Abstract
Data sources
Medline, EMbase and Cochrane databases
Study selection
Studies were included if they reported data on patients with a histologically-confirmed diagnosis of oral dysplasia. They also had to study at least one outcome measure and one intervention method or clinical risk factor. Outcome measures included malignant transformation rate (MTR) and time to malignant transformation (TMT). In studies on oral lesions, which contained a defined subset of patients with oral dysplasia, this subset but not all patients with oral lesions were included in the meta-analysis. Observational studies were included in the review due to the scarcity of randomised controlled trials with adequate follow-up period.
Data extraction and synthesis
Quality assessment was undertaken independently by two reviewers. When there was disagreement, a third reviewer was consulted. Quality criteria were agreed upon a priori, and the authors used a combination of quality assessment methods. Eligibility of studies was determined independently from the abstracts by two reviewers blinded to each other's selections. Outcome data were abstracted independently by a researcher and a statistician and checked by a third reviewer. Heterogeneity was assessed graphically in a forest plot and a meta-analysis was conducted. Subgroup analysis was performed by histologic grade, clinical risk factors and treatment modality.
Results
Fourteen non-randomised studies, reporting on 992 patients, were included. There was considerable heterogeneity between studies. The mean overall MTR was 12.1% (95% CI: 8.1%, 17.9%) and the mean TMT was 4.3 years. Histologic grade significantly affected mean MTR (p < 0.008). Furthermore, lesions that were not excised demonstrated considerably higher MTR than those that were excised (p = 0.003)
Conclusions
Oral dysplasia showed a significant rate of transformation to cancer, which was related to grade, and was decreased significantly but not eliminated by excision. Findings suggest the need for surgical excision and continued surveillance, particularly in high-grade lesions.
Similar content being viewed by others
Commentary
Oral dysplasia is detected by clinicians in the form of leukoplakia, a white patch in the oral cavity that cannot be diagnosed as any other known disorder. These lesions carry an increased risk of malignant progression to oral squamous cell carcinoma. The early diagnosis, treatment and surveillance of these precancerous lesions are important predictors in preventing progression to oral cancer; therefore, this meta-analysis is very relevant.
The aim of this work was to inform an evidence-based management and surveillance policy for oral dysplastic lesions. The authors assessed the risk of and interval to progression to cancer in patients diagnosed with oral dysplasia. This is an area of clinical practice that demonstrates variability and lacks high-quality evidence.
The review had rigorous inclusion and exclusion criteria. 14 prospective and retrospective studies were identified. Data were subcategorised by histologic grade of the lesion and management strategy. The relative risks of malignant transformation for gender, lesion site, continuation of smoking and alcohol consumption after diagnosis were also extracted, where available.
Results showed that oral dysplasia carries a significant rate of transformation to cancer (12.1%). Furthermore, surgical excision decreased the risk of transformation by more than half, but did not eliminate it. Subgroup analysis by dysplasia grade and treatment modality showed no significant differences in TMT. This may be due to the limited availability of data.
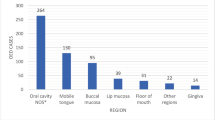
There was insufficient information in included studies to assess the effect of clinical risk factors on progression to malignancy. Nonetheless, malignant progression seemed to be associated with lesions of the tongue (relative risk =1.87; CI: 1.11, 3.17). The review showed that continuous smoking and alcohol use after diagnosis did not have any effect on malignant transformation. It is likely that this finding is due to the limited number of studies containing information on smoking and alcohol use and the reported heterogeneity between the two studies with data on smoking. Moreover, although oral dysplasia is uncommon in non-users of tobacco and alcohol, a study by Jaber1 found that oral dysplasia may develop in persons who have never used tobacco or alcohol, suggesting that risk factors other than alcohol and tobacco may exist.
The work also found that sex is a risk factor for oral dysplasia with women having a higher risk than men. Although this finding lacked statistical significance, it is in line with findings from other studies.1, 2 Lan and colleagues2 reported that risk of mild-moderate and severe dysplasia was 2.40 and 3.11 times higher, respectively, in women than men. They also reported that the malignant transformation of oral leukoplakia is correlated to clinical type and symptoms. As such, the risk of severe dysplasia and oral cancer of speckled leukoplakia (4.50 times), ulcerative (5.63 times), verrucous leukoplakia (4.09 times) were much higher than that of homogeneous leukoplakia. Furthermore, the risk of severe dysplasia and oral cancer in leukoplakia with symptoms was 4.38 times as high as without symptoms.2
The results of this meta-analysis should be interpreted with caution due to the small number of studies included, their limited quality and heterogeneity in terms of design, inclusion criteria, patient population, treatment, length of follow-up and analysis of patient risk factors. In addition, the systematic review showed a distinct lack of randomised controlled trials examining different surgical management and follow-up protocols. The meta-analysis used published data rather than original patient data, as many of the studies were conducted in the 1970s and 1980s. Due to these limitations, the work was unable to ascertain that higher grade dysplastic lesions transform earlier. Moreover, the limitations impeded the ability to perform subgroup analyses, especially for TMT and clinical risk factors. Despite this, the authors succeeded in combining the relatively scarce available data to provide a better understanding of the pathology of oral dysplasia.
Consequently, more research is required in this area. Given the poor prognosis associated with oral leukoplakia and the difficulties in distinguishing it from cancer lesions, there is an urgent need to explore molecular determinants and critical signal pathways underlying the malignant transformation of precancerous to cancerous tissue. Accurate markers would enable the targeting of these lesions for more aggressive treatment and closer follow-up. Smith et al. reported survivin, MMP 9 and DNA content to be potential markers for increased risk of progression from oral dysplasia to cancer.3 In addition, a study by Gouvêa and colleagues focusing on proliferative verrucous leukoplakia, a distinct and aggressive type of oral leukoplakia, observed that high immunoexpression of Mcm-2 and Mcm-5 in mild and moderate dysplasia could be helpful in predicting malignant transformation.4 Despite these findings, tumour markers have so far not gained any use in routine diagnosis and their utility in the prediction of risk of malignant transformation remains unknown.
In the case of oral leukoplakia patients with candidal infection, Cao et al. reported that candidal infection may be one of the most important factors to induce oral dysplasia and malignant transformation of oral leukoplakia. Therefore, saliva cultures should be taken for patients with oral leukoplakia to test for candidal infections.5
To date, there is no evidence of effective treatment in preventing malignant transformation of leukoplakia. Surgical treatments may be effective in the resolution of lesions: however, relapses and adverse effects are common. These include loss of function, increased morbidity and possible need for reconstructive procedures. Future research is needed to identify less invasive and more effective treatments. A case report by Huff et al. described a novel approach to managing mild oral dysplasia using cryotherapy with liquid nitrogen.6 It is noteworthy; however, that the possible effectiveness of less invasive interventions such as laser treatment and cryotherapy are yet to be studied by means of a randomised controlled trial. In the mean time, oral Leukoplakia patients remain in need for continued surveillance, especially in the case of high-grade dysplastic lesions, even following surgical excision.
References
Jaber MA . Oral epithelial dysplasia in non-users of tobacco and alcohol: an analysis of clinicopathologic characteristics and treatment outcome. J Oral Sci. 2010; 52: 13–21.
Lan AX, Guan XB, Sun Z. [Analysis of risk factors for carcinogenesis of oral leukoplakia] in Chinese. Zhonghua Kou Qiang Yi Xue Za Zhi 2009; 44: 327–331.
Smith J, Rattay T, McConkey C, Helliwell T, Mehanna H . Biomarkers in dysplasia of the oral cavity: a systematic review. Oral Oncol. 2009; 45: 647–653.
Gouvêa AF, Vargas PA, Coletta RD, Jorge J, Lopes MA . Clinicopathological features and immunohistochemical expression of p53, Ki-67, Mcm-2 and Mcm-5 in proliferative verrucous leukoplakia. J Oral Pathol Med. 2010; 39: 447–452.
Cao J, Liu HW, Jin JQ . [The effect of oral candida to development of oral leukoplakia into cancer] in Chinese. Zhonghua Yu Fang Yi Xue Za Zhi 2007; 41 Suppl: 90–93.
Huff KD, Garren KC, Huff MS . A novel, minimally invasive approach to managing mild epithelial dysplasia. Gen Dent. 2010; 58: 126–129.
Author information
Authors and Affiliations
Additional information
Address for Correspondence: Hisham M. Mehanna, Department of Head and Neck Surgery, Institute of Head and Neck Studies and Education, University Hospitals Coventry and Warwickshire, Coventry, United Kingdom. E-mail: hisham.mehanna@uhcw.nhs.uk
Mehanna HM, Rattay T, Smith J, McConkey CC. Treatment and follow-up of oral dysplasia - a systematic review and meta-analysis. Head Neck 2009; 31: 1600–1609
Rights and permissions
About this article
Cite this article
Al-Dakkak, I. Oral dysplasia and risk of progression to cancer. Evid Based Dent 11, 91–92 (2010). https://doi.org/10.1038/sj.ebd.6400745
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ebd.6400745