Abstract
Ovarian cancer and second malignant neoplasms are found to occur rather frequently in the same patient. From a clinical perspective, it is important to have quantitative information on concurrent malignancies in the same year of diagnosis of the epithelial ovarian cancer. In this population-based study, we used data from the Netherlands Nationwide Network for Registry of histo- and cytopathology (PALGA) and the Netherlands Cancer Registry (NCR). Data of the ovarian cancer as well as data on previous or later cancers were obtained. Age-specific cancer rates from the NCR were used to calculate expected numbers of cancer. Between 1987 and 1993, histopathology reports were identified of 4577 patients with primary epithelial malignant or primary borderline malignant ovarian cancers and its longitudinal data. As the database may lack detailed information on histopathology, a recent sample of 789 patients diagnosed with ovarian cancer in 1996–2003 was comprehensively studied as well. In the eventual data analysis of 5366 patients, 244 cases (4.5%) of concurrent primary malignancy were reported in the same year that the malignant epithelial ovarian tumor had been diagnosed against 51 expected. The observed vs expected ratio was 4.8 and the 95% confidence interval (CI) (4.3–5.5). For cancer of the uterus/endometrium the observed vs expected ratio was 62.3 (95% CI 52.5–73.5). For skin, breast, colorectal, urinary bladder, renal and cervical cancer the ratio was also larger than unity. The elevated risk of concurrent cancer may lead to clinical screening protocols. The findings on endometrial cancer may prompt research on common etiologies and biomarkers.
Similar content being viewed by others
Main
Most cases of epithelial ovarian cancer, which constitute 80–90% of all ovarian malignancies, are diagnosed at an advanced stage.1 The prognosis is poor with 5-year survival rates of about 40%.2 Survival for women with ovarian cancer has improved, such that the occurrence of second malignant neoplasms is surfacing. One study reported increased risk of second primary ovarian cancer in women diagnosed previously with cancer of different sites.3 When the time-window of occurrences is narrowed to say 1 year, the clinical implications and prognosis become warrant. Most ovarian cancers are adenocarcinomas, which are derived from the surface epithelium. These present in several distinctive histopathologic forms, such as cystadenocarcinoma with serous or mucinous differentiation or endometrioid tumors with endometrial-like tubular gland structures. Endometrial neoplasms also include adenocarcinomas, which showed well-defined, glandular structures as in endometrioid carcinoma. According to the sparse literature, the simultaneous presence of primary cancers in the ovary and the endometrium was initially a rare event, but an association has been reported by Sheu et al.4 From 421 patients diagnosed with a primary ovarian carcinoma, six cases showed a simultaneously primary endometrial carcinoma.
Multiple primary tumors may arise because of inherited or acquired cellular lesions or deficiencies,5 for example, because of environmental exposure to carcinogens. Ovarian carcinoma, breast and endometrial or even colon carcinoma are linked mechanistically to reproductive hormones. Thus, similarities in the spectrum of second neoplasms may be expected. Genetic and reproductive factors predisposing to ovarian cancer may also contribute to the elevated risk of breast, colorectal neoplasms and possibly melanoma.6, 7
The objective of the present study was to determine the excess risk of a concurrent primary malignant tumor in women with malignant primary epithelial ovarian tumor.
Materials and methods
Patient Information
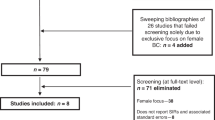
This project was performed using protocols approved by the PALGA Utilization Committee: PALGA, Dutch acronym and short for Pathologisch Anatomisch Landelijk Geautomatiseerd Archief, the Netherlands Nationwide computer Network for Registry of cyto/histopathology. All patients with a new ovarian cancer diagnosis in the period from 1987 to 1993, and registered as such in PALGA were included in this study. A small sample was taken from 1996 to 2003. The PALGA database is a national archive containing the abstracts of all histopathology and cytopathology reports in the Netherlands since 1991. For 1987, the coverage was approximately 75% depending on the participating pathology departments in PALGA in the Netherlands, whereas for 1988 and 1989, the coverage was already 90% and for 1990 almost 100%. Every record in the database contains a summary of the report and diagnostic codes similar to the Systematized Nomenclature of Medicine (SNOMED)5 classification of the College of American Pathologists. It also contains date of diagnosis and age at diagnosis. PALGA was not able to select primary cancers only.
Of the patients with epithelial ovarian cancer (malignant or borderline malignant), we obtained all other histopathologically confirmed diagnoses of primary invasive malignancies, previously, concurrently or after the diagnosis of the ovarian tumor. Uncertain diagnoses, and reports on recurrences or metastases were also included. Wrong coding of the pathologist can hamper the interpretation of diagnostic codes. Therefore, we studied the second more recent and smaller group of cases with a primary epithelial malignant ovarian neoplasm.
Of each case, not only the diagnostic codes in the PALGA database were reviewed, but also the corresponding pathology conclusions, that is, PALGA code and PALGA conclusion. This was also carried out for the other malignant occurring neoplasms. Two experienced pathologists (GPV, JB) reviewed all reports. Difficult cases were excluded, if it was not sure that we were dealing with a metastasis of the primary malignant tumor of the ovary or a new secondary type of tumor out of the ovaries. Basal cell and squamous cell carcinomas of the skin were also considered as malignant tumors. For the current study, other malignant primary cancers were only included if diagnosed in the same calendar year as the ovarian tumor.
Statistical Methods
The ovarian cancers were stratified to age at diagnosis in 5-year categories. Second malignancies were categorized in similar manner. To compute the expected numbers of second primaries in each of the 16 age-categories (Table 1), for several types of cancer the year and age-specific cancer incidence rates from the Netherlands Cancer Registry 1989–2003 were multiplied by the annual number of ovarian cancers.8 For 1987 and 1988, NCR incidence data of the year 1989 were used. The age-specific incidence rates of basal cell carcinoma were obtained from the Eindhoven Cancer Registry.9
The assumption was that a patient had been at risk of diagnosis of other primary cancers for the entire year in which the ovarian cancer had been diagnosed. However, for patients in whom ovarian cancer had been diagnosed at the beginning of the calendar year, but who had died shortly thereafter, the actual period at risk for the diagnosis of another primary cancer will have been shorter than 1 year. Therefore, the number of expected cancers may be underestimated.
For each type of cancer, the number of observed second primary cancers divided by the expected number, the O/E ratio, and its 95% confidence interval (CI) were calculated according to the method of Byar.10
Results
In the study period, 5366 cases of primary epithelial malignant tumors were selected from the PALGA registry, 4577 in the period 1987–1993 and 789 in the period 1996–2003 (Table 1). In these 5366 patients, 244 (4.5%) cases of concurrent primary malignancy were reported in the same year that the malignant epithelial ovarian tumor had been diagnosed. From these 244 cases, 10 new malignancies were detected in the ovaries (some of sexcord-stromal origin, germ cell tumor or different epithelial histological type).
For both study groups, primary malignant epithelial ovarian tumor was most prevalent in age category 65–69 years. The highest number of concurrent malignancies was observed mostly in patients aged 50–54 years.
For these patient numbers obtained, we calculated the observed vs expected number (O/E ratio) of the concurrent primary malignant cancers. As the magnitude of the O/E ratio from 1996 to 2003 did not differ from those of the larger database from 1987 to 1993, we decided to put the data together (Table 2). From Table 2, it can be seen that for all sites the number of concurrent primary cancer was 4.8 times as high as the expected number (95% CI 4.3–5.5).
Of the 244 concurrent malignancies, 142 (58.3%) originated from the uterus or endometrium. This yielded an O/E ratio of 62.3 (95% CI 52.5–73.5). Significantly increased risks were also found for kidney cancer (O/E ratio=19.7, 95% CI=6.3–45.9), cervical cancer (O/E=14.9, 95% CI=5.5–32.5), bladder cancer (O/E=13.4, 95% CI=3.6–34.4), colorectal cancer (O/E=5.2, 95% CI=3.4–7.6) and breast cancer (O/E=2.3, 95% CI=1.5–3.3). The excess risk for melanoma skin cancer (O/E ratio=7.4) and non-melanoma skin cancer (basal cell cancer included; O/E=1.6) did not reach statistical significance.
Discussion
As a result of the anatomical location and the many imaging techniques that can visualize the entire abdomen, ovarian tumors and endometrial tumors are often diagnosed together. The association between ovarian tumors and endometrial tumors has also been noted in population-based epidemiological studies.5 These tumors are linked mechanistically to reproductive hormones. Thus, similarities in the spectrum of second neoplasms may be expected.5 For most sites, our findings are moderately in accordance with the results from literature.2, 3, 4, 5, 6, 7, 11, 12, 13 Our results show that from 5366 patients diagnosed with a malignant primary epithelial ovarian tumor, 142 cases also manifested a concurrent endometrial malignancy (2.6%). Sheu et al report six cases from 421 ovarian cancer patients, who were also diagnosed with a synchronously endometrial cancer. Some considerations can be made. First of all, our data were restricted to epithelial ovarian cancer.
A discrepancy is that very often synchronous tumors are defined as those occurring within 6 weeks before or after the diagnosis of ovarian cancer, whereas in our study the concurrent tumors were selected in the same year of ovarian tumor diagnosis. A methodological reason may be the calculation of expected numbers, which has been occurring only recently in literature.
Besides, detection bias may explain a part of the increased risks of second primary cancers diagnosed in the same year as the ovarian cancer. As patients in whom ovarian cancer is suspected undergo extensive diagnostic testing, the probability that another cancer in the abdominal area is also detected may be quite large. It is not possible to estimate the extent of this bias.14 However, it is highly unlikely that this bias can explain an O/E ratio as high as 4–5.
A second peculiar kind of bias in population screening, but in clinical screening as well, is the lead-time effect. Lead-time is defined as the interval between the time of detection by screening and the time at which the disease would have been diagnosed in the absence of screening. It is the time by which screening advances diagnosis of the disease.14 In the diagnosis and staging of cancer, the entire abdomen will be screened. But, as the influence of lead-time bias diminishes over time, and our O/E ratios remain rather stable over time beyond the period of 1 year (data not presented), lead-time bias does not explain the excess risks.
Difficulties come forward in differential diagnosis, when the ovarian cancer is accompanied by a cancer of the uterine corpus. In the literature, it is reported that evidence in favor of synchronous primary neoplasms of both organs occurs as those cancers mostly have an excellent prognosis especially if the tumors are confined to both organs.15 However, in some cases the relation of the two tumors in both organs (two primaries or metastasis from one to another, especially in case of endometriod adenocarcinomas at both sites) is difficult to interpret from the code files only. Therefore, in case of serious doubt (ie about 25% or more uncertainty according to the experienced review pathologists GPV, JB), we excluded those cases for the concurrent cancer from further analysis. The same type of problem arises when an adenocarcinoma of the colorectal and a carcinoma of the ovary are involved, particularly in case of a mucinous type of adenocarcinoma of the ovary. These problematic cases were also excluded from further analysis, when serious doubt arises about the origin of both tumors. As there is still some doubt after this leaving out procedure at a level of 25% uncertainty, in a small number of cases when the tumors are simultaneously present in ovary and uterus or colorectum, the observed O/E ratio still may be somewhat biased of these two sites of origin. Therefore, we studied the two different study populations, the first one from 1987, to 1993 and the second from 1996 to 2003. The results of these separate populations were almost the same.
The above-mentioned problems will not occur for the other reported simultaneously occurring tumors, because all of them are other tumor types and morphologically quite different from the usually adenocarcinoma tumor types arising in the ovary (mucinous, serous, endometrioid and clear cell tumor types). Those malignancies (malignant melanoma of the skin, transitional cell carcinoma of the urinary bladder, renal cell carcinoma, squamous cell carcinoma of the skin and the cervix uteri and invasive ductal and lobular carcinoma of the breast) could be easily distinguished by the pathologist using standard histomorphological criteria whereas considering the microscopic slides.
Women of childbearing age willing to become pregnant and in whom the adenocarcinoma is restricted to one of the ovaries, only the ovary with the tumor is usually resected. Especially in these women, it is important that the clinician is informed about the status of the endometrium, as the risk of a simultaneous second primary tumor in this group of patients is very high. For the other types of secondary primary tumors elsewhere, alternative screening protocols may be considered (eg cervical smears, investigation of the urinary bladder for urothelial carcinoma, inspection of the skin for melanomas).
We conclude that in 4–5% of women diagnosed with a primary malignant epithelial ovarian tumor, a second new malignant primary tumor is occurring in the same year of the ovarian tumor, particularly in the endometrium where about more than half of these concurrent cancers are found. Also, an increased risk of colorectal, kidney, urinary bladder, cervix, mamma or skin malignancy was observed. The large number of second new primaries demand further evaluation of risk by histological type of epithelial ovarian tumors and may lead to new clinical screening protocols. The relations between some of these cancers suggest that future research should focus on common etiologies and biomarkers.
References
Weiss NS, Cook LS, Farrow DC . Ovarian cancer. In: Schottenfeld D, Fraumeni Jr JF (eds). Cancer Epidemiology and Prevention, 2nd edn. Oxford University Press: New York, 1996, pp 1040–1057.
Riman T, Dickman PW, Nilsson S, et al. Risk factors for invasive epithelial ovarian cancer: results from a Swedish case–control study. Am J Epidemiol 2002;156:363–373.
Hall HI, Jamison P, Weir HK . Second primary ovarian cancer among women diagnosed previously with cancer. Cancer Epidemiol Biom Prev 2001;10:995–999.
Sheu BC, Lin HH, Chen CK, et al. Synchronous primary carcinomas of the endometrium and ovary. Int J Gynecol Obstet 1995;51:141–146.
Hemminki K, Aaltonen L, Li X . Subsequent primary malignancies after endometrial carcinoma and ovarian carcinoma. Cancer 2003;97:2432–2439.
Travis LB, Curtis RE, Boice Jr JD, et al. Second malignant neoplasms among long-term survivors of ovarian cancer. Cancer Res 1996;56:1564–1570.
Hartge P, Tucker MA, Shields JA, et al. Casecontrol study of female hormones and eye melanoma. Cancer Res 1989;49:4622–4625.
Netherlands Cancer Registry. http://www.ikcnet.nl/page.php?id=41(accessed 21 April 2006).
Eindhoven Cancer Registry: Comprehensive Cancer Centre South (IKZ); 1990–2000; 29 (personal communication).
Snedecor GW, Cochran WG . Sampling of attributes. In: Statistical Methods, 6th edn. The Iowa State University Press: Ames, Iowa, 1974, pp 3–31.
Buiatti E, Crocetti E, Acciai S, et al. Incidence of second primary cancers in three Italian population-based cancer registries. Eur J Cancer 1997;33:1829–1834.
Kehoe S, Powell JE . Prior, synchronous and secondary malignancies in women with ovarian cancer. Int J Gynecol Obstet 2001;73:265–267.
Bertone-Johnson ER . Epidemiology of ovarian cancer: a status report. Lancet 2005;365:101–102.
Vineis P . History of bias. In: Morabia A (ed). History of Epidemiologic Methods and Concepts. Birkhäuser Verlag: Basel, 2004, pp 327–336.
Scully RE, Young RH, Clement PB . Tumors of the ovary, maldeveloped gonad, fallopian tube and broad ligament. In: Rosai J, Sobin LH (eds). Atlas of Tumor Pathology, 3rd series, Vol. 23. Armed Forces Institute of Pathology Press: Washington, 1998, pp 125–126.
Acknowledgements
We thank Idie Casparie MD, Bert G Siebers MSc, and Henk de Leeuw for data handling at the Stichting PALGA. We are also deeply indebted to Eric Brummelkamp for his help in data analysis. This work was supported by an internal grant of the department of Epidemiology and Biostatistics in Nijmegen. There were no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van Niekerk, C., Vooijs, G., Bulten, J. et al. Increased risk of concurrent primary malignancies in patients diagnosed with a primary malignant epithelial ovarian tumor. Mod Pathol 20, 384–388 (2007). https://doi.org/10.1038/modpathol.3800752
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3800752
Keywords
This article is cited by
-
Risks of non-ovarian cancers in women with borderline ovarian tumor: a national cohort study in Sweden
BMC Cancer (2023)
-
Uterine involvement in epithelial ovarian cancer and its risk factors
Journal of Ovarian Research (2021)
-
Endometrium is not the primary site of origin of pelvic high-grade serous carcinoma in BRCA1 or BRCA2 mutation carriers
Modern Pathology (2013)
-
Second primary cancers following borderline ovarian tumors
Archives of Gynecology and Obstetrics (2011)