realised by Dr E Moler, ref. GC232415. Cell lines with mutated p53 are on the left of the panel, and cell lines with wild-type p53 are on the right. White columns, common homozygous cell lines; grey columns, heterozygous cell lines; black columns, variant homozygous cell lines.
In the JFCR-45 panel, we observed, as in the NCI-60 panel, a significant relationship between the mutational status of p53 and the cytotoxicity of most anticancer drugs belonging to the classes of alkylating agents, topoisomerase inhibitors and antimetabolites. When the cytotoxic drug panel was considered as a whole, the mean ratio of GIC50 values between wild-type and p53-mutated cell lines was 1.35 (P=6.0 × 10−3). However, the TP53 polymorphism was not associated to differences in the cytotoxicity of any anticancer drug or drug class. The polymorphism of the MDM2 gene was in contrast associated, as in the NCI-60 panel, to major differences in drug sensitivity, the cell lines harbouring the variant MDM2 G allele being more chemosensitive than those harbouring only the common T allele; this was detected mainly in cell lines with wild-type p53 but also in cell lines where a mutation of p53 was detected, although to a lesser extent (Table 3). In p53 wild-type cell lines of the JFCR-45 panel, the mean GIC50 ratio of cytotoxic agents in cell lines with no G allele vs cell lines with a G allele reached 7.0 (P=2 × 10−10), whereas it was only 2.4 in p53-mutated cell lines. As in the NCI-60 panel, the expression of MDM2 in the JFCR-45 panel was higher in p53 wild-type cell lines than in p53-mutated cell lines (expression ratio=2.0, P=2 × 10−4) and, in p53 wild-type cell lines, MDM2 expression was higher in cell lines harbouring at least one G allele (expression ratio=1.9) (Table 3) but this did not reach significance (P=0.11) because of the small number of cell lines with common homozygous MDM2 genotype.
Discussion
The higher sensitivity of p53 wild-type cells, as compared to p53 mutated cells, to most anticancer agents (excluding spindle poisons), is a very general feature when cytotoxicity is evaluated by growth inhibition (Brown and Wouters, 1999). It was already observed by O’Connor et al (1997) in the NCI-60 panel and will not be further discussed here. The R72P polymorphism of p53 in the NCI panel had already been shown to be important in the cytotoxicity of several anticancer agents (Yarosh et al, 2005), especially those whose mechanism of action involves p53-mediated apoptosis. Yarosh et al (2005) had observed that the heterozygous cell lines were significantly more sensitive to alkylating agents than both common-allele and rare-allele homozygous cell lines. We found that this difference was significant only between heterozygous and rare-allele homozygous lines, but not between heterozygous and common-allele homozygous cell lines. The higher drug sensitivity of heterozygous cell lines in the NCI panel may be in fact related to the higher proportion of this genotype among the p53 non-mutated subset of the NCI-60 panel (31% vs 11% in the p53 mutated subset) and would not be a characteristic of the genotype. Indeed, there was no significant difference in drug sensitivity as a function of the TP53 polymorphism in the JFCR-45 panel, which confirms that the difference seen in the NCI panel should be a bias due to the distribution of the genotypes. However, this last observation is interesting per se: the higher proportion of heterozygotes among wild-type p53 tumours in both panels has never been mentioned before. It could be simply related to the loss of heterozygosity at the TP53 locus during evolution of p53 mutated, genetically unstable, tumours. It can also be hypothesised that the TP53 heterozygous genotype may protect against the occurrence of p53 mutations. Researching both the p53 mutational status and the TP53 polymorphism in clinical samples would be warranted to confirm this hypothesis.
The MDM2 gene is one of the numerous transcriptional targets of p53 and the MDM2 protein induces the proteasomal degradation of p53. Its polymorphism present in the 5′ untranslated region has been consistently associated with an increased transcription rate and a subsequent attenuation of p53, leading to an activation of tumour formation and growth (Bond and Levine, 2007). The most striking observation made in our study is that, in both cell line panels studied independently, this polymorphism may be important in the cytotoxicity of anticancer agents against tumour cell lines, and that, in the NCI-60 panel, this effect is limited to the tumours having no p53 mutation. The cell lines harbouring at least one variant G allele of MDM2 in this subset appeared 2- to 5-fold more sensitive to most DNA-interfering agents than the homozygous wild-type cell lines. This was not evidenced in cell lines with a mutated p53 and, therefore, should be related to the existence of a functional p53-dependent pathway. However, the higher drug sensitivity of the G allele-containing cell lines was observed in both p53 mutated and non-mutated cell lines of the JFCR-45 panel. This could be because not all p53 mutations exert the same effect on p53 function: it had been shown, for instance, that the 173H and the 273H mutations were able to induce apoptosis whereas most other mutations were not (Stähler and Roemer, 1998). A difference in the distribution of p53 mutations in the two panels could explain why the MDM2 gene polymorphism is associated to chemosensitivity in the p53-mutated subset of the JFCR panel and not on the corresponding subset of the NCI-60 panel. In addition, the presence of the rare G allele in both cell line panels was associated with an increase in MDM2 gene expression. This result was expected because the G allele of MDM2 has increased affinity to the MDM2 transcriptional activator Sp1.
The observation that the rare G allele of MDM2 is associated with increased drug cytotoxicity in these two models was unexpected, because the reduction of p53 availability in the variant cell lines would be suspected to lead to a decrease in drug-induced apoptosis and cell death. In addition, it was shown in recent studies that this polymorphism was associated with a worse outcome of cancer disease (Gryshchenko et al, 2008). However, no clinical study has evaluated separately the overall prognosis of the disease and the predictive function of the polymorphism on response to treatment. The degree of malignancy of a tumour cell is related, at least in part, to its rate of proliferation, as is its sensitivity to antiproliferative agents. In experimental models as in the clinical setting, the most rapidly growing tumours are also the most sensitive to anticancer drugs. It has been shown that, for instance, in a series of 431 patients with breast cancer the most aggressive tumours (SBR grade III) responded better to neo-adjuvant chemotherapy than the less aggressive ones (SBR grade I) (P<10−6) (Amat et al, 2002). Consequently, the overall prognosis of a cancer is not simply related to its responsiveness to chemotherapy. In the NCI-60 panel, the cell doubling times have been evaluated and are significantly correlated with chemosensitivity; however, no relationship could be evidenced between the polymorphisms studied and the cell doubling times, showing that the association between MDM2 polymorphism and drug cytotoxicity was independent from the rate of cell-cycle progression.
At the cellular level, it should be borne in mind that p53 is involved in many functions in the cell: it is not only in charge of inducing apoptosis in response to DNA damage (especially drug-induced DNA damage), but also of inducing DNA repair following drug-induced damage. One can hypothesise that the second function of p53 would be preponderant in the culture conditions of the cell line panels. As a consequence, the higher MDM2 activity associated with the variant genotype would be responsible for a decrease in p53-mediated DNA repair, which would explain in turn why the cytotoxicity of DNA-interfering agents is higher in cell lines harbouring the variant G allele of MDM2. One can also hypothesise that the variant allele brings an additional alkylation site of for agents whose mechanism of action involves covalent binding to a guanine, which is the case of most alkylators; in these conditions, the cytotoxicity of these agents would be dependent upon the number of G alleles in the promoter of the MDM2 gene. However, the higher drug sensitivity of T/G and G/G cell lines in comparison to T/T cell lines also applies to topoisomerase I-targeting and topoisomerase II-targeting drugs, rendering this mechanism unlikely.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Amat S, Penault-Llorca F, Cure H, Le Bouëdec G, Achard JL, Van Praagh I, Feillel V, Mouret-Reynier MA, Dauplat J, Chollet P (2002) Scarff-Bloom-Richardson (SBR) grading: a pleiotropic marker of chemosensitivity in invasive ductal breast carcinomas treated by neoadjuvant chemotherapy. Int J Oncol 20: 791–796
Bergamaschi D, Gasco M, Hiller L, Sullivan A, Syed N, Trigiante G, Yulug I, Merlano M, Numico G, Comino A, Attard M, Reelfs O, Gusterson B, Bell AK, Heath V, Tavassoli M, Farrell PJ, Smith P, Lu X, Crook T (2003) p53 polymorphism influences response in cancer chemotherapy via modulation of p73-dependent apoptosis. Cancer Cell 3: 387–402
Bertheau P, Turpin E, Rickman DS, Espié M, de Reyniès A, Feugeas JP, Plassa LF, Soliman H, Varna M, de Roquancourt A, Lehmann-Che J, Beuzard Y, Marty M, Misset JL, Janin A, de Thé H (2007) Exquisite sensitivity of TP53 mutant and basal breast cancers to a dose-dense epirubicin-cyclophosphamide regimen. PLoS Med 4: e90
Bond GL, Hu W, Bond EE, Robins H, Lutzker SG, Arva NC, Bargonetti J, Bartel F, Taubert H, Wuerl P, Onel K, Yip L, Hwang SJ, Strong LC, Lozano G, Levine AJ (2004) A single nucleotide polymorphism in the MDM2 promoter attenuates the p53 tumor suppressor pathway and accelerates tumor formation in humans. Cell 119: 591–602
Bond GL, Levine AJ (2007) A single nucleotide polymorphism in the p53 pathway interacts with gender, environmental stresses and tumor genetics to influence cancer in humans. Oncogene 26: 1317–1323
Brown JM, Wouters BG (1999) Apoptosis, p53, and tumor cell sensitivity to anticancer agents. Cancer Res 59: 1391–1399
Cimoli G, Malacarne D, Ponassi R, Valenti M, Alberti S, Parodi S (2004) Meta-analysis of the role of p53 status in isogenic systems tested for sensitivity to cytotoxic antineoplastic drugs. Biochim Biophys Acta 1705: 103–120
Dumont P, Leu JI, Della Pietra AC, George DL, Murphy M (2003) The codon 72 polymorphic variants of p53 have markedly different apoptotic potential. Nat Genet 33: 357–365
Flaman JM, Frebourg T, Moreau V, Charbonnier F, Martin C, Chappuis P, Sappino AP, Limacher IM, Bron L, Benhattar J, Tada M, Van Meir EG, Estreicher A, Iggo RD (1995) A simple p53 functional assay for blood and tumors. Proc Natl Acad Sci USA 92: 3963–3967
Gasco M, Crook T (2003) p53 family members and chemoresistance in cancer: what we know and what we need to know. Drug Resist Updat 6: 323–328
Gryshchenko I, Hofbauer S, Stoecher M, Daniel PT, Steurer M, Gaiger A, Eigenberger K, Greil R, Tinhofer I (2008) MDM2 SNP309 is associated with poor outcome in B-cell chronic lymphocytic leukemia. J Clin Oncol 26: 2252–2257
Hu Z, Jin G, Wang L, Chen F, Wang X, Shen H (2007) MDM2 promoter polymorphism SNP309 contributes to tumor susceptibility: evidence from 21 case-control studies. Cancer Epidemiol Biomarkers Prev 16: 2717–2723
Huang RS, Duan S, Bleibel WK, Kistner EO, Zhang W, Clark TA, Chen TX, Schweitzer AC, Blume JE, Cox NJ, Dolan ME (2007a) A genome-wide approach to identify genetic variants that contribute to etoposide-induced cytotoxicity. Proc Natl Acad Sci USA 104: 9758–9763
Huang RS, Duan S, Shukla SJ, Kistner EO, Clark TA, Chen TX, Schweitzer AC, Blume JE, Dolan ME (2007b) Identification of genetic variants contributing to cisplatin-induced cytotoxicity by use of a genomewide approach. Am J Hum Genet 81: 427–437
Huang RS, Duan S, Kistner EO, Bleibel WK, Delaney SM, Fackenthal DL, Das S, Dolan ME (2008) Genetic variants contributing to daunorubicin-induced cytotoxicity. Cancer Res 68: 3161–3168
Ikediobi ON, Davies H, Bignell G, Edkins S, Stevens C, O′Meara S, Santarius T, Avis T, Barthorpe S, Brackenbury L, Buck G, Butler A, Clements J, Cole J, Dicks E, Forbes S, Gray K, Halliday K, Harrison R, Hills K, Hinton J, Hunter C, Jenkinson A, Jones D, Kosmidou V, Lugg R, Menzies A, Mironenko T, Parker A, Perry J, Raine K, Richardson D, Shepherd R, Small A, Smith R, Solomon H, Stephens P, Teague J, Tofts C, Varian J, Webb T, West S, Widaa S, Yates A, Reinhold W, Weinstein JN, Stratton MR, Futreal PA, Wooster R (2006) Mutation analysis of 24 known cancer genes in the NCI-60 cell line set. Mol Cancer Ther 5: 2606–2612
Kanno J, Aisaki K, Igarashi K, Nakatsu N, Ono A, Kodama Y, Nagao T (2006) ‘Per cell’ normalization method for mRNA measurement by quantitative PCR and microarrays. BMC Genomics 7: 64
Le Morvan V, Bellott R, Moisan F, Mathoulin-Pélissier S, Bonnet J, Robert J (2006) Relationships between genetic polymorphisms and anticancer drug cytotoxicity vis-à-vis the NCI-60 panel. Pharmacogenomics 7: 843–852
Lee JM, Abrahamson JL, Bernstein A (1994) DNA damage, oncogenesis and the p53 tumour-suppressor gene. Mutat Res 307: 573–581
Lowe SW, Bodis S, McClatchey A, Remington L, Ruley HE, Fisher DE, Housman DE, Jacks T (1994) p53 status and the efficacy of cancer therapy in vivo. Science 266: 807–810
Moisan F, Longy M, Robert J, Le Morvan V (2006) Identification of gene polymorphisms of human DNA topoisomerase I in the National Cancer Institute panel of human tumour cell lines. Br J Cancer 95: 906–913
Monks A, Scudiero D, Skehan P, Shoemaker R, Paull K, Vistica D, Hose C, Langley J, Cronise P, Vaigro-Wolff A, Gray-Goodrich M, Campbell H, Mayo J, Boyd M (1991) Feasibility of a high flux anticancer drug screen using a diverse panel of cultured human tumor cell lines. J Natl Cancer Inst 83: 757–766
Nakatsu N, Yoshida Y, Yamazaki K, Nakamura T, Dan S, Fukui Y, Yamori T (2005) Chemosensitivity profile of cancer cell lines and identification of genes determining chemosensitivity by an integrated bioinformatical approach using cDNA arrays. Mol Cancer Ther 4: 399–412
Nayak MS, Yang JM, Hait WN (2007) Effect of a single nucleotide polymorphism in the murine double minute 2 promoter (SNP309) on the sensitivity to topoisomerase II-targeting drugs. Cancer Res 67: 5831–5839
Nief N, Le Morvan V, Robert J (2007) Involvement of gene polymorphisms of thymidylate synthase in gene expression, protein activity and anticancer drug cytotoxicity using the NCI-60 panel. Eur J Cancer 43: 955–962
O’Connor PM, Jackman J, Bae I, Myers TG, Fan S, Mutoh M, Scudiero DA, Monks A, Sausville EA, Weinstein JN, Friend S, Fornace Jr AJ, Kohn KW (1997) Characterization of the p53 tumor suppressor pathway in cell lines of the National Cancer Institute anticancer drug screen and correlations with the growth-inhibitory potency of 123 anticancer agents. Cancer Res 57: 4285–4300
Scherf U, Ross DT, Waltham M, Smith LH, Lee JK, Tanabe L, Kohn KW, Reinhold WC, Myers TG, Andrews DT, Scudiero DA, Eisen MB, Sausville EA, Pommier Y, Botstein D, Brown PO, Weinstein JN (2000) A gene expression database for the molecular pharmacology of cancer. Nat Genet 24: 236–244
Stähler F, Roemer K (1998) Mutant p53 can provoke apoptosis in p53-deficient Hep3B cells with delayed kinetics relative to wild-type p53. Oncogene 17: 3507–3512
Sullivan A, Syed N, Gasco M, Bergamaschi D, Trigiante G, Attard M, Hiller L, Farrell PJ, Smith P, Lu X, Crook T (2004) Polymorphism in wild-type p53 modulates response to chemotherapy in vitro and in vivo. Oncogene 23: 3328–3337
Vogelstein B, Lane D, Levine AJ (2000) Surfing the p53 network. Nature 408: 307–310
Wegman P, Stal O, Askmalm MS, Nordenskjöld B, Rutqvist LE, Wingren S (2006) p53 polymorphic variants at codon 72 and the outcome of therapy in randomized breast cancer patients. Pharmacogenet Genomics 16: 347–351
Yarosh DB, Peña A, Brown DA (2005) DNA repair gene polymorphisms affect cytotoxicity in the National Cancer Institute Human Tumour Cell Line Screening Panel. Biomarkers 10: 188–202
Acknowledgements
Part of this work was performed as the Master's research project of NF and LA at the Université de Bordeaux 2. We acknowledge the grants from the Ligue Nationale contre le cancer, committees of Charente and Charente-Maritime. We are grateful to Dr S Holbeck from the National Cancer Institute, Bethesda, MD, USA, for making available the NCI-60 panel for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Faur, N., Araud, L., Laroche-Clary, A. et al. The association between the T309G polymorphism of the MDM2 gene and sensitivity to anticancer drug is dependent on the p53 mutational status in cellular models. Br J Cancer 101, 350–356 (2009). https://doi.org/10.1038/sj.bjc.6605096
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6605096
Keywords
This article is cited by
-
Identification of SNPs associated with response of breast cancer patients to neoadjuvant chemotherapy in the EORTC-10994 randomized phase III trial
The Pharmacogenomics Journal (2015)
-
Genetic association of single nucleotide polymorphisms in P53 pathway with gastric cancer risk in a Chinese Han population
Medical Oncology (2015)
-
Association of the germline TP53 R72P and MDM2 SNP309 variants with breast cancer survival in specific breast tumor subgroups
Breast Cancer Research and Treatment (2011)