Key Points
-
A prospective study 1581 consecutive adult patients tested whether general dental practitioners are able to select patients appropriately for day case oral surgery
-
The referral criteria developed in this study improved the appropriateness of referrals. Patients referred directly to the day case unit without prior hospital assessment were judged appropriate in 82% of cases, a similar percentage to that recorded from the consultant clinics (83%)
-
The direct referral system resulted in fewer patient visits to hospital, shorter waiting times and improved attendance rates
-
Despite the proposed benefits of a direct referral system it was only used by a small number of GDPs.
Abstract
Direct referral of patients for day case surgery by general medical practitioners (without hospital assessment) has become widely accepted but few facilities exist for this form of referral from general dental practice. In order to evaluate whether direct access day surgery is applicable to dentistry, the quality of referral by GDPs and hospital consultant clinics was compared in a prospective study (1994–1997) involving 1581 patients.
Similar content being viewed by others
Main
Historically patients have been referred first to a hospital consultant clinic and then redirected for assessment on a separate occasion to a day case clinic prior to attending on a third occasion for surgery (three visit surgery). In a recent study, applying these principles to ENT surgery, it was estimated that 'direct listing' would save the NHS £1.2 million per annum.1 As third molar removal is the eighth commonest surgical procedure undertaken in the NHS2 a similar saving is possible in this surgical discipline. If the proposed one visit system (where by the patient is assessed, operated on and discharged on the same day) proved effective it would complement the shift in NHS policy from inpatient to day case surgery and apart from reducing cost would reduce the number of hospital visits for the patient.3
The dental surgeon is ideally suited to this shift in responsibility as surgery is an integral part of dental practice. A further advantage to the dental practitioner is that the operation date can be provided directly while the patient is in attendance by phoning or faxing the day case unit. This system could also be usefully adopted by surgical specialists,4 in the primary care sector.
This study was designed to establish if a direct listing is a realistic proposition for oral surgery.
How did we go about trying to achieve this?
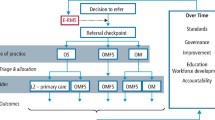
The project was undertaken on the oral surgery day case unit of the United Medical and Dental Schools (Jan 1994 – Feb 1997) and 1581 patients recruited in three groups. At the start of the project, the patients were referred to the day case unit from other hospital consultant clinics which involved a three visit process (Group 3, N = 741). In January 1994, 200 GDPs in the catchment area were provided with referral guidelines and informed of a new service whereby they could refer patients directly to the day case unit for pre-operative assessment. The patients were then booked on a separate occasion for surgery (Group 2, N = 739). In December 1995, the GDPs already referring directly to the unit were encouraged to use a one-visit system (Group 1, N = 101). GDPs were able to use any of the three referral routes according to their preference (fig. 1).
The referral guidelines for day case anaesthetic (fig. 2) were derived from The Royal College Guidelines,5 the Poswillo Report6 and analysis of the medical literature.7,8,9,10,11,12 Criteria for selecting surgical cases were generated from an analysis of day case patients treated in the previous 4 years as well as a review of the medical literature.13,14,15 The main criteria was that the duration of operation should be < 1 hour.16 Data was collected prospectively on a specifically designed database.
The main end-points in this study were accuracy of diagnosis, the appropriateness of surgical treatment plan and acceptance for day case surgery. In addition, the choice of referral pathway on waiting times and attendance was also assessed.
Despite the apparent advantages provided by a direct referral system only a minority of practitioners (12 of 200) made use of the one visit system. Possible explanations are a lack in effective marketing of the new system, time constraints in practice and also a reluctance of practitioners to take added responsibility for surgical treatment plans and medical assessment, both of which have medico-legal implications. The system will work optimally when used by enthusiastic practitioners who pay careful attention to selection criteria.
Furthermore, for the one visit system to work effectively the general practitioner must have the option to use a two visit programme (Group 2), for in this project GDPs intuitively directed the more problematic cases into a two visit pathway where the patients could be reassessed by hospital personnel and accounts for the poor results in this group. Another factor that became apparent was that one visit surgery did not suit all patients and the familiarity and reassurance provided by a two visit system must not be underestimated.
Were the referrals appropriate?
A one visit day case system (Group 1) proved effective and feasible to provide. The accuracy of diagnosis for the three Groups was '1' = 98%; '2' = 48% and '3' = 86%, and the choice of surgical treatment plan was judged to be appropriate in 98%, 34% and 82% of cases. The ultimate measure of this service is the percentage of cases that proceeded to surgery under general anaesthesia (fig. 3). Groups 1 and 3 had an acceptance rate for surgery of 82% and 83% compared to only 49% for Group 2.
Patients were appropriately referred in 82%, 49% and 83% cases (Groups 1, 2 and 3, respectively); 27% of Group 2 cases had to be redirected for LA or LA and IV sedation. Only 3.5% of cases assessed by GDPs (Groups 1 and 2) had to be diverted from day case to in-patient treatment. Overall, 18% of patients had no indication for surgery.
The probable explanation as to why Group 1 patients (one visit) were better selected is that they represented simpler cases and were referred by a small cohort of seven enthusiastic general practitioners. These practitioners formed part of the slightly larger group of dentists (n = 12) who referred 40% of Group 2 cases.
Issues that proved problematic for GDPs were choice of anaesthesia and accuracy of diagnosis for surgery. This was particularly evident in Group 2 for many of these patients (51%) did not require general anaesthesia and were redirected for the surgery under LA/ LA sedation (fig. 3). A significant proportion of patients in all Groups requested general anaesthetic without clinical indications. The request and acceptance for GA was highest in Group 1 reflecting the inability to change treatment plan on the day of surgery, and lowest in those patients reassessed by the day case unit team (fig. 4). Redirection of patients from day case to inpatient surgery was recorded in 9% of patients referred from the consultants clinic, and 3.5% from the other two groups. This change of treatment was mainly for medical and social reasons (Table 1). One limitation to the one visit day case system is that it has very little reserve built into the process, and if patients are selected inappropriately and are not suitable for surgery then operating facilities are wasted. The commonest referral was for third molar complaints (87%) but in 12% of these cases the diagnosis was incorrect as the symptoms arose from the TMJ.
The medical and surgical criteria used to select patients for day case oral surgery proved appropriate as post-operative medical complications were rare. Only 0.003% of patients required admission after treatment, a marked improvement on previous studies.17,18 This study confirms that by using a combination of the two direct referral systems, GDPs are capable of selecting patients for day case oral surgery on both surgical and anaesthetic grounds.19
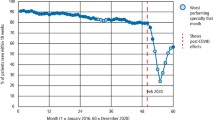
The effect of the three different pathways on reliability of attendance demonstrated that Groups 1 and 2 patients had a significantly higher overall pre-operative and operative attendance rate than Group 3 (85% versus 37%). The improved attendance rate might be explained by a shorter treatment delay (from GDP referral to treatment). The delay for Group 3 patients (168 days) was partly due to waiting times for outpatient clinics (generally > 60 days) but despite the short treatment delays for Groups 1 and 2 (69 days for Group 1, 90 days for Group 2), the attendance rate on the day of surgery was still only 85%. In Group 1, the ability to provide surgery within a short period of referral did not appeal to most patients. A delay of around 8 weeks, to make appropriate domestic and work arrangements, was preferred.
Conclusion
In order to establish if direct access surgery was applicable to oral surgery, a set of criteria had to be developed that selected patients appropriately, both with respect to surgery and suitability for anaesthesia. These have been tested and proved effective. However, the uptake of the new referral system was disappointing and reflects reluctance to change well-established and cherished referral patterns to trusted colleagues. A further inhibitory factor was that GDPs had to assume additional clinical responsibility for which there was no incentive. The climate may have change however, with the recent GDC directive on the use of general anaesthesia in dentistry, and in due course the criteria may prove more helpful to the referring clinician.
The implications of this study are that the guidelines formulated can be used to improve the quality and suitability of GDPs referrals to oral surgery units. In an appropriate setting the direct system of referral has application in day case oral surgery.
References
Shah C, Griffiths M, Moralee S . Direct listing for adult tonsillectomy. J Royal Coll Surg Edin 1997; 42: 45–46.
Shepherd J, Brickley M . Surgical removal of third molars. Br Med J 1994; 309: 620–621.
Joshi A, Snowdon A . Direct access for day case oral surgery (a personal communication). Brit Assoc Day Surgery Meeting, 1994.
White paper on Provision of personal dental services. Care in the Community. London: HMSO, 1996.
Guidelines for day case surgery. London: Roy Coll Surg Eng. 1985, revised March 1992.
'Poswillo Report'. Principal recommendations of the report of an expert working party on general anaesthesia, sedation and resuscitation in dentistry. Department of Health, 1990.
Commission on the provision of surgical services. Report of a working party on pain after surgery. London: College of Anaesthesia. Roy Coll Surg Eng, 1990.
Day surgery — making it happen. Value for money unit. NHS Management Executive. London: HMSO, 1991.
Measuring the quality: the patient's view of day surgery. Audit Commission, NHS occasional papers. No. 3, May 1991.
The Audit Commission for local authorities and the National Health Service for England and Wales: a short cut to better service. Day surgery in England and Wales. London: HMSO, 1990.
Barnard N, Williams R, Spencer E . Pre-operative patient assessment. A review of the literature and recommendations. Ann Roy Coll Surg Eng 1994; 76: 293–297.
Meridy H W Criteria for selection of ambulatory surgical patients and guidelines for anaesthetic management. A retrospective study of 1533 cases. Anaesthesia Analgesia 1982; 61: 921–924.
Mercier P, Precious D . Risks and benefits of removal of impacted third molars: A critical review of the literature. Int J Oral Maxfac Surg 1992; 21: 17–27.
Lopes V, Mumenya R, Feinman C, Harris M . Third molar surgery:an audit of indications for surgery, post operative complaints and patient satisfaction. Br J Oral Maxfac Surg 1995; 33: 33–35.
Shepherd J . Evidence-based indications for third molar removal. Dental Defence Union Focus 1996; 2: 8–10.
Weil T M, Akerson H A, Alling C C, Davis W M. Jr Parameters of care for oral and maxillofacial surgery: A guide for practice, monitoring and evaluation.(AAOMS parameters of care in dentoalveolar surgery). J Oral Max Fac Surg 1995 (supplement 5); 53: 31–59.
Yee K F, Holland R B, Carrick A, Vincent S J . Morbidity following day stay dental anaesthesia. Aust Dent J 1985; 30: 333–335.
Chye E P, Young I G, Osborn G A, Rudkin G E . Outcomes after same day oral surgery: a review of 1180 cases at a major teaching hospital. J Oral Maxillofac Surg 1993; 51: 846–849.
Joyson O B, Williams S L, Brickley M R, Shepherd J P . Lower third molar treatment planning ability of the general dental practitioners and oral maxillofacial surgeons using receiver operating characteristics methodology. Br Dent J 1996; 181: 411–415.
Acknowledgements
This project was funded by the Department of Health and administered by the Clinical Audit Committee of the Royal College of Surgeons of England. Anne Reid was the appointed project assistant, her computer skills were instrumental in introducing this report and we thank Mr J Lowry for his support with this project.
Author information
Authors and Affiliations
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Renton, T., McGurk, M. Direct referral day case oral surgery for dental practitioners: a pilot investigation. Br Dent J 186, 334–337 (1999). https://doi.org/10.1038/sj.bdj.4800103
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4800103
This article is cited by
-
One-stop endoscopic hernia surgery: efficient and satisfactory
Hernia (2015)
-
A controlled trial of three referral methods for patients with third molars.
British Dental Journal (2000)
-
Direct access day case oral surgery
British Dental Journal (2000)