Abstract
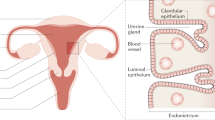
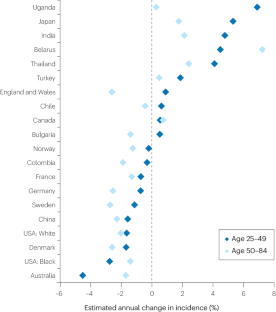
Globally, ovarian cancer is the eighth most common cancer in women, accounting for an estimated 3.7% of cases and 4.7% of cancer deaths in 2020. Until the early 2000s, age-standardized incidence was highest in northern Europe and North America, but this trend has changed; incidence is now declining in these regions and increasing in parts of eastern Europe and Asia. Ovarian cancer is a very heterogeneous disease and, even among the most common type, namely epithelial ovarian cancer, five major clinically and genetically distinct histotypes exist. Most high-grade serous ovarian carcinomas are now recognized to originate in the fimbrial ends of the fallopian tube. This knowledge has led to more cancers being coded as fallopian tube in origin, which probably explains some of the apparent declines in ovarian cancer incidence, particularly in high-income countries; however, it also suggests that opportunistic salpingectomy offers an important opportunity for prevention. The five histotypes share several reproductive and hormonal risk factors, although differences also exist. In this Review, we summarize the epidemiology of this complex disease, comparing the different histotypes, and consider the potential for prevention. We also discuss how changes in the prevalence of risk and protective factors might have contributed to the observed changes in incidence and what this might mean for incidence in the future.
Key points
-
The disease we call ‘ovarian’ cancer encompasses a wide range of tumour types, including cancers that arise in the fallopian tube; changes in coding and reporting make incidence trends over the past decade difficult to interpret.
-
Between 1920 and 1960, successive birth cohorts had lower risk of developing ovarian cancer, although incidence might be increasing again in women born after about 1970.
-
With the recognition that high-grade serous cancers originate in the fallopian tube, salpingectomy (opportunistic or targeted) offers the opportunity for prevention and could delay the need for oophorectomy among women with a high genetic risk.
-
Hormonally related factors, including pregnancy, oral contraceptive use and breastfeeding, reduce the risk of ovarian cancer, particularly the endometrioid and clear cell histotypes; the benefits of newer contraceptive formulations are less clear.
-
Lifestyle exposures, including smoking, obesity and, potentially, sedentary behaviour or inactivity, all increase the risk of a woman developing the less common histotypes but do not appear to affect the risk of developing the most common high-grade serous cancers.
-
If current trends continue, the incidence of ovarian cancer might start to increase, although widespread uptake of salpingectomy and expanded identification and interventions targeting BRCA mutation carriers have the potential to reduce incidence.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
McCluggage, W. G., Singh, N. & Gilks, C. B. Key changes to the World Health Organization (WHO) classification of female genital tumours introduced in the 5th edition (2020). Histopathology 80, 762–778 (2022).
Shih, I. M., Wang, Y. & Wang, T. L. The origin of ovarian cancer species and precancerous landscape. Am. J. Pathol. 191, 26–39 (2021).
Cheasley, D. et al. The molecular origin and taxonomy of mucinous ovarian carcinoma. Nat. Commun. 10, 3935 (2019).
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249 (2021).
Webb, P. M., Green, A. C. & Jordan, S. J. Trends in hormone use and ovarian cancer incidence in US white and Australian women: implications for the future. Cancer Causes Control. 28, 365–370 (2017).
Cabasag, C. J. et al. The influence of birth cohort and calendar period on global trends in ovarian cancer incidence. Int. J. Cancer 146, 749–758 (2020).
Ervik, M., Lam, F., Laversanne, M., Ferlay, J. & Bray, F. Global Cancer Observatory: Cancer Over Time https://gco.iarc.fr/overtime (2021).
GBD 2019 Cancer Risk Factors Collaborators. The global burden of cancer attributable to risk factors, 2010-19: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 400, 563–591 (2022).
Long Roche, K. C., Abu-Rustum, N. R., Nourmoussavi, M. & Zivanovic, O. Risk-reducing salpingectomy: let us be opportunistic. Cancer 123, 1714–1720 (2017).
Nitschke, A. S., do Valle, H. A., Dawson, L., Kwon, J. S. & Hanley, G. E. Long-term non-cancer risks in people with BRCA mutations following risk-reducing bilateral salpingo-oophorectomy and the role of hormone replacement therapy: a review. Cancers 15, 711 (2023).
Yoon, S. H., Kim, S. N., Shim, S. H., Kang, S. B. & Lee, S. J. Bilateral salpingectomy can reduce the risk of ovarian cancer in the general population: a meta-analysis. Eur. J. Cancer 55, 38–46 (2016).
Chen, Y., Du, H., Bao, L. & Liu, W. Opportunistic salpingectomy at benign gynecological surgery for reducing ovarian cancer risk: a 10-year single centre experience from China and a literature review. J. Cancer 9, 141–147 (2018).
Hanley, G. E. et al. Outcomes from opportunistic salpingectomy for ovarian cancer prevention. JAMA Netw. Open 5, e2147343 (2022).
Darelius, A., Kristjansdottir, B., Dahm-Kahler, P. & Strandell, A. Risk of epithelial ovarian cancer type I and II after hysterectomy, salpingectomy and tubal ligation — a nationwide case-control study. Int. J. Cancer 149, 1544–1552 (2021).
Duus, A. H., Zheng, G., Baandrup, L., Faber, M. T. & Kjaer, S. K. Risk of ovarian cancer after salpingectomy and tubal ligation: prospects on histology and time since the procedure. Gynecol. Oncol. 177, 125–131 (2023).
Leblanc, E. et al. Prophylactic radical fimbriectomy with delayed oophorectomy in women with a high risk of developing an ovarian carcinoma: results of a prospective national pilot study. Cancers 15, 1141 (2023).
Webb, P. M. & Jordan, S. J. Epidemiology of epithelial ovarian cancer. Best Pract. Res. Clin. Obstet. Gynaecol. 41, 3–14 (2017).
Peres, L. C. et al. Racial/ethnic differences in the epidemiology of ovarian cancer: a pooled analysis of 12 case-control studies. Int. J. Epidemiol. 47, 460–472 (2018).
Jervis, S. et al. Ovarian cancer familial relative risks by tumour subtypes and by known ovarian cancer genetic susceptibility variants. J. Med. Genet. 51, 108–113 (2014).
Flaum, N., Crosbie, E. J., Edmondson, R. J., Smith, M. J. & Evans, D. G. Epithelial ovarian cancer risk: a review of the current genetic landscape. Clin. Genet. 97, 54–63 (2020).
Norquist, B. M. et al. Inherited mutations in women with ovarian carcinoma. JAMA Oncol. 2, 482–490 (2016).
Phelan, C. M. et al. Identification of 12 new susceptibility loci for different histotypes of epithelial ovarian cancer. Nat. Genet. 49, 680–691 (2017).
Setiawan, V. W. et al. Type I and II endometrial cancers: have they different risk factors? J. Clin. Oncol. 31, 2607–2618 (2013).
Gong, T. T., Wu, Q. J., Vogtmann, E., Lin, B. & Wang, Y. L. Age at menarche and risk of ovarian cancer: a meta-analysis of epidemiological studies. Int. J. Cancer 132, 2894–2900 (2013).
Wentzensen, N. et al. Ovarian cancer risk factors by histologic subtype: an analysis from the ovarian cancer cohort consortium. J. Clin. Oncol. 34, 2888–2898 (2016).
Yarmolinsky, J. et al. Appraising the role of previously reported risk factors in epithelial ovarian cancer risk: a Mendelian randomization analysis. PLoS Med. 16, e1002893 (2019).
Yang, H. et al. Age at menarche and epithelial ovarian cancer risk: a meta-analysis and Mendelian randomization study. Cancer Med. 8, 4012–4022 (2019).
Fu, Z. et al. Lifetime ovulatory years and risk of epithelial ovarian cancer: a multinational pooled analysis. J. Natl Cancer Inst. 115, 539–551 (2023).
Husby, A., Wohlfahrt, J. & Melbye, M. Pregnancy duration and ovarian cancer risk: a 50-year nationwide cohort study. Int. J. Cancer 151, 1717–1725 (2022).
Wu, Y., Sun, W., Xin, X., Wang, W. & Zhang, D. Age at last birth and risk of developing epithelial ovarian cancer: a meta-analysis. Biosci. Rep. 39, BSR20182035 (2019).
Lee, A. W. et al. Expanding our understanding of ovarian cancer risk: the role of incomplete pregnancies. J. Natl Cancer Inst. 113, 301–308 (2021).
World Cancer Research Fund/American Institute for Cancer Research. Diet, Nutrition, Physical Activity and Cancer: A Global Perspective (World Cancer Research Fund International, 2018).
Gaitskell, K. et al. Histological subtypes of ovarian cancer associated with parity and breastfeeding in the prospective Million Women Study. Int. J. Cancer 142, 281–289 (2018).
Babic, A. et al. Association between breastfeeding and ovarian cancer risk. JAMA Oncol. 6, e200421 (2020).
Kotsopoulos, J. et al. Breastfeeding and the risk of epithelial ovarian cancer among women with a BRCA1 or BRCA2 mutation. Gynecol. Oncol. 159, 820–826 (2020).
Barcroft, J. F. et al. Fertility treatment and cancers-the eternal conundrum: a systematic review and meta-analysis. Hum. Reprod. 36, 1093–1107 (2021).
Lerner-Geva, L. et al. Subfertility, use of fertility treatments and BRCA mutation status and the risk of ovarian cancer. Arch. Gynecol. Obstet. 306, 209–217 (2022).
Dixon-Suen, S. C. et al. The association between hysterectomy and ovarian cancer risk: a population-based record-linkage study. J. Natl Cancer Inst. 111, 1097–1103 (2019).
Khoja, L. et al. Endometriosis and menopausal hormone therapy impact the hysterectomy-ovarian cancer association. Gynecol. Oncol. 164, 195–201 (2022).
Ring, L. L. et al. Hysterectomy and risk of epithelial ovarian cancer by histologic type, endometriosis, and menopausal hormone therapy. Cancer Epidemiol. 84, 102359 (2023).
Taylor, J. A. et al. Association of hysterectomy and invasive epithelial ovarian and tubal cancer: a cohort study within UKCTOCS. Br. J. Obstet. Gynecol. 129, 110–118 (2022).
Sieh, W. et al. Tubal ligation and risk of ovarian cancer subtypes: a pooled analysis of case-control studies. Int. J. Epidemiol. 42, 579–589 (2013).
Collaborative Group on Epidemiological Studies of Ovarian Cancer et al. Ovarian cancer and oral contraceptives: collaborative reanalysis of data from 45 epidemiological studies including 23,257 women with ovarian cancer and 87,303 controls. Lancet 371, 303–314 (2008).
Moorman, P. G. et al. Reproductive factors and ovarian cancer risk in African-American women. Ann. Epidemiol. 26, 654–662 (2016).
Sarink, D. et al. Racial/ethnic differences in ovarian cancer risk: results from the multiethnic cohort study. Cancer Epidemiol. Biomark. Prev. 29, 2019–2025 (2020).
Schrijver, L. H. et al. Oral contraceptive use and ovarian cancer risk for BRCA1/2 mutation carriers: an international cohort study. Am. J. Obstet. Gynecol. 225, 51.e1–51.e17 (2021).
Xia, Y. Y. et al. Contraceptive use and the risk of ovarian cancer among women with a BRCA1 or BRCA2 mutation. Gynecol. Oncol. 164, 514–521 (2022).
van Bommel, M. H. D. et al. Contraceptives and cancer risks in BRCA1/2 pathogenic variant carriers: a systematic review and meta-analysis. Hum. Reprod. Update 29, 197–217 (2023).
Shafrir, A. L. et al. A prospective cohort study of oral contraceptive use and ovarian cancer among women in the United States born from 1947 to 1964. Cancer Causes Control. 28, 371–383 (2017).
Iversen, L. et al. Association between contemporary hormonal contraception and ovarian cancer in women of reproductive age in Denmark: prospective, nationwide cohort study. Br. Med. J. 362, k3609 (2018).
Haakenstad, A. et al. Measuring contraceptive method mix, prevalence, and demand satisfied by age and marital status in 204 countries and territories, 1970-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 400, 295–327 (2022).
Balayla, J., Gil, Y., Lasry, A. & Mitric, C. Ever-use of the intra-uterine device and the risk of ovarian cancer. J. Obstet. Gynaecol. 41, 848–853 (2021).
Phung, M. T. et al. Depot-medroxyprogesterone acetate use is associated with decreased risk of ovarian cancer: the mounting evidence of a protective role of progestins. Cancer Epidemiol. Biomark. Prev. 30, 927–935 (2021).
Faber, M. T. et al. Oral contraceptive use and impact of cumulative intake of estrogen and progestin on risk of ovarian cancer. Cancer Causes Control. 24, 2197–2206 (2013).
Collaborative Group on Epidemiological Studies of Ovarian Cancer et al. Menopausal hormone use and ovarian cancer risk: individual participant meta-analysis of 52 epidemiological studies. Lancet 385, 1835–1842 (2015).
Pearce, C. L., Chung, K., Pike, M. C. & Wu, A. H. Increased ovarian cancer risk associated with menopausal estrogen therapy is reduced by adding a progestin. Cancer 115, 531–539 (2009).
Lee, A. W. et al. Estrogen plus progestin hormone therapy and ovarian cancer: a complicated relationship explored. Epidemiology 31, 402–408 (2020).
Fournier, A. et al. Use of menopausal hormone therapy and ovarian cancer risk in a French cohort study. J. Natl Cancer Inst. 115, 671–679 (2023).
Phung, M. T. et al. Effects of risk factors for ovarian cancer in women with and without endometriosis. Fertil. Steril. 118, 960–969 (2022).
Tsilidis, K. K. et al. Menopausal hormone therapy and risk of ovarian cancer in the European prospective investigation into cancer and nutrition. Cancer Causes Control. 22, 1075–1084 (2011).
Lokkegaard, E. C. L. & Morch, L. S. Tibolone and risk of gynecological hormone sensitive cancer. Int. J. Cancer 142, 2435–2440 (2018).
Yuk, J. S. & Kim, M. Effects of menopausal hormone therapy on the risk of ovarian cancer: health insurance database in South Korea-based cohort study. Menopause 30, 490–496 (2023).
Neven, P. et al. The effect of raloxifene on the incidence of ovarian cancer in postmenopausal women. Gynecol. Oncol. 85, 388–390 (2002).
Tuesley, K. M. et al. Nitrogen-based bisphosphonate use and ovarian cancer risk in women aged 50 years and older. J. Natl Cancer Inst. 114, 878–884 (2022).
Kvaskoff, M. et al. Endometriosis and cancer: a systematic review and meta-analysis. Hum. Reprod. Update 27, 393–420 (2020).
Harris, H. R. et al. Racial differences in the association of endometriosis and uterine leiomyomas with the risk of ovarian cancer. Obstet. Gynecol. 141, 1124–1138 (2023).
Gersekowski, K. et al. Folate intake and ovarian cancer risk among women with endometriosis: a case-control study from the Ovarian Cancer Association Consortium. Cancer Epidemiol. Biomark. Prev. 32, 1087–1096 (2023).
Harris, H. R. et al. Polycystic ovary syndrome, oligomenorrhea, and risk of ovarian cancer histotypes: evidence from the Ovarian Cancer Association Consortium. Cancer Epidemiol. Biomark. 27, 174–182 (2018).
Harris, H. R. et al. Association between genetically predicted polycystic ovary syndrome and ovarian cancer: a Mendelian randomization study. Int. J. Epidemiol. 48, 822–830 (2019).
Frandsen, C. L. B. et al. Risk of epithelial ovarian tumors among women with polycystic ovary syndrome: a nationwide population-based cohort study. Int. J. Cancer 153, 958–968 (2023).
Yin, W., Falconer, H., Yin, L., Xu, L. & Ye, W. Association between polycystic ovary syndrome and cancer risk. JAMA Oncol. 5, 106–107 (2019).
Rasmussen, C. B. et al. Pelvic inflammatory disease and the risk of ovarian cancer and borderline ovarian tumors: a pooled analysis of 13 case-control studies. Am. J. Epidemiol. 185, 8–20 (2017).
Stewart, L. M. et al. Risk of high-grade serous ovarian cancer associated with pelvic inflammatory disease, parity and breast cancer. Cancer Epidemiol. 55, 110–116 (2018).
Falconer, H., Yin, L., Salehi, S. & Altman, D. Association between pelvic inflammatory disease and subsequent salpingectomy on the risk for ovarian cancer. Eur. J. Cancer 145, 38–43 (2021).
Jonsson, S., Jonsson, H., Lundin, E., Haggstrom, C. & Idahl, A. Pelvic inflammatory disease and risk of epithelial ovarian cancer. A national population-based case-control study in Sweden. Am. J. Obstet. Gynecol. 230, 75.e1–75.e15 (2023).
Trabert, B. et al. Antibodies against Chlamydia trachomatis and ovarian cancer risk in two independent populations. J. Natl Cancer Inst. 111, 129–136 (2019).
Fortner, R. T. et al. Sexually transmitted infections and risk of epithelial ovarian cancer: results from the Nurses’ Health Studies. Br. J. Cancer 120, 855–860 (2019).
Idahl, A. et al. Serologic markers of Chlamydia trachomatis and other sexually transmitted infections and subsequent ovarian cancer risk: results from the EPIC cohort. Int. J. Cancer 147, 2042–2052 (2020).
Wang, L. H., Zhong, L., Xu, B., Chen, M. & Huang, H. X. Diabetes mellitus and the risk of ovarian cancer: a systematic review and meta-analysis of cohort and case-control studies. BMJ Open 10, e040137 (2020).
Saarela, K., Tuomilehto, J., Sund, R., Keskimäki, I. & Hartikainen, S. Cancer incidence among Finnish people with type 2 diabetes during 1989–2014. Eur. J. Epidemiol. 34, 259–265 (2019).
Yuan, S. et al. Is type 2 diabetes causally associated with cancer risk? evidence from a two-sample mendelian randomization study. Diabetes 69, 1588–1596 (2020).
Pearson-Stuttard, J. et al. Type 2 diabetes and cancer: an umbrella review of observational and mendelian randomization studies. Cancer Epidemiol. Biomark. Prev. 30, 1218–1228 (2021).
Urpilainen, E., Puistola, U., Boussios, S. & Karihtala, P. Metformin and ovarian cancer: the evidence. Ann. Transl. Med. 8, 1711 (2020).
Hurwitz, L. M. et al. Association of frequent aspirin use with ovarian cancer risk according to genetic susceptibility. JAMA Netw. Open 6, e230666 (2023).
Baandrup, L., Kjaer, S. K., Olsen, J. H., Dehlendorff, C. & Friis, S. Low-dose aspirin use and the risk of ovarian cancer in Denmark. Ann. Oncol. 26, 787–792 (2015).
Hurwitz, L. M. et al. Modification of the association between frequent aspirin use and ovarian cancer risk: a meta-analysis using individual-level data from two ovarian cancer consortia. J. Clin. Oncol. 40, 4207–4217 (2022).
Trabert, B. et al. Analgesic use and ovarian cancer risk: an analysis in the ovarian cancer cohort consortium. J. Natl Cancer Inst. 111, 137–145 (2019).
Zeleznik, O. A., Irvin, S. R., Samimi, G. & Trabert, B. The role of statins in the prevention of ovarian and endometrial cancers. Cancer Prev. Res. 16, 191–197 (2023).
Yarmolinsky, J. et al. Association between genetically proxied inhibition of HMG-CoA reductase and epithelial ovarian cancer. J. Am. Med. Assoc. 323, 646–655 (2020).
Tuesley, K. M. et al. Association between antihypertensive medicine use and risk of ovarian cancer in women aged 50 years and older. Cancer Epidemiol. 86, 102444 (2023).
Zhuang, Y. J. et al. The incidence risk of breast and gynecological cancer by antidepressant use: a systematic review and dose-response meta-analysis of epidemiological studies involving 160,727 patients. Front. Oncol. 12, 939636 (2022).
Lauby-Secretan, B. et al. Body fatness and cancer — viewpoint of the IARC Working Group. N. Engl. J. Med. 375, 794–798 (2016).
Dixon, S. C. et al. Adult body mass index and risk of ovarian cancer by subtype: a Mendelian randomization study. Int. J. Epidemiol. 45, 884–895 (2016).
Friedenreich, C. M., Ryder-Burbidge, C. & McNeil, J. Physical activity, obesity and sedentary behavior in cancer etiology: epidemiologic evidence and biologic mechanisms. Mol. Oncol. 15, 790–800 (2021).
Vithayathil, M. et al. Body size and composition and risk of site-specific cancers in the UK Biobank and large international consortia: a Mendelian randomisation study. PLoS Med. 18, e1003706 (2021).
Olsen, C. M. et al. Obesity and risk of ovarian cancer subtypes: evidence from the Ovarian Cancer Association Consortium. Endocr. Relat. Cancer 20, 251–262 (2013).
Aarestrup, J. et al. Childhood overweight, tallness, and growth increase risks of ovarian cancer. Cancer Epidemiol. Biomark. Prev. 28, 183–188 (2019).
Schauer, D. P. et al. Bariatric surgery and the risk of cancer in a large multisite cohort. Ann. Surg. 269, 95–101 (2019).
Cannioto, R. et al. Chronic recreational physical inactivity and epithelial ovarian cancer risk: evidence from the Ovarian Cancer Association Consortium. Cancer Epidemiol. Biomark. Prev. 25, 1114–1124 (2016).
McTiernan, A. et al. Physical activity in cancer prevention and survival: a systematic review. Med. Sci. Sports Exerc. 51, 1252–1261 (2019).
Biller, V. S. et al. Sedentary behaviour in relation to ovarian cancer risk: a systematic review and meta-analysis. Eur. J. Epidemiol. 36, 769–780 (2021).
Chen, J. W. et al. Genetic associations of leisure sedentary behaviors and the risk of 15 site-specific cancers: a Mendelian randomization study. Cancer Med. 12, 13623–13636 (2023).
Collaborative Group on Epidemiological Studies of Ovarian Cancer. Ovarian cancer and body size: individual participant meta-analysis including 25157 women with ovarian cancer from 47 epidemiological studies. PLoS Med. 9, e1001200 (2012).
Faber, M. T. et al. Cigarette smoking and risk of ovarian cancer: a pooled analysis of 21 case-control studies. Cancer Causes Control. 24, 989–1004 (2013).
Baron, J. A., Nichols, H. B., Anderson, C. & Safe, S. Cigarette smoking and estrogen-related cancer. Cancer Epidemiol. Biomark. Prev. 30, 1462–1471 (2021).
Ko, K. P. et al. The association between smoking and cancer incidence in BRCA1 and BRCA2 mutation carriers. Int. J. Cancer 142, 2263–2272 (2018).
Gersekowski, K. et al. Risk factors for ovarian cancer by BRCA status: a collaborative case-only analysis. Cancer Epidemiol. Biomark. Prev. https://doi.org/10.1158/1055-9965.EPI-23-0984 (2024).
Endogenous Hormones Breast Cancer Collaborative Group et al. Circulating sex hormones and breast cancer risk factors in postmenopausal women: reanalysis of 13 studies. Br. J. Cancer 105, 709–722 (2011).
Larsson, S. C. et al. Smoking, alcohol consumption, and cancer: a mendelian randomisation study in UK Biobank and international genetic consortia participants. PLoS Med. 17, e1003178 (2020).
Ong, J. S. et al. Association between coffee consumption and overall risk of being diagnosed with or dying from cancer among >300 000 UK Biobank participants in a large-scale Mendelian randomization study. Int. J. Epidemiol. 48, 1447–1456 (2019).
Yang, C. S., Wang, X., Lu, G. & Picinich, S. C. Cancer prevention by tea: animal studies, molecular mechanisms and human relevance. Nat. Rev. Cancer 9, 429–439 (2009).
Byrd, D. A. et al. Development and validation of novel dietary and lifestyle inflammation scores. J. Nutr. 149, 2206–2218 (2019).
Yang, J. et al. Dietary inflammatory index and ovarian cancer risk: a meta-analysis. Nutr. Cancer 74, 796–805 (2022).
Vojdeman, F. J. et al. Vitamin D levels and cancer incidence in 217,244 individuals from primary health care in Denmark. Int. J. Cancer 145, 338–346 (2019).
Keum, N., Lee, D. H., Greenwood, D. C., Manson, J. E. & Giovannucci, E. Vitamin D supplementation and total cancer incidence and mortality: a meta-analysis of randomized controlled trials. Ann. Oncol. 30, 733–743 (2019).
Ong, J. S. et al. A comprehensive re-assessment of the association between vitamin D and cancer susceptibility using Mendelian randomization. Nat. Commun. 12, 246 (2021).
Wentzensen, N. & O’Brien, K. M. Talc, body powder, and ovarian cancer: a summary of the epidemiologic evidence. Gynecol. Oncol. 163, 199–208 (2021).
O’Brien, K. M. et al. Association of powder use in the genital area with risk of ovarian cancer. J. Am. Med. Assoc. 323, 49–59 (2020).
Utada, M. et al. Radiation risk of ovarian cancer in atomic bomb survivors: 1958-2009. Radiat. Res. 195, 60–65 (2021).
Leung, L. et al. Shift work patterns, chronotype, and epithelial ovarian cancer risk. Cancer Epidemiol. Biomark. Prev. 28, 987–995 (2019).
Liang, X. et al. Sleep characteristics and risk of ovarian cancer among postmenopausal women. Cancer Prev. Res. 14, 55–64 (2021).
Nash, Z. & Menon, U. Ovarian cancer screening: current status and future directions. Best Pract. Res. Clin. Obstet. Gynaecol. 65, 32–45 (2020).
Naumann, R. W., Hughes, B. N., Brown, J., Drury, L. K. & Herzog, T. J. The impact of opportunistic salpingectomy on ovarian cancer mortality and healthcare costs: a call for universal insurance coverage. Am. J. Obstet. Gynecol. 225, 397.e391–397.e6 (2021).
Idahl, A., Darelius, A., Sundfeldt, K., Palsson, M. & Strandell, A. Hysterectomy and opportunistic salpingectomy (HOPPSA): study protocol for a register-based randomized controlled trial. Trials 20, 10 (2019).
Steenbeek, M. P. et al. TUBectomy with delayed oophorectomy as an alternative to risk-reducing salpingo-oophorectomy in high-risk women to assess the safety of prevention: the TUBA-WISP II study protocol. Int. J. Gynecol. Cancer 33, 982–987 (2023).
Huh, W. et al. NRG-CC008: a nonrandomized prospective clinical trial comparing the non-inferiority of salpingectomy to salpingo-oophorectomy to reduce the risk of ovarian cancer among BRCA1 carriers [SOROCk]. J. Clin. Oncol. 60, https://doi.org/10.1200/JCO.2022.40.16_suppl.TPS106 (2022).
Evans, O., Gaba, F. & Manchanda, R. Population-based genetic testing for women’s cancer prevention. Best Pract. Res. Clin. Obstet. Gynaecol. 65, 139–153 (2020).
Alsop, K. et al. BRCA mutation frequency and patterns of treatment response in BRCA mutation-positive women with ovarian cancer: a report from the Australian Ovarian Cancer Study Group. J. Clin. Oncol. 30, 2654–2663 (2012).
Konstantinopoulos, P. A. et al. Germline and somatic tumor testing in epithelial ovarian cancer: ASCO guideline. J. Clin. Oncol. 38, 1222–1245 (2020).
Samimi, G. et al. Traceback: a proposed framework to increase identification and genetic counseling of BRCA1 and BRCA2 mutation carriers through family-based outreach. J. Clin. Oncol. 35, 2329–2337 (2017).
Brown, K. F. et al. The fraction of cancer attributable to modifiable risk factors in England, Wales, Scotland, Northern Ireland, and the United Kingdom in 2015. Br. J. Cancer 118, 1130–1141 (2018).
Jordan, S. J. et al. Cancers in Australia in 2010 attributable to total breastfeeding durations of 12 months or less by parous women. Aust. N. Z. J. Public Health 39, 418–421 (2015).
ClinicalTrials.gov. US National Library of Medicine https://clinicaltrials.gov/study/NCT03480776 (2023).
Appiah, D., Nwabuo, C. C., Ebong, I. A., Wellons, M. F. & Winters, S. J. Trends in age at natural menopause and reproductive life span among US women, 1959-2018. J. Am. Med. Assoc. 325, 1328–1330 (2021).
Cheng, H. et al. Global trends in total fertility rate and its relation to national wealth, life expectancy and female education. BMC Public Health 22, 1346 (2022).
Boutari, C. & Mantzoros, C. S. A 2022 update on the epidemiology of obesity and a call to action: as its twin COVID-19 pandemic appears to be receding, the obesity and dysmetabolism pandemic continues to rage on. Metabolism 133, 155217 (2022).
Kurman, R., Carcangiu, M., Herrington, C. & Young, R. WHO Classification of Tumours. Female Reproductive Organs (IARC, 2014).
Surveillance Epidemiology and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: Incidence — SEER Research Plus Data with Delay-Adjustment, 17 Registries, Malignant Only, Nov 2022 Sub (2000-2020) — Linked To County Attributes — Total U.S., 1969-2021 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, released April 2023, based on the November 2022 submission (accessed 2023).
Australian Institute of Health and Welfare (AIHW). Cancer Data in Australia https://www.aihw.gov.au/reports/cancer/cancer-data-in-australia/ (2023).
Larønningen, S. et al. NORDCAN: Cancer Incidence, Mortality, Prevalence and Survival in the Nordic Countries, Version 9.3 (02.10.2023). Association of the Nordic Cancer Registries. Cancer Registry of Norway. Available from: https://nordcan.iarc.fr/, (accessed 22 October 2023).
Rosenberg, P. S., Check, D. P. & Anderson, W. F. A web tool for age-period-cohort analysis of cancer incidence and mortality rates. Cancer Epidemiol. Biomark. Prev. 23, 2296–2302 (2014).
The US National Cancer Institute. Site Recode ICD-O-3 2023 Revision Expanded Definition https://seer.cancer.gov/siterecode/icdo3_2023_expanded/ (2024).
WHO Classification of Tumours Editorial Board. World Health Organization Classification of Female Genital Tumours. 5th Edition (IARC Press, 2020).
McCluggage, W. G., Hirschowitz, L., Gilks, C. B., Wilkinson, N. & Singh, N. The fallopian tube origin and primary site assignment in extrauterine high-grade serous carcinoma: findings of a survey of pathologists and clinicians. Int. J. Gynecol. Pathol. 36, 230–239 (2017).
McCluggage, W. G. Progress in the pathological arena of gynecological cancers. Int. J. Gynaecol. Obstet. 155, 107–114 (2021).
Cancer Research UK. Ovarian Cancer Incidence Statistics https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/ovarian-cancer/incidence#collapseTwo (2024).
National Cancer Institute (NCI). Cancer Stat Facts: Ovarian Cancer. https://seer.cancer.gov/statfacts/html/ovary.html (accessed 31 January 2024).
Global Burden of Disease Cancer Collaboration et al. Cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life years for 29 cancer groups from 2010 to 2019: a systematic analysis for the Global Burden of Disease Study 2019. JAMA Oncol. 8, 420–444 (2022).
Author information
Authors and Affiliations
Contributions
Both authors made a substantial contribution to all aspects of the preparation of this manuscript.
Corresponding author
Ethics declarations
Competing interests
P.M.W. has received speaker’s fees and research funding from AstraZeneca. S.J.J. declares no competing interests.
Peer review
Peer review information
Nature Reviews Clinical Oncology thanks the anonymous reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Webb, P.M., Jordan, S.J. Global epidemiology of epithelial ovarian cancer. Nat Rev Clin Oncol 21, 389–400 (2024). https://doi.org/10.1038/s41571-024-00881-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41571-024-00881-3