Abstract
Pseudomyxoma peritonei syndrome is a disease characterized by mucinous ascites and mucinous tumor disseminated on peritoneal surfaces; the disease almost always originates from a perforated appendiceal epithelial tumor. Histopathologic assessment of aggressive versus noninvasive character of the mucinous tumor has been shown to have an impact on survival in patients treated with cytoreductive surgery and intraperitoneal chemotherapy. Out of a database of 312 patients having a complete cytoreduction for pseudomyxoma peritonei syndrome, 46 patients (24 male and 22 female) had at least one second-look surgery. Before this review, all 46 of these patients were clinically uniformly categorized with a diagnosis of pseudomyxoma peritonei. Using the criteria described by Ronnett and colleagues, all specimens from the multiple surgical procedures performed on these patients were reviewed and reclassified as disseminated peritoneal adenomucinosis (adenomucinosis), adenomucinosis/mucinous adenocarcinoma (hybrid), or mucinous adenocarcinoma. The review was performed in a blinded fashion by a single pathologist (HY). To facilitate a critical evaluation of these histopathologic assessments, the patients were separated into two groups: (1) 19 patients who had a second-look surgery that was unsuccessful in that they went on to die of their disease or in that they currently have disease progression and a limited survival and (2) 27 patients who had a successful second look and currently continue disease free with a minimum 3-year follow-up period. As a result of this review, 11 of 19 patients with an unsuccessful second look and originally designated pseudomyxoma peritonei were reclassified as hybrid-type malignancy (four patients) or mucinous adenocarcinoma (seven patients). Only two patients were reclassified in the successful second-look group (P =.0005). Transitions from a less aggressive to a more invasive histology from one cytoreduction to the next occurred on 13 occasions in patients whose second-look surgery failed and in one patient with a successful second-look surgery (P <.0001). Seven patients retained a histologic classification of disseminated peritoneal adenomucinosis but went on to die of an aggressive disease process. Clinical assessments suggested that failure of second-look surgery for pseudomyxoma peritonei was associated with a biologically more aggressive disease. Unsuccessful second-look surgery for patients with a clinical diagnosis of pseudomyxoma peritonei tumor was often related to an inaccurate initial histologic classification of appendiceal mucinous tumor. Also, a transition from less to more aggressive histology was frequently seen in patients dying of this disease. Assessment of tumor histology can predict the outcome if a uniform surgical treatment is used in patients with peritoneal dissemination of mucinous epithelial tumors of the appendix.
Similar content being viewed by others
INTRODUCTION
Pseudomyxoma peritonei syndrome is a rare disease usually characterized by a perforated appendiceal epithelial tumor that causes mucinous ascites and multifocal mucinous tumor implants diffusely involving the peritoneal surfaces. The syndrome includes patients with diverse and poorly predictable prognosis. Since Werth first introduced the term pseudomyxoma peritonei in 1884 (1), its features, definition, origin, and prognosis have been debated for more than a century. Recently, morphologic, immunohistochemical, and molecular genetic studies have analyzed a large number of pseudomyxoma peritonei cases in an effort to document the appendix as the primary site in both men and women and to more clearly define the natural history of the disease (2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12). Also, the description of a new histopathologic classification of appendiceal mucinous tumors suggested that prognosis was correlated with morphology if a uniform treatment strategy was used. In the publication by Ronnett and coworkers (5), the mucinous appendiceal tumors were classified as disseminated peritoneal adenomucinosis, peritoneal mucinous carcinomatosis, or hybrid tumor. This new histologic classification may be significant for understanding the history of this disease and in helping pathologists and surgeons to knowledgeably treat it. The purpose of this study was to correlate the morphology, as defined by the modern classification, with the results of a uniform treatment plan to test the predictive value it offered over an extended time period. Forty-six patients who had multiple tissue samples available at a minimum of three different surgeries were used to complete this evaluation.
MATERIALS AND METHODS
Clinical Features
From a database of 312 patients with a clinical diagnosis of pseudomyxoma peritonei syndrome, an attempt was made to retrieve and review the clinical data and the pathologic material on all patients who had at least one second-look procedure between 1987 and 1999. The original histologic diagnoses in all these patients was low-grade mucinous appendiceal tumor or malignancy compatible with pseudomyxoma peritonei. These histologic diagnoses were made before the uniform application of the Ronnett criteria to the evaluation of mucinous appendiceal tumors. This included the appendectomy specimen and the peritoneal surface mucinous tumor. All patients underwent an appendectomy for their primary appendiceal tumor at an outside institution (n = 38) or at Washington Hospital Center concomitantly with cytoreductive surgery (n = 8). The 46 patients eligible for this analysis were separated into two categories based on failure versus success with second-look surgery: 19 patients who failed the treatment approach and went on to die of their disease or who currently have progressive disease (failure group) and 27 patients who currently have disease-free survival (success group).
Histopathological Classification
In a blinded re-study, all tissue specimens were reclassified according to Ronnett's criteria (4, 5); the average number of slides reviewed for each patient was 50, with a range of 30 to 90. The tissues were divided into one of three following histological categories of mucinous appendiceal epithelial malignancies. Then, the group identified as mucinous adenocarcinoma was subdivided as well differentiated, moderately differentiated, or poorly differentiated. Each patient, at a minimum of three different points in time, had the histology of these mucinous tumors identified as one of five different subtypes.
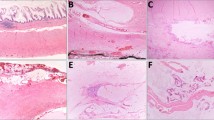
Adenomucinosis was characterized by multifocal mucinous tumors adherent to but not invading into visceral and parietal peritoneal surfaces. Microscopically, the peritoneal lesions contained scant histologically benign mucinous epithelium within abundant extracellular mucin (Fig. 1). An intense hyalinizing fibrotic reaction that separated pools of mucin was another important histologic feature of this lesion. Also, the dissecting quality of the mucin was consistent. Intraoperatively, the mucinous implants have a characteristic distribution by peritoneal fluid and by the forces of gravity. There was noninvasive involvement of the parietal peritoneal surfaces with sparing of the peritoneal surfaces of the bowel and its mesentery. This has been referred to as a redistribution phenomenon (8). The need to distinguish secondary involvement of the ovaries by a perforated mucinous appendiceal tumor from mucinous borderline tumors of the ovary has been previously established (7).
Mucinous adenocarcinoma was characterized by invasive peritoneal lesions composed of abundant epithelium with glandular or signet-ring cell morphology with sufficient architectural complexity and cytological atypia to warrant a diagnosis of mucinous adenocarcinoma (Fig. 2). Mucinous adenocarcinomas were further separated into three grades (13) by evaluating epithelial content of the tumors in order to more completely describe the histological progression (1). Well-differentiated mucinous adenocarcinoma was composed predominantly of single tubular glands. The tumor cells were well polarized similar to epithelium of an adenoma. Atypia of the tumor cells was remarkable, and an invasive component was identified (2). Moderately differentiated mucinous adenocarcinoma showed characteristics between well- and poorly differentiated adenocarcinoma. It was composed of solid sheets of malignant cells admixed with glandular formations. The polarity of the tumor cells was minimal or absent (3). Poorly differentiated adenocarcinoma was composed of highly irregular glandular structures or lacked glandular differentiation. The polarity of the cancer cells had disappeared completely. In some cases, signet-ring cells were seen.
Hybrid appendiceal mucinous tumors as described by the Ronnett criteria included foci of intermediate type and diffuse peritoneal adenomucinosis histology present within the same clinical material. The hybrid tumors predominantly demonstrate histologic features of adenomucinosis; however, focal areas (lower than 5% of the tumor cells) of well-differentiated adenocarcinoma were identified in peritoneal lesions (Fig. 3). Because the tissue processing was performed at many different institutions, the extent of sampling was not uniform for all cases. Copious tissue obtained through the procedures performed at our institution and multiple operations performed reduced the possibility of sampling errors.
Hybrid type of appendiceal mucinous tumor predominantly demonstrated features of disseminated peritoneal adenomucinosis (right upper corner). However, as shown in the center of the photomicrograph, if sufficient tissue is examined, focal areas of well-differentiated adenocarcinoma are identified. (hematoxylin and eosin, × 80). In this patient, 15 slides showed disseminated peritoneal adenomucinosis, and in 1 of these, foci of mucinous adenocarcinoma was identified. The cystic foci seen in this figure adjacent to areas of adenocarcinoma are not likely to be dilated glands of carcinoma. They represent the predominant histologic pattern of diffuse peritoneal adenomucinosis seen in this patient.
Peritoneal Cancer Index
The peritoneal cancer index is a quantitative assessment of cancer distribution of tumor throughout the abdomen and pelvis (14). Two components are involved in its calculation. One component is the distribution of tumor in the abdominopelvic regions, and the other component is the lesion size score. The abdominopelvic regions are defined by anatomic landmarks that surround the abdominal and pelvic cavity. Two transverse planes and two sagittal planes are used to divide the abdomen in nine abdominopelvic regions. The upper transverse plane is located at the lowest aspect of the costal margin. The lower transverse plane is placed at the anterior superior iliac spine. The sagittal planes divide the abdomen into three equal sectors. The regions are numbered 0–8, starting at the umbilical region and proceeding in a clockwise manner. The small bowel was separately scored as four regions; the upper jejunum was 9, lower jejunum 10, upper ileum 11, and lower ileum 12. Peritoneal cancer index scores vary between 0 (no tumor seen) and 39.
Cytoreduction
All patients underwent a cytoreductive surgical procedure (as described elsewhere; 15) that was always performed by the same surgical team. Briefly, the goal of surgery was to remove all visible tumor within the peritoneal cavity. Up to six different peritonectomy procedures were used as necessary in various combinations to remove all visible evidence of tumor. These procedures included a greater omentectomy with splenectomy, left upper-quadrant peritonectomy, right upper-quadrant peritonectomy, lesser omentectomy with cholecystectomy, partial or total resection of the stomach, and pelvic peritonectomy with resection of the rectosigmoid colon.
Completeness of Cytoreduction Score
The completeness of cytoreduction score is an assessment of the volume of disease that remains after the surgery (14). The site containing the largest amount of residual disease following cytoreductive surgery must be recorded. Completeness of cytoreduction is indicated by CC-0 through CC-3. A CC-0 resection indicates patients in whom no tumor is visualized in the entire abdomen and pelvis during the course of the complete resection. These are patients with walled-off tumor nodules or tumor encased within scar tissue or are patients who may have had complete response to induction chemotherapy. CC-1 resections leave behind tumor nodules less than 2.5 mm in greatest diameter. CC-2 resections are those that have residual tumor between 2.5 mm and 2.5 cm in diameter. The CC-3 resections are in patients in whom tumor more than 2.5 cm in diameter is left behind or a confluence of tumor at any site.
Intraperitoneal Chemotherapy
Intraoperatively, the abdomen and pelvis were lavaged with heated chemotherapy using 3 L of 1.5% dextrose peritoneal dialysis solution with mitomycin C. This was followed by 5 days of early postoperative intraperitoneal chemotherapy with 5-fluorouracil (16).
Statistical Analysis
Fisher's exact test was performed, and the results are given in Tables 1, 2 and 3. A Kaplan-Meier survival analysis was fitted to the data and tested using a log rank test for difference between rates.
RESULTS
Patients from the failure group were between 31 and 69 years of age (mean, 45 y), and patients from the success group were between 29 and 61 years of age (mean, 45 y) at the time of their appendectomy. There were 9 males and 10 females in the failure group and 15 males and 12 females in the success group. Of these 46 patients, 38 underwent an appendectomy and a partial resection of peritoneal surface mucinous tumors at an outside institution; the slides or paraffin blocks were available for review on 24. In all eight patients who had the appendectomy at Washington Hospital Center, the slides of appendix were available for review. In all initial cytoreductions, second-look, third-look, and fourth-look procedures performed at the Washington Hospital Center, complete histologic material were available for a review.
The initial evaluation was to compare the original diagnosis of pseudomyxoma peritonei given by the surgeon and a staff pathologist with that determined by a review according to the histologic features described by Ronnett et al. (4, 5) In the failure group, 11 of 19 patients (57.9%) had the primary appendiceal tumor and the peritoneal surface tumors reclassified as hybrid (four patients) or mucinous adenocarcinoma (seven patients). In the success group, two of 27 patients (7.4%) were reclassified upon review of the initial tissues sampled (Table 1). There was a prominent association of failure of second look with an inaccurate original classification of the abdominal mucinous tumors (P =.0005).
Histologic evaluation also included a search for evidence: a transition of histologic appearance from a less to a more aggressive type was sought (Table 2). At the time of initial cytoreduction, 6 of the 19 patients in the failure group showed an increasingly aggressive histopathology between the time of the initial diagnosis and the first cytoreduction. The transition was from adenomucinosis to hybrid type in three patients, from hybrid to well-differentiated mucinous adenocarcinoma in one, and from well-differentiated to more aggressive mucinous adenocarcinoma in two. In the group with a successful second look, only a single transition occurred between initial diagnosis and first cytoreduction.
As shown in Table 2, similar transitions occurred between the time of first cytoreduction and second look in the failure group. Transition from adenomucinosis to hybrid was observed in one patient, transition from hybrid to well-differentiated mucinous adenocarcinoma in three patients, and transition from well-differentiated mucinous adenocarcinoma to a more aggressive mucinous adenocarcinoma in three patients.
A single transition between first cytoreduction and second look was observed in the success group; this is the only histologic assessment from a more- to a less-aggressive histology observed in this histologic review. Two patients in the success group patients did show a progressive transition at a later time in their clinical course. One had focal well-differentiated adenocarcinoma with lung metastases at a third-look surgery, and another had focal well-differentiated adenocarcinoma on peritoneal surfaces at a fourth-look procedure. Both these two patients remain free of disease or alive with the disease at 10-year and 12-year follow-ups, respectively, from the initial diagnosis.
A perplexing group of seven patients were those who went on to die of this disease despite a pathology that was consistently interpreted as adenomucinosis. These patients showed adenomucinosis at the time of their initial diagnosis, at the time of their first cytoreduction, and at the time of a second cytoreduction. However, in all seven of these patients at the time of second-look surgery, the redistribution of mucinous tumor implants had ceased, and diffuse involvement of surfaces of the small bowel and small-bowel mesentery was observed. All of these patients went on to die of progressive intraabdominal disease.
The median survival of patients from the initial cytoreduction in the failure group was studied using the Kaplan-Meier method. Median survival for the group with the adenomucinosis (n = 8) was 81 months; for hybrid (n = 4), the median survival was not reached; and for mucinous adenocarcinoma (n = 7), it was 40 months. There was no significant difference in the survival of the patients when the three groups of patients who failed the treatment were compared. The group of patients consistently showing adenomucinosis went on to die at a rate not statistically different from the hybrid and the mucinous adenocarcinoma patients. None of the patients appeared to have an indolent type of disease.
A search was made for clinical features that would explain the failure vs. success with a second-look surgery. The items that were statistically analyzed are shown in Table 3. The peritoneal cancer index determined the extent of disease at the time of the first cytoreduction; it did not show differences in these two groups. However, if the peritoneal cancer index recorded at the time of second look indicated multiple sites of recurrent disease, it was a strong prognostic indicator (P =.0011). Likewise, a failure of the peritoneal cancer index to change from a high value at the time of initial cytoreduction to a low value at the time of second-look surgery was also significant (P <.0001). Completeness of cytoreduction at the initial cytoreduction was not significant when the second-look failures were compared with second-look success. However, completeness of cytoreduction at the time of second- or third-look surgery was highly significant (P <.0001 and P =.012).
DISCUSSION
The hypothesis entertained when initiating this study was that mucinous appendiceal tumors over time and with repeated surgical and intraperitoneal chemotherapy interventions may change to a more invasive process. These data supported this hypothesis in that 13 transitions from a less to a more aggressive histology were observed in 19 patients with treatment failure as compared with in 2 of 26 patients who are free of disease. Transitions from a less aggressive to a more aggressive histology were much more likely to occur in patients who failed this uniform treatment and went on to die of their disease.
It is quite possible that differences in chemotherapy penetration of mucinous and solid tumors may result in a persistence and a progression of the more solid components of a non-uniform tumor tissue. The hybrid appendiceal tumors are described as having large areas of adenomucinosis with small, even minute, areas of more aggressive malignant tissue. In areas of residual disease after cytoreductive surgery, the penetration of intraperitoneal chemotherapy into the mucin that contains adenomatous epithelial cells may eradicate these cells. However, even small foci of solid tumor may not be completely penetrated by chemotherapy. Consequently, the foci of more aggressive tumors are areas that become evident at second-look surgery in patients having progressive disease.
This study confirms the importance of a complete and knowledgeable initial histopathologic evaluation in the assessment of prognosis of pseudomyxoma peritonei syndrome. Approximately one half of the patients failing second-look surgery did not have the correct diagnosis at the initial clinical and histologic assessment. A histologic assessment of “well-differentiated mucinous neoplasm” was not sufficient to indicate the prognosis of these patients with disseminated appendiceal mucinous tumors (4, 5). In our opinion, this general terminology should be discarded by pathologists when describing mucinous epithelial appendiceal tumors. An inaccurate clinical and pathologic assessment of the original malignancy accounted for the poor result with second-look surgery in many patients.
Seven patients who had a tumor histopathology that was consistently adenomucinosis did not conform to the expected natural history, that is, small-bowel sparing and an indolent course. These seven patients all had extensive tissue resection, so histopathologic errors in classification from inadequate sampling were unlikely. In these patients, a tissue morphology of adenomucinosis was associated with death from progressive disease at the same rate as with mucinous adenocarcinoma or hybrid type of mucinous tumor. Explanations for this lack of clinical/pathologic correlation were not immediately apparent.
An important distinction between two tumors that may have a similar histologic appearance but different histogenesis (appendiceal mucinous tumors and mucinous borderline tumors of the ovary) has been made by Young and colleagues (7). They suggested that ovarian mucinous tumors that presented synchronously with similar mucinous tumors of appendix were secondary ovarian tumors rather than primary ovarian cancer. A histologic appearance of copious acellular mucus with mucus dissecting through the ovarian stroma, right-sided or bilateral ovarian mucinous tumors, and the taller epithelium lining in cysts in the ovarian tumors than usual primary ovarian tumors help to exclude the ovary as a primary site. Although the simultaneous occurrence of a perforated appendiceal mucinous tumor and a borderline ovarian tumor is remotely possible, secondary involvement of the ovary by an appendiceal primary tumor is the usual condition.
The hybrid type of peritoneal surface malignancy from an appendiceal malignancy is a controversial category. Identification of adenocarcinoma cells mixed with predominantly peritoneal mucinous adenomatosis is a frequent occurrence. Yet considerable difficulty in clearly defining the hybrid type of mucinous tumor exists. What quantity of atypia is sufficient to qualify the specimen as hybrid? What extent of histologic sampling is sufficient to rule out hybrid-type mucinous tumor? Is it possible that the apparent transitions reported in this manuscript can be explained by inconsistencies in sampling? The break point between diffuse peritoneal adenomucinosis and hybrid type of mucinous tumor is not likely to be the same for different pathologists. This creates a subjectivity in reading appendiceal histopathology. Perhaps all hybrid types of mucinous tumors can be classified as mucinous adenocarcinoma? In the grading of most malignancies, the histologic appearance of the most aggressive foci of cancer determines the category.
Table 3 is an attempt to identify clinical factors that could explain failure versus success with second-look procedures. Concomitant versus prior resection of the primary tumor was suggested as an important prognostic variable for colon cancer (17). This was not meaningful with these appendiceal tumors. Also, the prior surgical score shown to be a meaningful prognosticator for appendiceal tumors was not important in this group of patients having a second look (18). The extent of the primary malignancy at the time of the initial cytoreduction (failure group, 26 and successful group, 30) by the peritoneal cancer index was not predictive of outcome. Neither was there a difference in the completeness of cytoreduction at the first cytoreductive surgery. Significant differences between the failure group and the success group occurred when these parameters were compared at second-look and at third-look surgery. A decrease in the peritoneal cancer index between the first and second cytoreduction is an important prognosticator. In the failure group, the peritoneal cancer index decreased little if at all between the first- and second-look surgeries. In contrast, in the success group, the mean peritoneal cancer index decreased between the first- and second-look surgeries. Also, an incomplete resection with second-look surgery predicted a significantly reduced survival. In the failure group, the frequency of incomplete resection was 63%; in the successful group, it was 0%. The more aggressive growth potential of the mucinous tumors showing hybrid-type or mucinous adenocarcinoma histology and the transitions from a less to a more aggressive histology was thought to be responsible for the marked difference in the outcome between the groups as a result of second-look surgery.
Perforated appendiceal tumors may represent a paradigm by which to study peritonectomy, intraperitoneal chemotherapy, and the knowledgeable management of carcinomatosis. The wide spectrum of clinical behavior and tumor morphology has allowed an assessment of prognosis by histologic criteria. The histopathologic classification of these mucinous appendiceal malignancies correlated with the clinical outcome if a uniform treatment strategy aiming at cure was utilized. If there is an accurate initial histologic assessment, two caveats remain in the application of these prognostic designations to patients with the clinical diagnosis of pseudomyxoma peritonei. With repeated use of cytoreductive surgery plus intraperitoneal chemotherapy to remove mucinous tumors and ascites, a transition from a less to more aggressive histopathology may occur. This was a prominent association with treatment failure. A more disconcerting exception to accurate prognostication by histopathology was observed in seven patients who had three or more cytoreductions to treat adenomucinosis. Even with a complete cytoreduction and no revisions in their histopathology, these patients went on to die of this disease. Explanation for the poor results of treatment of these seven patients requires further investigation. One hypothesis is that extensive prior surgery and the conversion of a peritoneal surface tumor to a deeply embedded one as a result of extensive surgical dissection may have occurred (19). Or these mucinous tumors may have had unusually poor response to the intraperitoneal mitomycin C and 5-fluorouracil used to eliminate microscopic residual disease.
References
Werth R . Klinische und anatomische untersuchungen zur lehre von den bauchgeschwuelsten und der laparotomie. Arch Gynaekol 1884; 24: 100–118.
Ronnett BM, Shmookler BM, Diener-West M, Sugarbaker PH, Kurman RJ . Immunohistochemical evidence supporting the appendiceal origin of pseudomyxoma peritonei in women. Int J Gynecol Pathol 1997; 16: 1–9.
Cuatrecasas M, Matias-Guiu X, Prat J . Synchronous mucinous tumors of the appendix and the ovary associated with pseudomyxoma peritonei. A clinicopathologic study of six cases with comparative analysis of c-Ki-ras mutations. Am J Surg Pathol 1996; 20: 739–746.
Ronnett BM, Shmookler BM, Sugarbaker PH, Kurman RJ . Pseudomyxoma peritonea: new concepts in diagnosis, origin, nomenclature, and relationship to mucinous borderline (low malignant potential) tumors of the ovary. Anat Pathol 1997; 2: 197–226.
Ronnett BM, Zahn CM, Kurman RJ, Kass ME, Sugarbaker PH, Shmookler BM . Disseminated peritoneal adenomucinosis and peritoneal mucinous carcinomatosis. A clinicopathologic analysis of 109 cases with emphasis on distinguishing pathologic features, site of origin, prognosis, and relationship to “pseudomyxoma peritonei” Am J Surg Pathol 1995; 19: 1390–1408.
Prayson RA, Hart WR, Petras RE . Pseudomyxoma peritonei. A clinicopathologic study of 19 cases with emphasis on site of origin and nature of associated ovarian tumors. Am J Surg Pathol 1994; 18: 591–603.
Young RH, Gilks CB, Scully RE . Mucinous tumors of the appendix associated with mucinous tumors of the ovary and pseudomyxoma peritonei. A clinicopathological analysis of 22 cases supporting an origin in the appendix. Am J Surg Pathol 1991; 18: 415–429.
Sugarbaker PH, Ronnett BM, Archer A, Averbach AM, Bland R, Chang D, et al. Pseudomyxoma peritonei syndrome. Adv Surg 1997; 30: 233–280.
Szych C, Staebler A, Connolly DC, Wu R, Cho KR, Ronnett BM . Molecular genetic evidence supporting the clonality and appendiceal origin of pseudomyxoma peritonei in women. Am J Pathol 1999; 6: 1849–1855.
Guerrieri C, Franlund B, Boeryd B . Expression of cytokeratin 7 in simultaneous mucinous tumors of the ovary and appendix. Mod Pathol 1995; 8: 573–576.
Ronnett BM, Kurman RJ, Zahn CM, Shmookler BM, Jablonski KA, Kass ME, et al. Pseudomyxoma peritonei in women: a clinicopathologic analysis of 30 cases with emphasis on site of origin, prognosis, and relationship to ovarian mucinous tumors of low malignant potential. Hum Pathol 1995; 26: 509–524.
Ronnett BM, Kurman RJ, Shmookler BM, Sugarbaker PH, Young RH . The morphologic spectrum of ovarian metastases of appendiceal adenocarcinomas: a clinicopathologic and immunohistochemical analysis of tumors often misinterpreted as primary ovarian tumors or metastatic tumors from other gastrointestinal sites. Am J Surg Pathol 1997; 21: 1144–1155.
Fenoglio-Preiser CM, Pascal RR, Perzin K . Tumors of the intestines. Atlas of tumor pathology. 2nd series, Fascicle 27. Washington, DC: Armed Forces Institute of Pathology; 1990.
Jacquet P, Sugarbaker PH . Current methodologies for clinical assessment of patients with peritoneal carcinomatosis. J Exp Clin Cancer Res 1996; 15: 49–58.
Sugarbaker PH . Peritonectomy procedures. Annu Surg 1995; 221: 29–42.
Sugarbaker PH . Management of peritoneal surface malignancy using intraperitoneal chemotherapy and cytoreductive surgery: a manual for physician and nurses. Grand Rapids, MI: The Ludann Co.; 1993. p. 13–23.
Pestieau SR, Sugarbaker PH . Treatment of primary colon cancer with peritoneal carcinomatosis: A comparison of concomitant versus delayed management. Dis Colon Rectum (in press).
Sugarbaker PH . Results of treatment of 385 patients with peritoneal surface spread of appendiceal malignancy. Ann Surg Oncol 1999; 6: 727–731.
Zoetmulder FA, Sugarbaker PH . Patterns of failure following treatment of pseudomyxoma peritonei of appendiceal origin. Eur J Cancer 1996; 32A: 1727–1733.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yan, H., Pestieau, S., Shmookler, B. et al. Histopathologic Analysis in 46 Patients with Pseudomyxoma Peritonei Syndrome: Failure versus Success with a Second-Look Operation. Mod Pathol 14, 164–171 (2001). https://doi.org/10.1038/modpathol.3880276
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3880276
Keywords
This article is cited by
-
Long-term results of laparoscopic cytoreductive surgery and HIPEC for the curative treatment of low-grade pseudomyxoma peritonei and multicystic mesothelioma
Surgical Endoscopy (2020)
-
Pathology of Mucinous Appendiceal Tumors and Pseudomyxoma Peritonei
Indian Journal of Surgical Oncology (2016)
-
Female patients with pseudomyxoma peritonei: a single-institution clinicopathologic study of 35 cases
Archives of Gynecology and Obstetrics (2014)
-
Clinicopathological analysis of primary epithelial appendiceal neoplasms
Medical Oncology (2010)
-
Interstitial pneumonitis following intrapleural chemotherapy
World Journal of Surgical Oncology (2009)