Abstract
Study design:
Prospective, single centre study.
Objectives:
Previous studies have suggested a relationship between stress reaction and elevated levels of prolactine. The aim of the present study was to investigate if there was a relationship between s-prolactine and menstrual cycle status following spinal cord injury (SCI).
Setting:
Spinal Cord Injury Unit, Göteborg, Sweden.
Methods:
S-prolactine and menstrual cycle status were investigated in 16 consecutive women with SCI, treated at the SCI Unit, Sahlgrens University Hospital, Göteborg, Sweden. Level of injury ranged from C1 to L5, ASIA A–D. Mean age at injury was 45 years (range 20–79).
Results:
S-Prolactine showed a mean value of 741 mIU/l (standard deviation (s.d.): 625; 95% confidence interval (CI): 435–1788 mIU/l, reference value <400 mIU/l). When dividing the group according to fertility status we found hyperprolactinaemia in the women who were in childbearing age (n=9): mean value 1050 mIU/l (s.d.: 678; 95% CI: 607–1493 mIU/ml), whereas it was normal in the group in menopause (n=7): mean value 343 mIU/l (s.d.: 185, 95% CI: 206–480 mIU/l) (P<0.01 when comparing groups). The group that developed amenorrhoea showed the highest values of s-prolactine. All values but one was normalised 3–6 months later.
Conclusion:
Amenorrhoea following SCI is correlated to level of s-prolactine. We found no correlation between level of s-prolactine and level or degree of injury.
Similar content being viewed by others
Introduction
Women sustaining spinal cord injury (SCI) have historically represented a small percentage of spinal cord injured persons and data from the Model SCI systems indicate that less than 20% are women.1 However our own incidence at the SCI Unit in Göteborg shows that the proportion of women increases and today reaches 30% of the injured population. This increasing incidence of SCI in women makes it more important to investigate the gender-specific effect of SCI in women. Examples of complications affecting women as amenorrhoea and galactorrhoea (spontaneous flow of milk from the nipple) have been reported in the acute situation following SCI,2, 3 and may raise the suspicion of concussion of the pituitary stalk, pregnancy or hormonal disturbance.
The biological responses to trauma are complex and long-term effects of trauma are visualized in the neurochemical responses including the catecholamine response and the duration and extent of cortisol response.4 Other endocrine alterations have been reported. In one study, a few SCI women were reported to exhibit elevated prolactine values in chronic stage (mean 7.5 years after injury).2 It has been reported that prolactine levels increase during some kinds of psychosocial stress5, 6 and it has been proposed that prolactine is important in the process of coping with stress and traumatic experience.6 Hyperprolactinaemia can cause galactorrhoea,3 and one paper reported four cases of galactorrhoea and hyperprolactinaemia in SCI women.7 The authors suggested a relationship with prescribed medications.7 Little is known about the prolactine response following acute SCI in women. Furthermore, since it is not known whether the prolactine levels differ according to age, we were interested in the prolactine level in all injured SCI women. Against this background we decided to incorporate analysis of prolactine in all newly spinal cord injured women. This was performed with the informed consent of the investigated women.
The aim of this study was to investigate whether there are elevated levels of prolactine in women in the acute phase of a spinal cord lesion and if there exist a relationship between prolactine and pattern of menstruation following SCI.
Materials and methods
Subjects
The study group compromised 16 consecutive new spinal cord injured women treated at our unit in the years 2001–2004. Mean age at injury was 45 years (range 20–79 years). Thirteen suffered from a traumatic origin of SCI and three from a non-traumatic. The level of injury varied from C1 to L5. For detailed patient characteristics see Table 1. Patients are normally admitted to the SCI unit directly from the accident. In this population there was some delay due to requirement of intensive care or due to referral from other hospitals or even other countries. Blood samples were analysed for s-prolactine when the patients arrived in our unit in mean 30 days after injury. When we found elevated values, we made a second investigation 3–6 months later. Two women with increased values were lost for follow-up.
Results
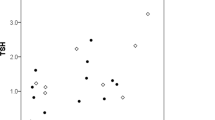
The mean s-prolactine value was 741 mIU/l (standard deviation (s.d.): 625; 95% confidence interval (CI): 435–1788 mIU/l) at first investigation (reference value <400 mIU/l). In nine women, who exhibited elevated s-prolactine in the first sample, a second investigation was carried out. All values but one was normal or slightly elevated at the second investigation, mean value was 428 mIU/l (s.d.: 244; 95% CI: 269–587 mIU/ml; P<0.01) (see Figure 1). When dividing the women according to fertility status we found that all women who were in menopause (n=7) showed normal or only slightly elevated values (mean value 343 mIU/l, s.d.: 185, 95% CI: 206–480 mIU/l), whereas in the childbearing age group (n=9) all but one showed elevated values. The mean value in the childbearing age group was 1050 mIU/l (s.d.: 678; 95% CI: 607–1493 mIU/ml). The difference between the groups was statistically significant, P<0.01. There was a negative correlation between age and s-prolactine values (r=−0.56), but we found no correlation to level or degree of injury. Three women had normal menstruation after injury and only slightly elevated values of s-prolactine (282–558 mIU/l). Six of the women in the childbearing age suffered from amenorrhoea, the first 6 months after injury. The women with amenorrhoea displayed the highest level of s-prolactine (700–2300 mIU/l) without overlap to the group in menopause or to the group who displayed normal menstruation pattern following SCI (see Table 1 for individual values).
Discussion
The main finding in this study is that women who sustain SCI in childbearing age are at high risk to develop hyperprolactinaemia and that the hyperprolactinaemia is strongly associated with amenorrhoea. Previous reports have proposed that the high values of prolactine were due to concussion of the pituitary stalk.3 The lack of correlation between level of injury and level of prolactine in our study does not support that. A more probable explanation might be that the hyperprolactinaemia is part of the reaction following SCI. Previous studies have shown that stress and crises, where you are unable to influence the course of events, are linked to hyperprolactinaemia.5, 6 SCI has a profound effect on the total life of the injured. In the early phase following injury, the ability to take active part in the care and planning is reduced. However, as time and rehabilitation passes, the injured subject is involved actively in the daily activities and the responsibility is returned to the subject. It has been shown that interventions aimed to improve psychological adjustment and coping is successful in reducing depression and anxiety.8 It might be that it also may influence the neurochemical responses to trauma. However, we did not investigate the perception of stress in this group of women. This needs to be further investigated. It is also important to state that the prolactine values differed between women. There was no increase in the group in menopause and the levels in the childbearing age group were not uniformly increased. It seems as prolactine is not a general marker of stress reaction. Further studies with larger samples are needed to evaluate the role of prolactine in reaction to SCI.
A previous study has shown that women postpartum or pregnant at the time of the injury sometimes develop galactorrhoea in association with increased values of prolactine.3 Galactorrhoea was not found in our subjects and none of the subjects was pregnant or postpartum. However, the hyperprolactinaemia was not asymptomatic since it was accompanied by amenorrhoea. The condition is in line with what is reported in other trauma situation. A study of almost 200 patients suffering from acute musculoskeletal trauma showed that 25% suffered from oligomenorrhoea or amenorrhoea during a 6-month period following trauma.9 It might be assumed that an extensive trauma as SCI also could cause disturbances in other hormonal axes. It was not the scope of this study to clarify this but animal data suggest that this needs to be further investigated. Experimental thoracic SCI in rats showed that 44% showed disturbances in the oestrous cycle.10
In conclusion, it seems as the amenorrhoea following spinal cord injury is due to a transient increase in prolactine, presumably as part of the neurochemical response to the stressful situation. Whether there are other transient or persistent changes in the hormonal axes following SCI deserves further investigations, especially as some disturbances are possible to treat.
References
Stover SL, Fine PR . The epidemiology and economics of spinal cord injury. Paraplegia 1987; 25: 225–228.
Huang TS . The hypothalamus–pituitary–ovary and hypothalamus–pituitary thyroid axes in spinal cord-injured women. Metabolism 1996; 45: 718–722.
Berezin M, Ohry A, Shemesh Y, Zeilig G, Brooks ME . Hyperprolactinaemia, galactorrhoea and amenorrhoea in women with a spinal cord injury. Gynecol Endocrinol 1989; 3: 159–163.
Desborough JP . The stress response to trauma and surgery. Br J Anaesth 2000; 85: 109–117.
Theorell T . Prolactine – a hormone that mirrors passiveness in crisis situations. Integr Physiol Behav Sci 1992; 27: 32–38.
Sivik T . The role of blood pressure, cortisole, and prolactine among soldiers injured in the 1991–1993 war in Croatia. Integr Physiol Behav Sci 1997; 32: 364–372.
Yarkony GM, Novick AK, Roth EJ, Kirschner KL, Rayner S, Betts HB . Galactorrhoea: a complication of spinal cord injury. Arch Phys Med Rehabil 1992; 73: 878–880.
Kennedy P, Duff J, Evans M, Beedie A . Coping effectiveness training reduces depression and anxiety following traumatic spinal cord injuries. Br J Clin Psychol 2003; 42: 41–52.
To WW, Wong MW . The relationship of physical trauma and surgical stress to menstrual dysfunction. Aust NZ J Obstet Gyneaecol 2000; 40: 48–53.
Hubscher CH, Armstrong JE, Johnson JR . Effects of spinal cord injury on the rat estrous cycle. Brain Res 2006; 1100: 118–124.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rutberg, L., Fridén, B. & Karlsson, AK. Amenorrhoea in newly spinal cord injured women: an effect of hyperprolactinaemia?. Spinal Cord 46, 189–191 (2008). https://doi.org/10.1038/sj.sc.3102095
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102095