Abstract
The risk of prostate cancer is known to be elevated in carriers of germline mutations in BRCA2, and possibly also in carriers of BRCA1 and CHEK2 mutations. These genes are components of the ATM-dependent DNA damage signalling pathways. To evaluate the hypothesis that variants in ATM itself might be associated with prostate cancer risk, we genotyped five ATM variants in DNA from 637 prostate cancer patients and 445 controls with no family history of cancer. No significant differences in the frequency of the variant alleles at 5557G>A (D1853N), 5558A>T (D1853V), ivs38-8t>c and ivs38-15g>c were found between the cases and controls. The 3161G (P1054R) variant allele was, however, significantly associated with an increased risk of developing prostate cancer (any G vs CC OR 2.13, 95% CI 1.17–3.87, P=0.016). A lymphoblastoid cell line carrying both the 3161G and the 2572C (858L) variant in the homozygote state shows a cell cycle progression profile after exposure to ionising radiation that is significantly different to that seen in cell lines carrying a wild-type ATM gene. These results provide evidence that the presence of common variants in the ATM gene, may confer an altered cellular phenotype, and that the ATM 3161C>G variant might be associated with prostate cancer risk.
Similar content being viewed by others
Main
Prostate cancer is the second most common malignancy and the second commonest cause of cancer deaths in men in the European Union, with 143 000 new cases and 60 000 deaths year−1 (GLOBCAN 2000, www-dep.iarc.fr). The aetiology of prostate cancer is poorly understood. Prostate cancer is known to aggregate in families, indicating that genetic susceptibility may be important, but the genes involved are largely unknown. Linkage studies in multiple case families have suggested susceptibility loci on chromosomes 1q24, 1q42, 1p36, 8p22–23, 17p, 20q13 and Xq (see recent reviews by DeMarzo et al, 2003; Gronberg, 2003) but none have been definitively replicated. As a consequence of these linkage studies, variants in prostate cancer families have been identified in several genes including Macrophage Scavenger Receptor 1(MSR1), 2′-5′-oligoadenylate-dependent ribonuclease L (RNASEL) and ELAC2 (chromosome 17p11/HPC2 region) (reviewed in Simard et al, 2003), but again none have been reliably associated with risk.
Several independent studies have demonstrated that individuals with germline mutations in BRCA2 are at increased risk of prostate cancer (The Breast Cancer Linkage Consortium, 1999; Edwards et al, 2003; Giusti et al, 2003). There is also some evidence for an increased risk in carriers of BRCA1 mutations (Thompson et al, 2002). More recently, Seppala et al (2003) have found that the CHEK2 variant 1100delC, known to be associated with an increased risk of breast cancer, is also associated with an increased risk of prostate cancer, and Dong et al (2003) found that this and other missense variants in CHEK2 occurred at increased frequency in prostate cancer cases. The proteins encoded by the BRCA1 and BRCA2 genes participate in the maintenance of genomic stability through their involvement in the homologous recombination pathway for the repair of DNA double-strand breaks and transcription coupled repair and the CHEK2 protein is also involved in DNA damage signalling pathways. BRCA1 and CHEK2 are both phosphorylated in response to DNA damage in an ATM-dependent fashion (Matsuoka et al, 2000). Thus, we hypothesised that the ATM gene, whose protein functions upstream of these known susceptibility genes, could also be a mutation target in prostate cancer.
In a preliminary study by Hall et al (1998), germline mutations in ATM were identified in three out of 17 (17.6%) prostate cancer patients who showed a severe late response to radiation therapy and in whom most or all of the ATM gene was examined, while no such mutations were found in the control group. In this same study, the 5557G>A ATM sequence variant was found in 35% of cases compared with the reported population frequency of 15%. This variant has been found to modulate the penetrance of hereditary nonpolyposis colorectal cancer in carriers of germline MLH1 and MLH2 mutations (Maillet et al, 2000). Loss of heterozygosity of chromosome 11q, the location of the ATM gene, has also been reported in metastatic prostate carcinoma (Ruijter et al, 1999).
In order to assess whether ATM variants play a pathogenic role in prostate cancer development, we compared the frequencies of five ATM single-nucleotide polymorphisms (SNPs) 5557G>A, 5558A>T, 3161C>G, ivs38-8t>c, ivs38-15g>c in 618 British prostate cancer cases and 445 controls. In addition, the cellular phenotype of a lymphoblastoid cell line carrying the 3161G variant allele in a homozygote state was evaluated.
Materials and methods
Subjects
Subjects were obtained from a study of prostate cancer cases treated at the Royal Marsden NHS Trust over the period 1993–2002, as previously described (Eeles et al, 1999). The patients were unselected for age or family history. The current study included 637 Caucasian cases diagnosed between ages 43 and 86 years.
Controls
Controls were recruited from two series. Series one comprised of spouses of patients enrolled in a population-based study of colorectal cancer in the UK (84 males, 86 females) Series 2 (n=275) were male controls from a different population-based case–control study of early-onset prostate cancer. These controls were chosen from the same general practitioners as controls in the case–control study, and were therefore recruited from across the UK. Controls had no personal history of cancer. Individuals whose ethnic group was recorded as non-white were excluded from both the case and control series.
Lymphoblastoid cell lines
A lymphoblastoid cell line (LCL) (HA220) was established by infection with Epstein–Barr virus from a breast cancer patient carrying the ATM 3161G variant in the homozygous state. This individual carried none of the other SNPs investigated in this present study; however, the 2572T>C variant, which is in strong linkage disequilibrium with 3161C>G, was also present. LCLs from a subject with a wild-type ATM gene (IARC 1104) and a classical AT patient carrying truncating mutations on both alleles (IARC AT11 Q2002X; Q2714X) were used for comparative purposes in this study. These two lines were obtained from Dr G Lenoir. The cells were routinely maintained at 37°C in 5% CO2 in RPMI 1640 Glutamax-1 medium (Gibco, Invitrogen Corporation, Cergy-Pontoise, France) containing 10% heat-inactivated foetal calf serum (Integro b.v.i, Zaandan, Holland) and 1% penicillin/streptomycin (Biochrom AG, Berlin, Germany).
Cell cycle distribution by flow cytometry
Two flasks were set-up containing 20 ml of stock cultures (5 × 105 cells ml−1). One flask served as an unirradiated control and the second was treated with 5 Gy of ionising radiation from a Cs137 source. A volume of 4 ml was harvested immediately from each flask (time 0 h) and then 24 and 48 h postirradiation. The cells were centrifuged at 1100 r.p.m. for 5 min at 4°C, washed once in PBS and frozen at −80°C in citrate/sucrose/DMSO buffer (CycleTESTTM PLUS staining kit Becton Dickinson, Franklin Lakes, NJ, USA) until being evaluated. Just before analysis, the cells were resuspended in a trypsin solution for 10 min at room temperature, followed by the addition of RNAse buffer (10 min at room temperature) and stained with a solution of propidium iodide. The samples were subsequently analysed with a FACS Calibur flow cytometer (Becton Dickinson). The ModFit LT cell cycle analysis software was used to estimate percentage of cells in the G0–G1, S and G2–M phases. At least three independent experiments were done for each cell line and the G2/G1 ratios were calculated.
DNA extraction
DNA was extracted from blood samples by routine methods with the inclusion of a second proteinase K digestion at 50°C (Edwards et al, 1997). DNA was dissolved in 0.2–0.4 ml of water (BDH, Poole, UK) and stored at −20°C until required.
ATM SNP analysis
The frequency of the ATM SNPs was assessed using either high-performance liquid chromatography (DHPLC) or restriction fragment length polymorphism (RFLP) after polymerase chain reaction (PCR) amplification of the appropriate ATM fragment. For DHPLC analysis, PCRs of 40 μl were performed in 96-well plates to amplify two regions using the primers listed in Table 1. Each PCR contained 25 ng DNA, 200 μ M each dNTP, 3 mM MgCl2, 0.4 μ M primer and 1.5 U Platinum Taq polymerase (InVitrogen SARL, Cergy Pontoise, France). The cycling conditions were 94°C 5 min, followed by 35 cycles of 94°C 30 s, 52°C (exon 24) or 57°C (exon 39) 30 s, 72°C 30 s, with a final extension at 72°C for 5 min. The PCR products were denatured for 5 min at 95°C and then slowly cooled to permit reannealing and formation of homoduplexes and heteroduplexes.
DHPLC analysis of exon 24 (containing the 3161C>G variant) and exon 39 (containing the 5557G>A, 5558A>T, ivs38-8t>c and ivs38-15g>c variants) was performed on a WAVE DNA Fragment Analysis System (Transgenomic, Omaha, NE, USA). Buffer gradient and temperature conditions were calculated using the WAVEmaker software (version 3.4.4. Transgenomic). In order to establish whether the homoduplexes contained a wild-type or variant sequence, a second DHPLC analysis was carried out mixing these samples with a DNA sample containing a wild-type sequence. For all samples displaying aberrant DHPLC chromatograms, the PCR was repeated and the sequences of these PCR products determined using an ABI 3100 Genetic Analyser. The primers used for sequencing were the forward and reverse PCR primers in Table 1.
The frequency of the 3161C>G SNP was assessed in the DNAs of all the controls and 226 of the cases using restriction endonuclease digestion making use of the fact that this SNP occurs at a naturally occurring AlwI site (Table 1). The PCRs were carried out in a total volume of 25 μl containing 25 ng DNA, 100 μ M each dNTP, 2 mM MgCl2, 0.4 μ M primer and 1.5 U Platinum Taq polymerase (InVitrogen SARL, Cergy Pontoise, France). The cycling conditions were 94°C 5 min, followed by 40 cycles of 94°C 30 s, 59°C 30 s, 72°C 30 s, with a final extension at 72°C for 5 min. The PCR product was digested with AlwI according to the manufacturer's instructions and the fragments analysed by electrophoresis on a 3% NuSieve agarose gel. DNA samples known to be carrying the mutant allele were included in each analysis, with the genotype of the samples being determined by the banding pattern observed on the gels (the 494 bp PCR product being cut into 305 and 189 bp fragments if the wild-type allele is present). A random sample of DNAs was also analysed by direct sequencing of the corresponding exon and complete concordance between the different techniques was observed (data not presented).
Statistical methods
Analyses of genotype frequencies for each polymorphism were based on all cases and controls successfully typed for each polymorphism. Departures from Hardy–Weinberg equilibrium were assessed by comparing the observed and expected genotype frequencies. Differences in genotype frequencies between cases and controls were tested using standard χ2-tests. Odds ratios (OR) and confidence limits (CI) were calculated by standard methods. For the 5557G>A polymorphism where there was more than two genotypes, 95% floating confidence limits (FCIs) were also computed as suggested by Easton et al (1991). An ANOVA analysis was used to compare the G2/G1 ratios between the control, AT and HA220 cell lines and a t-test to compare the results obtained for HA220 and the group of six control cell lines. All computations were calculated using STATA version 7.0 (Stata Corporation).
Results
The genotype frequencies for the five SNPs in cases and controls, with corresponding ORs, are shown in Table 2. The maximum number of cases and controls for whom a genotype was available was 628 and 445, respectively. The frequencies of the variant alleles 5557A, 5558T and 3161G are in good agreement with previous studies in the Caucasian population (Dork et al, 2001; Spurdle et al, 2002; Mauget-Faysse et al, 2003). The frequency of the intronic SNPs ivs38-15g>c (Thorstenson et al, 2001) and ivs38-8t>c (Sandoval et al, 1999) have previously only been determined in a small number of individuals. The ivs38-15 is the rarer of the two variants, the c allele being present at an allele frequency of 0.004, while the ivs38-8c allele is found at a frequency of 0.036. In agreement with previous observations, the ivs38-8t>c variant was in strong linkage disequilibrium with the G5557A variant. The allele frequency did not differ significantly between the two series of controls, or between male and female controls, for any of the SNPs examined. We therefore combined our control series for the main analysis.
We found no significant differences in the genotype distribution between cases and controls for the SNPs 5557, 5558, ivs38-8 and ivs38-15. The 3161G allele was, however, associated with an increased risk of developing prostate cancer (any G vs CC OR 2.13, 95% CI 1.17–3.87; P=0.016) (Table 2).
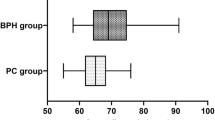
A lymphoblastoid cell line carrying both the 3161G variant in the homozygote state and the 2572T>C variant in exon 19 (F858L), which are in strong linkage disequilibrium, was available. The line originated from a German breast cancer patient who was diagnosed at age 38 and suffered from a local relapse by age 40. Her father died from prostate cancer, but she had no family history of breast cancer. ATM protein was found to be expressed at wild-type levels in the line HA220 as revealed by immunoblotting (data not shown). The cell cycle profile after exposure to 5 Gy was determined in this lymphoblastoid line (HA220) in comparison with a LCL carrying a wild-type or a mutant ATM gene. At zero time (T0 h Figure 1) there was no differences in the proportion of cells in the different phases of the cell cycle and thus in the G2/G1 ratios between HA220, the control and AT cell lines. After exposure to 5 Gy of ionising radiation the G2/G1 ratio, representative of the percentage of cells which accumulate in G2, is significantly higher in the AT line, IARC AT11, than the control line, IARC 1104 at both 24 h (P=0.001) and 48 h (P=0.000014). The ANOVA analysis of the observed cellular response, adjusted for time, for HA220 shows that it is intermediate between that seen in these two cell types. The G2/G1 ratio was significantly higher than that seen in the control cell line after exposure (G2/G1 HA220 vs IARC 1104 P=0.033) yet lower than that seen in the AT line (G2/G1HA220 vs IARC AT11 P=0.000005). When this profile is compared with the results obtained from the analysis of six cell lines carrying a wild-type ATM gene assayed under similar conditions (Angèle et al, 2003) the response in HA220 it is not statistically different 24 h after exposure to ionising radiation. However, at 48 h postirradiation there was significantly more cells in the G2 phase of the cell cycle than in the treated control cell lines (HA220 vs control cell lines 48.62±3.47 vs 41.22±4.63% P=0.0296 (t-test) full data set not shown).
Discussion
We have investigated the possible association between five ATM sequence variants and an increased risk of prostate cancer. Of the SNPs investigated, we found evidence for an association with prostate cancer only for the 3161C>G (1054P>R) variant. This association, while significant at the 0.016 level, is not definitive and will require further evaluation in other case–control studies. Conversely, modest associations with some of the other SNPs cannot be definitively excluded. This is particularly true of the 5558A>T and ivs38-15g>c variants, which are rare and for which the upper 95% CI on the OR exceeds 3.
Assuming that the association between 3161G variant allele and prostate cancer is not due to chance, there are essentially three possible explanations for the association: a difference in frequency between the populations from which the cases and controls were drawn (population stratification), linkage disequilibrium or a true causal association. Although population stratification remains a possibility, the similarity in frequency between the two control groups, and the fact that one of the control groups were chosen from the general practitioners of prostate cancer cases makes this less likely. To distinguish between a causal association and linkage disequilibrium, it would be necessary to evaluate all variants occurring on the same haplotype as 3161G. Strong linkage disequilibrium has been found between 3161G (P1054R) and the variant allele at 2572C (F858L). It has also been found to occur in cis to the splicing mutation 3576G to A found in some AT patients of South or South East European descent (Sandoval et al, 1999) although this splicing mutation was neither present in the patient HA220 nor in any other breast cancer patient carrying the 3161G allele (Dork et al, 2001). There may, however, be other variants on this haplotype (including noncoding alterations) that have not been studied.
The 3161G>C variant is located in the β-adaptin domain of the ATM protein and has been suggested to be linked to an increased cancer risk (Vorechovsky et al, 1996, 1999). It has been reported as a pathogenic mutation in a B-cell chronic lymphocytic leukaemia patient (Stankovic et al, 1999). Larson et al (1997/8) found that the variant genotype was present in 13.6% of breast cancers with an affected sister, compared with 3.5% of breast cancers without a family history and 3.2% of the controls. The results from subsequent breast cancer studies do not provide strong support for this association (Dork et al, 2001; Sommer et al, 2002; Spurdle et al, 2002). A combined analysis of these three studies, however, provides some suggestion of an association between 3161G and breast cancer risk (OR after stratification by study 1.34, 95% CI 0.99–1.83). Dork et al (2001) found a higher proportion of node-positive tumours was observed in P1054R heterozygous breast cancer patients (P<0.01) suggesting that this ATM variant could modulate the course or prognosis of breast carcinoma. Interestingly, the LCL established from a homozygous carrier of the 3161G allele shows a cell cycle progression profile with time after exposure to ionising radiation that is intermediate between that seen for LCLs carrying a wild-type or a mutant ATM gene. In addition, this line and five other LCLs established from breast cancer patients carrying the linked 2572T>C and 3161 C>G variants in the heterozygous state had higher levels of micronuclei induction after exposure to ionising radiation compared with LCLs with a wild-type ATM gene (Gutiérrez-Enríquez et al, 2004) suggesting that the presence of this variant may influence the cellular response after exposure to ionising radiation.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Angèle S, Lauge A, Fernet M, Moullan N, Beauvais P, Couturier J, Stoppa-Lyonnet D, Hall J (2003) Phenotypic cellular characterization of an ataxia telangiectasia patient carrying a causal homozygous missense mutation. Hum Mutat 21: 169–170
DeMarzo AM, Nelson WG, Isaacs WB, Epstein JI (2003) Pathological and molecular aspects of prostate cancer. Lancet 361: 955–964
Dong X, Wang L, Taniguchi K, Wang X, Cunningham JM, McDonnell SK, Qian C, Marks AF, Slager SL, Peterson BJ, Smith DI, Cheville JC, Blute ML, Jacobsen SJ, Schaid DJ, Tindall DJ, Thibodeau SN, Liu W (2003) Mutations in CHEK2 associated with prostate cancer risk. Am J Hum Genet 72: 270–280
Dork T, Bendix R, Bremer M, Rades D, Klopper K, Nicke M, Skawran B, Hector A, Yamini P, Steinmann D, Weise S, Stuhrmann M, Karstens JH (2001) Spectrum of ATM gene mutations in a hospital-based series of unselected breast cancer patients. Cancer Res 61: 7608–7615
Easton DF, Peto J, Babiker AG (1991) Floating absolute risk: an alternative to relative risk in survival and case–control analysis avoiding an arbitrary reference group. Stat Med 10: 1025–1035
Edwards S, Meitz J, Eles R, Evans C, Easton D, Hopper J, Giles G, Foulkes WD, Narod S, Simard J, Badzioch M, Mahle L (2003) International ACTANE Consortium. Results of a genome-wide linkage analysis in prostate cancer families ascertained through the ACTANE consortium. Prostate 57: 270–279
Edwards SM, Dearnaley DP, Ardern-Jones A, Hamoudi RA, Easton DF, Ford D, Shearer R, Dowe A, Eeles RA (1997) No germline mutations in the dimerization domain of MXI1 in prostate cancer clusters. The CRC/BPG UK Familial Prostate Cancer Study Collaborators. Cancer Research Campaign/British Prostate Group. Br J Cancer 76: 992–1000
Eeles RA, The UK Familial Prostate Study Co-ordinating Group & the CRC/BPG UK Familial Prostate Cancer Study (1999) Genetic predisposition to prostate cancer. Prostate Cancer Prostatic Diseases 2: 9–15
Giusti RM, Rutter JL, Duray PH, Freedman LS, Konichezky M, Fisher-Fischbein J, Greene MH, Maslansky B, Fischbein A, Gruber SB, Rennert G, Ronchetti RD, Hewitt SM, Struewing JP, Iscovich J. (2003) A twofold increase in BRCA mutation related prostate cancer among Ashkenazi Israelis is not associated with distinctive histopathology. J Med Genet 40: 787–792
Gronberg H (2003) Prostate cancer epidemiology. Lancet 361: 859–864
Gutiérrez-Enríquez S, Fernet M, Dörk T, Bremer M, Lauge A, Stoppa-Lyonnet D, Moulla N, Angèle S, Hall J (2004) Functional consequences of ATM sequence variants on chromosomal radiosensitivity. Genes, Chromosomes Cancer 40: 109–119
Hall EJ, Schiff PB, Hanks GE, Brenner DJ, Russo J, Chen J, Sawant SG, Pandita TK (1998) A preliminary report: frequency of A–T heterozygotes among prostate cancer patients with severe late responses to radiation therapy. Cancer J Sci Am 4: 385–389
Larson GP, Zhang G, Ding S, Foldenauer K, Udar N, Gatti RA, Neuberg D, Lunetta KL, Ruckdeschel JC, Longmate J, Flanagan S, Krontiris TG (1997/8) An allelic variant at the ATM locus is implicated in breast cancer susceptibility. Genet Testing 1: 165–170
Maillet P, Chappuis PO, Vaudan G, Dobbie Z, Muller H, Hutter P, Sappino AP (2000) A polymorphism in the ATM gene modulates the penetrance of hereditary non-polyposis colorectal cancer. Int J Cancer 88: 28–31
Matsuoka S, Rotman G, Ogawa A, Shiloh Y, Tamai K, Elledge SJ (2000) Ataxia telangiectasia-mutated phosphorylates Chk2 in vivo and in vitro. Proc Natl Acad Sci USA 97: 10389–10394
Mauget-Faysse M, Vuillaume M, Quaranta M, Moullan N, Angèle S, Friesen MD, Hall J (2003) Idiopathic and radiation-induced ocular telangiectasia: the involvement of the ATM gene. Invest Ophthalmol Vis Sci 44: 3257–3262
Ruijter ET, Miller GJ, van de Kaa CA, van Bokhoven A, Bussemakers MJ, Debruyne FM, Ruiter DJ, Schalken JA (1999) Molecular analysis of multifocal prostate cancer lesions. J Pathol 188: 271–277
Sandoval N, Platzer M, Rosenthal A, Dork T, Bendix R, Skawran B, Stuhrmann M, Wegner RD, Sperling K, Banin S, Shiloh Y, Baumer A, Bernthaler U, Sennefelder H, Brohm M, Weber BH, Schindler D (1999) Characterization of ATM gene mutations in 66 ataxia telangiectasia families. Hum Mol Genet 8: 69–79
Seppala EH, Ikonen T, Mononen N, Autio V, Rokman A, Matikainen MP, Tammela TL, Schleutker J (2003) CHEK2 variants associate with hereditary prostate cancer. Br J Cancer 89: 966–970
Simard J, Dumont M, Labuda D, Sinnett D, Meloche C, El-Alfy M, Berger L, Lees E, Labrie F, Tavtigian SV (2003) Prostate cancer susceptibility genes: lessons learned and challenges posed. Endocr Relat Cancer 10: 225–259
Sommer SS, Buzin CH, Jung M, Zheng J, Liu Q, Jeong SJ, Moulds J, Nguyen VQ, Feng J, Bennett WP, Dritschilo A (2002) Elevated frequency of ATM gene missense mutations in breast cancer relative to ethnically matched controls. Cancer Genet Cytogenet 134: 25–32
Spurdle AB, Hopper JL, Chen X, McCredie MR, Giles GG, Newman B, Chenevix-Trench G, Khanna K (2002) No evidence for association of ataxia-telangiectasia mutated gene T2119C and C3161G amino acid substitution variants with risk of breast cancer. Breast Cancer Res 4: R15
Stankovic T, Weber P, Stewart G, Bedenham T, Murray J, Byrd PJ, Moss PA, Taylor AM (1999) Inactivation of ataxia telangiectasia mutated gene in B-cell chronic lymphocytic leukaemia. Lancet 353: 26–29
The Breast Cancer Linkage Consortium (1999) Cancer risks in BRCA2 mutation carriers. J Natl Cancer Inst 91: 1310–1316
Thompson D, Easton DF, Breast Cancer Linkage Consortium. Cancer Incidence in BRCA1 mutation carriers (2002) J Natl Cancer Inst 94: 1358–1365
Thorstenson YR, Shen P, Tusher VG, Wayne TL, Davis RW, Chu G, Oefner PJ (2001) Global analysis of ATM polymorphism reveals significant functional constraint. Am J Hum Genet 69: 396–412
Vorechovsky I, Luo L, Lindblom A, Negrini M, Webster AD, Croce CM, Hammarstrom L (1996) ATM mutations in cancer families. Cancer Res 56: 4130–4183
Vorechovsky I, Luo L, Ortmann E, Steinmann D, Dork T (1999) Lancet 353: 127
Acknowledgements
The financial support of the AICR to Janet Hall is gratefully acknowledged. We gratefully acknowledge the contributions of Karin Klöpper, Elisabeth Ortmann, Diana Steinmann, Regina Waltes and Johann H Karstens to the recruitment and mutation analysis of breast cancer patients. We thank Dr G Lenoir for access to certain cell lines. We are grateful to the Prostate Cancer Charitable Trust, Cancer Research UK, The Institute of Cancer Research UK and the Community Fund. DFE is a Principal Research Fellow of Cancer Research UK. Norman Moullan participated in this study while holding an IARC Special Training Award.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Angèle, S., Falconer, A., Edwards, S. et al. ATM polymorphisms as risk factors for prostate cancer development. Br J Cancer 91, 783–787 (2004). https://doi.org/10.1038/sj.bjc.6602007
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6602007
Keywords
This article is cited by
-
Germline mutations in prostate cancer: a systematic review of the evidence for personalized medicine
Prostate Cancer and Prostatic Diseases (2023)
-
An appraisal of genetic testing for prostate cancer susceptibility
npj Precision Oncology (2022)
-
Germline risk of clonal haematopoiesis
Nature Reviews Genetics (2021)
-
Association between ATM rs1801516 polymorphism and cancer susceptibility: a meta-analysis involving 12,879 cases and 18,054 controls
BMC Cancer (2018)
-
Managing Patient with Mutations in PALB2, CHEK2, or ATM
Current Breast Cancer Reports (2018)