Abstract
Data Sources
Medline and bibliographies of relevant papers were used to source relevant studies. Case reports and references to relevant conference presentations were also included. Animal and in-vitro studies were excluded. Publications in English, French and German were included.
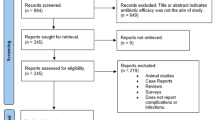
Study selection
All relevant articles including case studies and references to abstracts of conference presentations were considered.
Data extraction and synthesis
A qualitative summary was made of relevant data.
Results
Of 144 articles retrieved, there were 23 prospective studies but no randomised or comparative trials. Twenty-seven reports (18.8%) favoured prophylaxis for special circumstances, 11 publications (7.6%) did not perceive any benefit and 106 (73.6%) took no clear position.
Conclusions
I nfections of total hip or knee replacements because of haematogenous seeding following dental intervention are very rare. The scientific rationale for systemic or local antimicrobial prophylaxis is very weak at best.
Similar content being viewed by others
Commentary
This systematic review of the available evidence relating to antibiotic prophylaxis for patients with hip and knee replacements is timely, as it follows the recent guidance from the UK national institute for health and clinical excellence (NICE).1 NICE recommended that antibiotic prophylaxis is not justified for patients with structural heart disease at risk of infective endocarditis. Although the NICE guidance has been widely disseminated and accepted by national bodies, this is a major change in practice and has generated some anxiety for individual cardiologists, dentists and patients, leading to NICE issuing an interim statement highlighting the importance of professionals following their guidance.
Antibiotic prophylaxis for dental patients with prosthetic joints has been a contentious issue for some time and Seymour et al. (2003)2 undertook a critical review of the then-proposed British Orthopaedic Association and British Dental Association Guidance (Table 1). In their article they addressed three questions: these are summarised, with their responses, in Table 2.
After addressing these questions in detail, Seymour et al. (2003) then considered the proposed guidance, concluding, “the case for providing antibiotic prophylaxis prior to dental treatment in patients fitted with a joint prosthesis is weak or virtually non-existent. Furthermore, the risk from providing prophylaxis is greater than the risk of a joint infection.”
In commenting on this new, more systematic review of the area, it is worth revisiting the questions asked by Seymour and colleagues. In their review, Uçkay et al., highlight a computer simulation paper which indicates a low incidence of joint infections associated with dental infections (0.04%). they also point out that the reports included in the review of infections following a dental procedure often assumed of a dental cause, underlined by microbiological results compatible with oral flora, because of a lack of alternative explanation. In one human prospective study included in the review, which followed 1000 people, only three patients developed joint infections and all were associated with skin microflora.
This review agreed with Seymour et al. (2003) that, although antibiotic prophylaxis reduces bacteraemia, it does not eliminate them. What is clear from the evidence reviewed for the NICE guidance, is that that everyday activities such as chewing causes bacteraemia, and that these activities happen with much greater frequency, and for longer times, than dental procedures.
The present review did not address the cost–risk benefit directly but did come to the same conclusion as Seymour and colleagues, specifically that the scientific rationale for systemic or antibiotic prophylaxis prior to dental treatment in patients with joint prosthesis is very weak at best.
In their editorial in the same journal as this review, Oswald and Gould3 support its conclusions and recommendations, stating, “In summary there is no evidence to link prosthetic joint infections to dental procedures and none to prove that antibiotic is effective. the continued use of antibiotics would be expensive, contribute to an increase in bacterial resistance, lead to increased morbidity as a result of adverse side effects and antibiotic-associated infections and increase the risk of death.”
The Working Party of the British Society for Antimicrobial Chemotherapy emphasised in 19924 that there was no evidence to support the use of antibiotic prophylaxis before dental work in patients with joint replacement, and yet the debate has rumbled on. With the significant change in practice being brought about by the NICE recommendations on antibiotic prophylaxis against infective endocarditis and the increasing concerns over antibiotic resistance, it is time to take note of the available evidence and stop providing people who have had hip and knee replacements with antibiotic prophylaxis for dental procedures.
References
Department of Health. NICE guidance on ‘antibiotic prophylaxis against infective endocarditis’. London: Department of Health; 2008.
Seymour RA, Whitworth JM, Martin M . Antibiotic prophylaxis for patients with joint prostheses — still a dilemma for dental practitioners. Br Dent J 2003; 194:649–653.
Oswald TF, Gould FK . Dental treatment and prosthetic joints: antibiotics are not the answer! J Bone Joint Surg Br 2008; 90:825–826.
Simmons NA, Ball AP, Cawson RA, et al. Case against antibiotic prophylaxis for dental treatment of patients with joint prostheses. Lancet 1992; 339:301.
Author information
Authors and Affiliations
Additional information
Address for correspondence: Professor D Pittet, University of Geneva Hospitals and Faculty of Medicine, 24 Rue Micheli-du-Crest, 1211 Geneva 14, Switzerland. E-mail: didier.pittet@hcuge.ch
Uçkay I, Pittet D, Bernard L, Lew D, Perrier A, Peter R. Antibiotic prophylaxis before invasive dental procedures in patients with arthroplasties of the hip and knee. J Bone Joint Surg Br 2008; 90:833–838
Rights and permissions
About this article
Cite this article
Rodgers, J., Richards, D. No evidence to link prosthetic joint infections with dental procedures. Evid Based Dent 9, 103–104 (2008). https://doi.org/10.1038/sj.ebd.6400609
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ebd.6400609