Abstract
This paper considers the differences in perception of dental treatment between the dentist, a professional, and the lay person.
Similar content being viewed by others
Main
It is generally accepted that dentists know more about dentistry than their patients and that the dental treatment they provide is rooted in scientific and professional knowledge. To suggest otherwise would seem bizarre. Although treatment decisions are founded upon clinical and objective criteria, there is evidence to suggest that doing so at the expense of listening to patients' feelings may lead to difficulties in diagnosis, patient management and subsequent non-compliance with treatment plans.1
There is a tendency for dentists to discount their patients' worries while concentrating on professional and clinical matters. This concentration on clinical matters starts when the dental undergraduate changes from being a lay participant to being an active health professional. The process of professionalisation2 requires the student to discard previously held lay views and accept professional ideas concerning health and causation of disease. As professionalisation continues the student's lay perspectives and health attitudes will be replaced by those of the profession. Professionalisation in this context maps out the process by which the student becomes a dentist. Once graduated the newly qualified dentist will have gained scientific knowledge, power, and autonomy characteristic of any professional group.3
This however only represents one side of the dentist–patient equation. The student's future general practice patients will not have experienced equivalent shifts in their dental health knowledge or related attitudes. The patient who enters the dental surgery may have a lay understanding of dental health matters similar to those held by the dentist prior to training. Within this professional–lay interaction the scene is set for a status differential to exist, characteristic of which, according to Coleman and Burton,4 is that the dentist will know 'everything' (professional knowledge) and the patient will know 'nothing' (lay understanding).
To think of the dentist–patient interaction as one way traffic, with information and treatment flowing from dentist to patient, would be to ignore the dynamic quality of the relationship. By acknowledging that a dynamic interplay (see part 2 of this series) exists provides the dental health professional with the opportunity for effective communication, information exchange and the negotiation of preventive and treatment goals.1 Nevertheless the difficulties that can occur within the treatment alliance may cause disturbances in communication and information exchange with patients. This results from status inequalities within the dentist–patient relationship. The development of the status differential is associated with the professional and lay aspects of the dentist–patient interaction and is exacerbated by the tendency for the patient to perceive the practitioner as an adult figure and to feel like the child (s)he was once (see part 2 of this series). Factors that may contribute to the development of this status differential also include how the participants view the impact of dental symptoms, how they feel symptoms are translated into accessing dental care as well as lay and professional perceptions of treatment need. These factors may have the potential to affect compliance because the same situation may be interpreted differently by dentists and their patients.
The aim of this paper is to discuss each of the above factors in order to examine their potential to cause disruption in the treatment alliance. Understanding that dentists and patients perceive the same dental healthcare situation from different contextual frameworks (professional knowledge versus lay understanding) enables dentists to provide effective care instead of disappointing treatment outcomes and unachievable health goals.
Professional-lay perspective 1: The impact of oral symptoms
What can be learned from Case 1? There seemed to be two different agendas with regard to Mrs P symptoms — professional and lay. For the dentist the physical source of the pain and discomfort were of prime importance: for Mrs P her difficulty in eating, her reduced social contact with family and friends and her low spirits seemed to carry equal weight with the discomfort she experienced. It would be fair to say that Mrs P's quality of life had been affected by her oral symptoms. For Mrs P it was not only the physical impact of her oral symptoms but their psycho-social impact which particularly affected her.
Case 1
Mrs P was an 81 year old widow. She complained of discomfort under her upper complete denture on eating. She had had these symptoms for several months but had attended now because eating was becoming 'impossible'. In fact she had cancelled a family outing as a result of her oral discomfort. She admitted the denture problem was getting her down.
The dentist examined Mrs P's mouth and found nothing clinically wrong. Symptomatic treatment was provided by way of easing of the denture. This afforded Mrs P some relief but she soon returned complaining of the same discomfort as before. The dentist was concerned about the physical origins of Mrs P's pain and referred her to the local dental hospital. Radiographic examination revealed the source of the pain and discomfort — two erupting canines.
The idea that physical symptoms can affect psychological functioning and social interaction is not new. It is almost to be expected in patients with atypical facial pain or burning mouth syndrome.5,6 It has been suggested recently that equivalent feelings are experienced by patients with dental caries, periodontal disease and denture problems.7,8,9,10
Many of these dental patients have difficulties in interacting with family and friends. Some admit to feeling embarrassed when talking, eating or kissing and some will even avoid social occasions altogether. Such avoidance behaviours will exacerbate feelings of anxiety and low-spiritedness resulting in even lower self-esteem and self-confidence11.
Patients, therefore, do not just perceive their oral symptoms in physical terms but also with regard to their quality of life. In this way lay perspectives of the impact of oral symptoms can be thought of as being analogous to a triangle of health,12 being composed of physical, psychological and social dimensions (Figure 1).
Some value may be gained from thinking in this way as it provides a means of understanding why professional and lay perceptions of the impact of oral symptoms differ. The example of patient satisfaction with dentures is illustrative in this regard. A recent study of patient denture satisfaction has shown that whilst patients' concerns were related to comfort (physical), aesthetics (psychological) and communication (social) factors, their dentists rated denture satisfaction in terms of the physical attributes of the denture.10
It would seem that rather than thinking in psycho-social terms dentists tend to restrict their focus to the physical impact dental symptoms have on their patients. For the dental health professional the impact of dental symptoms is perceived mainly in physical terms. This is important in the analysis of patient care, but for the patient symptoms have psychological, social as well as physical impacts.
Professional-lay perspective 2: Translating oral symptoms into dental care
The diversity that exists between the perception of oral symptoms by professionals on the one hand and their impact on patients on the other may provide an indication as to why some people attend routinely and others appear to attend only in an emergency. The issue of how the psycho-social impact of dental symptoms are translated into accessing treatment has been emphasised by Tickle et al.9 They suggest it is the reporting of the physical symptoms together with the psycho-social factors that impact to provide the stimulus to access dental care.
Case 2
Mrs J had been a practice patient for many years and was well known to everyone in the surgery. She attended for her routine examination. On being told that she needed to see the hygienist, Mrs J responded that she had thought she needed a scale and polish and wondered if that clinical session could it be arranged to fit in, in time with her son's wedding - she wanted to 'look good' for the photographs.
How can such ideas relate to a group of patients for whom regular dental care has become part of a health routine and as such contributes to their quality of life? These patients routinely attend, but are not necessarily compelled to do s, because of the impact of physical symptoms. It has been proposed that these patients translate their dental care needs into regular attendance based upon their previous psycho-social experience of being cared for.13 According to Coleman and Burton4 it is at 'the check-up consultation' appointment that professional and lay meanings of attendance are at their closest, that is, the dentist knows 'something' and the patient knows 'something' of the reasons for their meeting.
In terms of professional and lay understanding both the dentist and Mrs J, in Case 2, knew 'something' as to why she had accessed care — her yearly dental visit. Mrs J attended not only in response to her knowing that she needed a scale and polish (physical) but also because she wished to look attractive for her son's wedding (psychological and social). It would seem that psycho-social impacts may play a part with regard to accessing regular care.
When a patient presents at the dental surgery as an emergency the impact of the symptoms in terms of professional and lay understanding may be at their most diverse. Dentists will expect patients to attend as soon as they become aware of their severe oral symptoms. For some patients it is not the symptom alone but rather a combination of the psycho-social impacts together with the symptoms which provides the impetus to seek care. The example of Case 3, Mrs K and her daughter Ann, is illustrative.
Case 3
Mrs K brought her 4 year old daughter, Ann to the emergency dental clinic. She thought that 'a couple of weeks ago' Ann's face had been a little red and possibly swollen but Ann had been 'out of sorts'. Mrs K had thought little of it as Ann had not complained of toothache. However for the last couple of nights Ann's sleep had been disrupted. In fact the whole household had been disturbed with Ann crying about her 'sore mouth'. Mrs K was shocked to discover that Ann had a number of decayed teeth and that one appeared abscessed. Mrs K felt that something had to be done to relieve her daughter's pain. In addition she stated 'we're all in need of a good night's sleep'.
The issue of translating the psycho-social impact of dental symptoms into treatment is clear in the example of Ann. Tickle et al.9 suggest that it is the reporting of the physical symptom that provides the stimulus to access dental care. In the above illustration it was Ann's reporting of her 'sore mouth' together with the disruption of the household at night which provided the stimulus for mother to access care. Mother was unaware of the true state of her daughter's dentition until onset of acute symptoms. It was not physical need alone that enabled the mother to access care but the psycho-social impact of her daughter's dental symptoms.
Translating symptoms into care will be different for dentists and their patients. Professionally, dentists perceive physical symptoms as the impetus for accessing dental treatment. For patients psycho-social impacts may carry equal weight with physical discomfort and together provide the stimulus to seek dental care. The effect of this may be to distort further the dentist–patient interaction with regard to perceptions of professional-lay treatment need.
Professional-lay perspective 3: Perceptions of treatment need
The concept of need reflects the difficulties inherent within the professional–lay dimension of the dentist–patient relationship. This is because need means different things to different people. A plethora of definitions of need exists.14 These range from statements about professional assessments of health status to definitions associated with treatment procedures. In order to clarify such diversity in the definition of need three different categories have been identified. These are normative, expressed and felt need (Table 1). The greatest mismatch in perception of need exists in relation to unmet treatment need. It is in the need for treatment of unmet oral health needs that the professional–lay differential can have the greatest influence upon the treatment alliance.
The reasons for this are quite clear. The dental health professional's concept of need is related to their professional knowledge and skills and is hence connected to the patient's physical dental health status. The patient's concepts of need are related to psycho-social influences such as previous dental experiences and dental phobia status. The dentist's clinical skill and judgement lead to a diagnosis together with the formulation of an appropriate treatment plan. Successful treatment outcome will be dependent upon the patient's capacity to use the treatment offered. Redford and Gift1 have stated 'before any recommended treatment can be delivered, information exchange and value negotiation must take place between dentist and patient'. The need for the dental health professional to grasp the importance of the patient's ability to understand the necessity of the treatment offered will maintain an equality within the treatment alliance and lead to a successful outcome.
Case 4
Mr G, a 35 year old unmarried patient, had a number of deep periodontal pockets. He had been referred for periodontal care. He had now returned to the practice for maintenance therapy during which the hygienist routinely examined his mouth. However she was becoming increasingly concerned about Mr G's poor plaque control and subsequent gingivitis. Based upon her clinical experience and skill she believed that there was an unmet treatment need and began to formulate a preventive treatment plan (normative need). Mr G stated that he found it difficult to stick to the advice given to him so that he infrequently used the floss or inter-dental brushes he had been advised to buy. He felt that his gums looked 'healthy enough', 'didn't hurt' and 'were OK'. He just did not see the point to all of this. As long as his mouth looked alright and he had no pain or discomfort then he really would prefer to leave things as they were (expressed need). In fact he thought it was a waste of time and money (felt need).
In Case 4 there had been no prior discussion or information exchange with regard to referral for specialist care or maintenance programme. The scene was therefore set for a mismatch in the perception of need for periodontal treatment. The patient Mr G was unable to use the periodontal treatment provided by the hygienist because he had not understood the need to care for his own mouth between visits to the hygienist. The treatment alliance between Mr G and his dental health professionals had been disturbed resulting in an unsuccessful treatment outcome.
Professional-lay perspective 4: Implications for practice
It has been suggested that patients' health care and treatment needs are in fact continually changing and will be traded against other more urgent or important life needs.15 Health needs are therefore sensitive to changes in socio- economic and/or employment status and have a tendency to vary in response to personal, family and life circumstances (psycho-social influences). Evaluating health care needs in this way connects the psycho-social impacts of dental symptoms with accessing care and with perceptions of treatment need. From a lay perspective dental symptoms affect the quality of life but psycho-social impacts also influence expressed and felt treatment needs. Therefore changes which occur in lifestyle will affect the perception of the impact of dental symptoms and treatment need. However, equivalent shifts in professional perception of treatment need may not have occurred. The dentist's perception of the patients' normative need may remain the same and hence provide a situation in which a clash occurs between the patients' changing expressed and felt needs and the professional's static normative need. The result of this clash between professional and lay perspective may result in patients leaving unsatisfied with the dental care they have received.
Example 1
A male patient complained that the crown on a central incisor was defective and he demanded to have it replaced. After a detailed examination the dentist agreed the crown was, to some extent, clinically defective. The old crown was removed, impressions taken and colour chosen with the patient's approval. The dentist was surprised when the patient returned some weeks after the crown had been fitted to say that it was unsatisfactory and stated it to be 'defective'. The dentist replaced the crown for a second time but the patient found it again 'defective' and requested a second opinion from a consultant. He confided to the consultant that his family circumstances had changed in that his youngest child had moved into residential care as she was severely disabled. The patient described his daughter as 'defective'. He had always hoped that his daughter would become perfect. It seemed that his wish for a perfect daughter and a perfect crown were synonymous. He remained dissatisfied with his treatment and decided to seek legal advice.
Example 2
Ms L was 28 years old when she presented. She had not been for dental treatment for many years and admitted to being 'terrified'. Many of her teeth were broken and she knew that they needed attention although they were not causing much in the way of discomfort. She felt that something had to be done before her 'front teeth went the same way'. She confided to the dentist and the dental nurse that her new partner had insisted that she have dental treatment. It was as if the option was 'visit the dentist or we finish'. By acknowledging Ms L's felt need for dental care a negotiated treatment was agreed. The treatment outcome was successful.
In the two short examples above the first illustrates that when the normative need is influenced by the patient's demands for care, the patient may remain dissatisfied with the treatment outcome and consider litigation. The second case illustrates how an acknowledgement of the psycho-social influences on the patient's dental health status together with felt and expressed needs can lead to a successful treatment outcome.
Conclusions
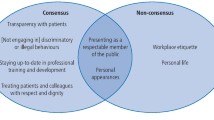
The aim of this article was to present some guidance on professional and lay perspectives of the dentist–patient interaction. It would seem that a gulf may potentially exist between the way in which dental health professionals think about oral health and disease compared with their patients. It was suggested that this potential gulf may alter the dynamics of the treatment alliance. For the health professional thoughts about the impact of dental symptoms, how these are translated into accessing care and the need for dental treatment, were based upon clinical and physical dimensions of health, but this is not always so for the patient. From a lay perspective the impact of dental symptoms includes not only physical but also psychological and social dimensions. The means by which oro-facial symptoms are translated into accessing dental care and treatment need are also subjected to psycho-social influences.
Dental health professionals, by acknowledging that differences exist, will be able to maintain the equality of the dentist-patient interaction. By discussing and negotiating preventive regimes and treatment plans they will be able to provide effective dental care.
References
Redford M, Gift H C . Dentist-patient interactions in treatment decision-making: a qualitative study. J Dent Educ 1997; 61: 16–21.
Weare K . The contribution of education to health promotion. In Health Promotion: Disciplines and Diversity R Bunton and G MacDonald (Eds). London. Routledge 1993.
Locker D . An introduction to behavioural science and dentistry. London, Routledge 1989.
Coleman H, Burton J . Aspects of control on the dentist-patient relationship. Int Soc. Lang 1985; 51: 75–104.
Lamey P J, Lamb A B . Prospective study of the aetiological factors in burning mouth syndrome. Brit Med J 1988; 296: 1243–1246.
Freeman R A . psychotherapeutic approach to the understanding and treatment of a psychosomatic disorder: the case of burning mouth syndrome. In Centres and peripheries of psychoanalysis: an introduction to psychoanalytic studies. R Ekins and R Freeman (Eds). London. Karnac Books. 1994.
Leao A, Sheiham A . The development of a socio-dental measure of dental impacts on daily living. Community Dental Health 1996; 13: 22–26.
Adulyanon S., Vourapukjaru J. Sheiham A . Oral impacts affecting daily performance in a low dental disease Thai population. Community Dent Oral Epidemiol 1996; 24: 385–389.
Tickle M, Craven R, Blinkhorn A S . An evaluation of a measure of subjective oral health status in the UK. Community Dental Health 1997; 13: 175–180.
Ettinger R L, Jakobsen J R . A comparison of patient satisfaction and dentist evaluation of overdenture therapy. Community Dent Oral Epidemiol 1997; 25: 223–227.
Fiske J, Davis D M, Frances C, Gelbier S . The emotional effects of tooth loss in edentulous people. Brit Dent J 1998; 184: 90–93.
Freeman R . The triangle of health: applications for general practice part 1 the clinical arena. Dental UpDate 1997; 24: 61–63.
Jacob C, Plamping D The practice of primary health care. Bristol. Wright. 1989.
Sheiham A, Maizels J, Cushing A . New composite indicators of dental health. Community Dental Health 1987; 4: 407–414.
Ong B N . The practice of health services research. London: Chapman & Hall: 1993.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Freeman, R. Reflections on professional and lay perspectives of the dentist–patient interaction. Br Dent J 186, 546–550 (1999). https://doi.org/10.1038/sj.bdj.4800166
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4800166
This article is cited by
-
A study of parental presence/absence technique for child dental behaviour management
European Archives of Paediatric Dentistry (2017)
-
The effect of parental presence on the child’s perception and co-operation during dental treatment
European Archives of Paediatric Dentistry (2016)
-
Influence of parental presence on the child’s perception of, and behaviour, during dental treatment
European Archives of Paediatric Dentistry (2011)
-
A dental anxiety scale for children
British Dental Journal (2005)
-
An investigation of paediatric dentists' attitudes towards parental accompaniment and behavioural management techniques in the UK
British Dental Journal (2002)