Abstract
Frequent loss of heterozygosity of microsatellites markers on specific chromosomal region have been reported in various types of primary human cancer. The same loss of heterozygosity has also been identified in the matched plasma/serum DNA. Using 109 microsatellite markers representing 24 chromosomal arms, we have examined the loss of heterozygosity in 21 cases of hepatocellular carcinoma, six of cholangiocarcinoma, and 27 cases of chronic hepatitis or cirrhosis. All cases of the hepatocellular carcinoma showed deletion from two to 10 chromosomal arms, while deletion of chromosomes from two to eight regions was detected in five of six cholangiocarcinoma patients. One or more loss of heterozygosity in the paired serum DNA could be detected in 16 of 25 (76.2%) hepatocellular carcinoma patients. In contrast, no alterations in serum DNA test could be found in cholangiocarcinoma patients. Five of seven (71.4%) hepatocellular carcinoma patients with alpha-fetoprotein levels less than 20 ng ml−1 produced positive serum DNA test. The profiles of 19 microsatellite markers gave a 100% positive predictive value and an 80.8% negative predictive value for hepatocellular carcinoma. In conclusion, we have determined a profile of microsatellite markers appropriate for differential diagnosis of primary liver cancer. The discovery may permit a high-throughput screening of hepatocellular carcinoma at an early stage of disease.
Similar content being viewed by others
Main
Primary liver cancer ranks fifth in frequency among all malignancies in the world with an estimated number of 437 000 new cases in 1990. The vast majority of primary liver cancer is hepatocellular carcinoma (HCC), a malignant tumour derived from hepatocytes. HCC is increasing in many countries, particularly in areas where hepatitis C virus infection is more common than hepatitis B virus infection (El-Serag and Mason, 1999). The cholangiocarcinoma (CC), an intrahepatic malignant tumour which arises in the epithelium of the bile ducts, is the second common hepatic tumour. Its occurrence is largely high in areas where liver fluke infestation or intrahepatic stones is endemic, such as Hong Kong, Thailand and Taiwan (Okuda et al, 1977).
The prognosis of HCC or CC is usually poor, with 3-year survival rates estimated at 44.9% and 34% after hepatic resection, respectively (Okuda et al, 1977). In patients with symptomatic HCC, the tumours are usually either too large and/or with local invasion or distant metastasis. Therefore, only 10–20% of patients could be treated with potentially curative therapy, while the remaining patients can only receive non-surgical therapy, such as a transcatheter arterial embolisation or other local ablation treatments with a less satisfactory outcome. The patients with CC often present with obstructive jaundice at the stage of advanced stage. Currently, resection offers the only chance of cure and the best chance of long-term survival.
In order to improve the chances of successful treatment and patient survival, great effort has been devoted to detect HCC in the early stage when it is ‘small’, for example smaller than 3 cm, and where liver function reserve is good enough for curative therapy. Measurement of serum α-fetoprotein (AFP) and hepatic ultrasonography are widely used as surveillance modalities for high-risk patients. Elevated levels of AFP, with normal range set at 20 ng ml−1, are detected in up to 75% of HCC patients, and values above 400 ng ml−1 are considered diagnostic for HCC (Ebara et al, 1986). However, 35% of HCC smaller than 3 cm may secrete little or no AFP into the circulation and thus will not be identified by this test (Ebara et al, 1986). As a result, measurement of AFP alone is not an ideal test for early diagnosis of HCC.
Recent advances in tumour genetics reveal that the genesis and progression of tumours follow an accumulation of multiple genetic alterations, including inactivation of tumour suppressor genes and/or activation of proto-oncogenes. Frequent loss of heterozygosity (LOH) of microsatellites markers on specific chromosomal region have been reported in various types of human cancer. In addition, nucleic acid-based molecular techniques have successfully identified the same LOH in the paired plasma/serum DNA from patients with diverse types of epithelial cancer, such as lung (Chen et al, 1996; Sozzi et al, 1999, 2001), head and neck (Coulet et al, 2000; Nunes et al, 2001), colon (Hibi et al, 1998), breast (Chen et al, 1999; Silva et al, 1999), kidney (Goessl et al, 1998; Eisenberger et al, 1999). The results indicate that microsatellite DNA analysis may have potential as a non-invasive test for cancer diagnosis. In this pilot study, we have searched for the genetic alterations, using a total of 109 microsatellite markers representing 24 chromosomal regions, in the serum DNA of patients with primary liver cancer, i.e. HCC (n=21) and CC (n=6). The results suggest that microsatellite serum DNA analysis may be a valuable, non-invasive method for the early detection of primary liver cancer.
Materials and methods
Sample collection and DNA preparation
Primary tumour from 21 cases of HCC and six cases of CC were collected from the Department of Surgery, National Cheng Kung University Hospital, Tainan, Taiwan between September 1998 and March 2000 (Tables 1 and 2). The tumour tissue was obtained immediately after surgical resection and stored at −80°C, and then microdissected as described in detail previously (Eisenberger et al, 1999). We also enrolled 27 patients (age- and sex-matched) with a biopsy diagnosis of chronic hepatitis (n=20) or cirrhosis (n=7) as controls. Both peripheral blood lymphocytes and serum samples were obtained with written informed consent. Briefly, DNA was extracted from peripheral blood lymphocytes, tumour and matched serum samples by digestion with 1% SDS/proteinase K (BD Biosciences Clontech, CA, USA) overnight followed by phenol-chloroform extraction and ethanol precipitation. Each tumour was reviewed for histologic grading according to the Edmondson classification (1958). Clinical staging was determined according to the tumour-node-metastasis staging protocol of the American Joint Committee on Cancer (1997) with surveys of the clinical details, image studies, and pathologic data. The clinical characteristics, including AFP, hepatitis B surface antigen (HBsAg) and hepatitis C virus antibody (anti-HCV), were obtained from medical records.
Analysis for allelic loss
Microsatellite markers from selected chromosomal arms for PCR analysis were obtained from Research Genetics (Huntsville, AL, USA). The marker pairs selected for HCC (74 markers from 17 chromosomal arms) included 1p (D1S160, D1S163, D1S170, D1S186, MYCL), 3p (D3S1317), 4p (D4S394), 4q (D4S398, D4S395, D4S392, D4S422, FGA, FABP2, D4S427, D4S415, D4S1615, D4S1554, D4S1426, D4S1598, D4S620, D4S1566, D4S1545, D4S2920, D4S2943, D4S2954), 5q (D5S409), 6q (D6S264), 8p (D8S261, D8S277), 8q (D8S85, D8S200, D8S555, D8S283), 9p (D9S169, D9S1747, D9S104), 10q (D10S109), 11p (D11S554, D11S436, D11S1344, D11S932, D11S1324), 11q (D11S938, D11S29), 12p (D12S93), 13q (D13S171, D13S153, Rb1, D13S133, D13S227, D13S159, D13S166, D13S168), 14q (D14S72, D14S51), 16p (D16S419, D16S409, D16S3106, D16S498), 16q (D16S415, D16S408, D16S512, D16S289, D16S402, D16S516, D16S422, D16S413), and 17p (D17S520, D17S1176, TP53, D17S513, D17S578, D17S796, D17S849) based on previous reports (Yeh et al, 1996; Nagai et al, 1997; Piao et al, 1998; Fujii et al, 2000; Okabe et al, 2000; Yeh et al, 2001). The marker pairs selected for CC (35 markers from 16 chromosomal arms) included 2p (BAT-26), 3p (D3S3667, D3S1578, D3S3582, D3S3560, D3S1581, D3S3729, D3S1588, D3S3648), 4 (D4S415, D4S413), 5q (D5S323, D5S417), 6p (D6S263), 6q (D6S292), 7q (D7S495, D7S486), 9p (D9S747, D9S171), 11p (D11S907, D11S569), 14q (D14S1436), 16q (D16S3094, D16S511, D16S534, D16S520), 17 (D17S695), 18q (D18S67, D18S51, D18S535), 20 (D20S85), 21q (D21S1245, D21S1436, D21S1270), and Xp (DXS538) (Ding et al, 1993; Fujii et al, 2000). All of the tumours, irrespective of histopathology, were analysed for a total of 109 microsatellite markers (74 markers for HCC and 35 markers for CC) to confirm the specificity of chromosomal alterations as well as their presence in the serum as tumour markers.
Prior to amplification, one primer from each pair was end-labelled with [γ-32P]ATP (20 μCi; Amersham Pharmacia Biotech Inc., NJ, USA) and T4 kinase (New England Biolabs Inc., MA, USA) (Eisenberger et al, 1999). The amplification conditions for polymerase chain reaction (PCR) were 1 × buffer (GibcoBRL, NY, USA), 1.5 mM MgCl2, 0.6 mM dNTP, 5 pmol of each primer, 1.0 μl γ-32P-labelled primer, 4 μl DNA, and 0.1 μl of Taq DNA polymerase (GibcoBRL, NY, USA) in a total of 10 μl. PCR for each primer set was performed for 35 cycles consisting of denaturation at 95°C for 30 s, annealing at 50–60°C for 1 min, and extension at 70°C for 1 min (Perkin-Elmer Gene Amp PCR System 9600, Perkin-Elmer Corporation, MA, USA). The reaction products were separated on 7% urea- formamide-polyacrylamide gels (GibcoBRL, NY, USA) and exposed for 12–24 h. For informative tumours, LOH was scored if the tumour allele demonstrated a greater than 30% reduction in intensity compared to the corresponding normal control visually as previously described (Figure 1) (Eisenberger et al, 1999). Each LOH was confirmed by two independent experiments. Allelic loss was determined by observation of LOH at any informative marker mapped to the same chromosomal region. Then, LOH analysis was performed on matched serum samples.
Statistical analysis
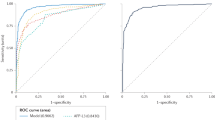
Allelic status was correlated with clinical and pathologic factors of HCC, such as histological grading, disease stage, tumour size, serum AFP levels, portal vein thrombosis and satellite nodule formation by Fisher's exact test. To evaluate the diagnostic accuracy in the microsatellite analysis, we considered four events: (A) positive test: presence of LOH in the primary tumour and in the matched serum DNA (true positive); (B) positive test: absence of LOH in tumour but presence of LOH in patient serum (false positive); (C) negative test: presence of LOH in tumour but absence in paired serum samples (false negative); and (D) negative test: absence of LOH either in tumour or in paired serum samples (true negative). Decision diagnostic criteria were obtained from the results A, B, C, and D. Test sensitivity is equal to A/A+C. Test specificity is equal to D/D+B. Test accuracy is equal to: A+D/A+B+C+D. Predictive positive result or positivity prediction is equal to A/A+B. Predictive negative result or negativity prediction is equal to D/D+C.
Results
All of the HCC cases showed deletion from two to 10 chromosomal arms (Table 1). The highest incidence was 16q (66.7%), followed by 1p (57.1%), 4q (57.1%), 8p (52.4%), 17p (52.4%), 13q (47.6%), 14q (42.9%), 9p (33.3%), 16p (33.3%), 3p (28.6%), 8q (28.6%), 5q (23.8%), 10q (14.3), 11p (9.5%), 18 (4.8%), and 7q (4.8%), respectively. The allelic losses were compared with biologic indicators of HCC, such as histological grading, tumour stage, size, and AFP serum levels (Table 1). A positive correlation was observed for 4q with AFP greater than 20 ng ml−1 (P=0.02), and 13q with satellite lesion (P=0.04) (data not shown). There was a trend toward positive association of 8p or 13q loss with advanced tumour staging (P=0.06), and 8p loss with AFP greater than 20 ng ml−1 (P=0.06). LOH on 14q and 16q occurred more frequently in hepatitis C virus-negative patients (P<0.05, respectively). Otherwise, patterns of allelic loss did not relate to histological grading or tumour size (P>0.1, respectively). In addition, novel alleles indicative of microsatellite instability were found in three patients (cases 2, 3 and 7, respectively) at chromosome 2, 13 and 16, respectively (data not shown).
As for tumour diagnosis, a total of 16 of 21 (76.2%) HCC patients were found to have LOH in serum DNA from one to four microsatellite markers (Table 1). The presence of LOH in the serum DNA did not relate to histological grading, staging or tumour size (P>0.1, respectively). If the cut-off values were set at AFP 400 ng ml−1, negative serum LOH test was observed in two of 10 (20%) patients with abnormal AFP level (cases 1 and 15), and in three of 11 (27.3%) patients having AFP level within normal limits (case 17, 18 and 20). In contrast, five of seven (71.4%) patients (cases 2, 3, 9, 10 and 21) having AFP less than 20 ng ml−1 had positive LOH test. The results imply that microsatellite DNA analysis may have potential as a non-invasive diagnostic test for the early detection of HCC, especially for those who having AFP below reference range. However, none of three cases showing microsatellite instability in primary tumours had the same alterations detected in the serum DNA (data not shown).
With regard to cholangiocarcinoma, five of six patients belong to advanced stage of tumour (Table 2). Deletion of chromosome was detected from two to eight regions in five of six patients. But, no any alterations in serum DNA test could be found, despite of the fact that some common allelic losses were observed between HCC and CC. The results seem to imply a limited potential of the microsatellite analysis in diagnosing of CC.
Altogether, the data of this pilot study indicate that microsatellite analysis of serum DNA could successfully detect around three-quarters (76.2%) of HCC by screening the following profile of microsatellite markers, i.e. D1S160, D1S163, D1S170, D4S1545, D5S409, D7S495, D8S200, D8S555, D9S171, D9S747, D11S1344, D13S227, D14S51, D16S289, D16S402, D16S419, D16S422, D16S498, D16S516. The positive predictive value was 100%, and negative predictive value was 80.8%.
Discussion
Currently, only ultrasound-guided needle biopsy yields diagnostic material and allows a definitive differential diagnosis between HCC and CC (Tsuji et al, 1999). Measurement of serum AFP and hepatic ultrasonography are widely used as surveillance modalities for patients with high-risk of liver cancer. In patients with HCC, however, around one-third of small tumour (<3 cm) was shown to secrete little or no AFP into the circulatory system (Ebara et al, 1986). As a result, it is mandatory to explore supplementary tumour marker for early detection of HCC.
In this study, we detected one or more LOH in the serum DNA in three-quarters of HCC patients. The results are comparable to some prior reports showing microsatellite alterations in the plasma/serum from cancer patients (Chen et al, 1996, 1999; Goessl et al, 1998; Hibi et al, 1998; Eisenberger et al, 1999; Silva et al, 1999; Sozzi et al, 1999, 2001; Coulet et al, 2000; Nunes et al, 2001). However, the sensitivity of microsatellite DNA test greatly depends on the kind of cancer studied. For example, the detection rate was 71% for small cell carcinoma of the lung (Chen et al, 1996), from 60 to 63% for renal cell carcinoma (Goessl et al, 1998; Eisenberger et al, 1999), between 48 and 66% for breast cancer (Chen et al, 1999; Silva et al, 1999), from 40 to 45% for non-small cell lung cancer (Sozzi et al, 1999, 2001), between less than 2 and 18.7% for head and neck cancer (Coulet et al, 2000; Nunes et al, 2001) using a set of primer pairs.
In contrast, the lack of tumour-specific LOH in the serum of CC patients appears to correspond to the observation reported for colon cancer (0%) (Hibi et al, 1998), though these patients may still have very low levels of tumour-derived DNA. Nonetheless, the difference appears to support the propensity of HCC to spread to vascular system (portal vein and hepatic vein), whereas perineural invasion and lymphatic involvement are frequently present in CC at an early stage (Sasaki et al, 2001). Taken together, the data support the detection of circulating tumour-derived DNA as a supplementary tumour marker in the differential diagnosis of primary liver cancer.
Of particular interest, LOH in the serum DNA could be detected in five of seven HCC patients with serum AFP less than 20 ng ml−1, the normal range for the healthy adults. Previous study found that approximately one third of small HCC (less than 3 cm) may secrete little or no AFP into the circulation (Ebara et al, 1986). Our data imply that the limitation of low specificity of AFP in diagnosing small HCC might be compensated by microsatellite analysis on cell-free DNA in cancer patients. It will be especially valuable in patients with poor liver function or ascites, in which further diagnostic investigation is prohibited. A prospective study is required to validate the importance of this molecular technique in the multimodality therapy for HCC.
We showed that the detection of HCC (71.4% sensitivity and 100% specificity) is feasible by screening the serum samples with a profile of 19 microsatellite markers. However, a recent study reported that around 50% of the cirrhotic nodules are monoclonal and already have chromosomal aberrations (Yeh et al, 2001). Whether the aberrations are also present in the serum DNA is currently unknown. Wang et al (2000) reported 87% of sensitivity in detection of p15/p16 methylation in the circulating DNA of HCC patients. Although the results seem to be better than we have in monitoring the profile of microsatellite markers, both the ability of differential diagnosis of HCC from CC and their value in patients having AFP below reference range were not examined. As a result, the impact of these observations in the development of HCC and/or cell type-specific genetic markers needs to be clarified in a large cohort of liver disease patients.
In conclusion, we have determined a profile of molecular markers appropriate for differential diagnosis of primary liver cancer in the serum. The discovery may permit a high-throughput screening of hepatocellular carcinoma at an early, and potentially resectable, stage of disease.
References
Chen XQ, Stroun M, Magnenat JL, Nicod LP, Kurt AM, Lyautey J, Lederrey C, Anker P (1996) Microsatellite alterations in plasma DNA of small cell lung cancer patients. Nat Med 2: 1033–1035
Chen X, Bonnefoi H, Diebold-Berger S, Lyautey J, Lederrey C, Faltin-Traub E, Stroun M, Anker P (1999) Detecting tumor-related alterations in plasma or serum DNA of patients diagnosed with breast cancer. Clin Cancer Res 5: 2297–2303
Coulet F, Blons H, Cabelguenne A, Lecomte T, Lacourreye O, Brasnu D, Beaune P, Zucman J, Laurent-Puig P (2000) Detection of plasma tumor DNA in head and neck squamous cell carcinoma by microsatellite typing and p53 mutation analysis. Cancer Res 60: 707–711
Ding SF, Delhanty JD, Bowles L, Dooley JS, Wood CB, Habib N (1993) A. Loss of constitutional heterozygosity on chromosomes 5 and 17 in cholangiocarcinoma. Br J Cancer 67: 1007–1010
Ebara M, Ohto M, Shinagawa T, Sugiura N, Kimura K, Matsutani S, Morita M, Saisho H, Tsuchiya Y, Okuda K (1986) Natural history of minute hepatocellular carcinoma smaller than three centimeters complicating cirrhosis. A study in 22 patients. Gastroenterology 90: 289–298
Eisenberger CF, Schoenberg M, Enger C, Hortopan S, Shah S, Chow NH, Marshall FF, Sidransky D (1999) Diagnosis of renal cancer by molecular urinalysis. J Natl Cancer Inst 91: 2028–2032
El-Serag HB, Mason AC (1999) Rising incidence of hepatocellular carcinoma in the United States. N Engl J Med 340: 745–750
Fujii H, Zhu XG, Matsumoto T, Inagaki M, Tokusashi Y, Miyokawa N, Fukusato T, Uekusa T, Takagaki T, Kadowaki N, Shirai T (2000) Genetic classification of combined hepatocellular-cholangiocarcinoma. Hum Pathol 31: 1011–1017
Goessl C, Heicappell R, Munker R, Anker P, Stroun M, Krause H, Muller M, Miller K (1998) Microsatellite analysis of plasma DNA from patients with clear cell renal carcinoma. Cancer Res 58: 4728–4732
Hibi K, Robinson CR, Booker S, Wu L, Hamilton SR, Sidransky D, Jen J (1998) Molecular detection of genetic alterations in the serum of colorectal cancer patients. Cancer Res 58: 1405–1407
Nagai H, Pineau P, Tiollais P, Buendia MA, Dejean A (1997) Comprehensive allelotyping of human hepatocellular carcinoma. Oncogene 14: 2927–2933
Nunes DN, Kowalski LP, Simpson AJ (2001) Circulating tumor-derived DNA may permit the early diagnosis of head and neck squamous cell carcinomas. Int J Cancer 92: 214–219
Okabe H, Ikai I, Matsuo K, Satoh S, Momoi H, Kamikawa T, Katsura N, Nishitai R, Takeyama O, Fukumoto M, Yamaoka Y (2000) Comprehensive allelotype study of hepatocellular carcinoma: potential differences in pathways to hepatocellular carcinoma between hepatitis B virus-positive and –negative tumors. Hepatology 31: 1073–1079
Okuda K, Kubo Y, Okazaki N, Arishima T, Hashimoto M (1977) Clinical aspects of intrahepatic bile duct carcinoma including hilar carcinoma: a study of 57 autopsy-proven cases. Cancer 39: 232–246
Piao Z, Park C, Park JH, Kim H (1998) Allelotype analysis of hepatocellular carcinoma. Int J Cancer 75: 29–33
Sasaki A, Kawano K, Aramaki M, Ohno T, Tahara K, Takeuchi Y, Yoshida T, Kitano S (2001) Clinicopathologic study of mixed hepatocellular and cholangiocellular carcinoma: modes of spreading and choice of surgical treatment by reference to macroscopic type. J Surg Oncol 76: 37–46
Silva JM, Dominguez G, Garcia JM, Gonzalez R, Villanueva MJ, Navarro F, Provencio M, San Martin S, Espana P, Bonilla F (1999) Presence of tumor DNA in plasma of breast cancer patients: clinicopathological correlations. Cancer Res 59: 3251–3256
Sozzi G, Musso K, Ratcliffe C, Goldstraw P, Pierotti MA, Pastorino U (1999) Detection of microsatellite alterations in plasma DNA of non-small cell lung cancer patients: a prospect for early diagnosis. Clin Cancer Res 5: 2689–2692
Sozzi G, Conte D, Mariani L, Lo Vullo S, Roz L, Lombardo C, Pierotti MA, Tavecchio L (2001) Analysis of circulating tumor DNA in plasma at diagnosis and during follow-up of lung cancer patients. Cancer Res 61: 4675–4678
Tsuji M, Kashihara T, Terada N, Mori H (1999) An immunohistochemical study of hepatic atypical adenomatous hyperplasia, hepatocellular carcinoma, and cholangiocarcinoma with alpha-fetoprotein, carcinoembryonic antigen, CA19-9, epithelial membrane antigen, and cytokeratins 18 and 19. Pathol Int 49: 310–317
Wang HN, Lo YM, Yeo W, Lau WY, Johnson PJ (2000) Frequent p15 promoter methylation in tumor and peripheral blood from hepatocellular carcinoma patients. Clin Cancer Res 6: 3516–3521
Yeh SH, Chen PJ, Lai MY, Chen DS (1996) Allelic loss on chromosomes 4q and 16q in hepatocellular carcinoma: association with elevated alpha-fetoprotein production. Gastroenterology 110: 184–192
Yeh SH, Chen PJ, Shau WY, Chen YW, Lee PH, Chen JT, Chen DS (2001) Chromosomal allelic imbalance evolving from liver cirrhosis to hepatocellular carcinoma. Gastroenterology 121: 699–709
Acknowledgements
This study was supported by research grant NSC 89-2314-B-006-027 from the National Science Council, and research grant NCKUH 89-051 from the National Cheng Kung University Hospital, Taiwan, Republic of China.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Chang, YC., Ho, CL., Chen, HW. et al. Molecular diagnosis of primary liver cancer by microsatellite DNA analysis in the serum. Br J Cancer 87, 1449–1453 (2002). https://doi.org/10.1038/sj.bjc.6600649
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6600649
Keywords
This article is cited by
-
Circulating tumor DNA in hepatocellular carcinoma: trends and challenges
Cell & Bioscience (2016)
-
The prognostic value of circulating plasma DNA level and its allelic imbalance on chromosome 8p in patients with hepatocellular carcinoma
Journal of Cancer Research and Clinical Oncology (2006)
-
Allelic loss of 14q32 in the pathogenesis of gastrointestinal and ampullary malignancies: mapping of the target region to a 17�cM interval
Journal of Cancer Research and Clinical Oncology (2005)