Abstract
Study design:
Case–control.
Objective:
Tetraplegic patients are subject to episodes of autonomic dysreflexia and postural hypotension. It is suggested that these patients sustain, in addition, unstable baseline blood pressure (BP) that is independent of symptoms and body position.
Methods:
BP monitoring was conducted in 10 tetraplegic patients, motor and sensory complete (American Spinal Injury Association (ASIA) A) (Group A), and five paraplegic at T8–T10 levels, ASIA A (Group B). A SpaceLabs automatically inflating pneumatic cuff recorded arm pressures at 10–30 min intervals in the daytime, sitting position and at 30 min intervals in the night-time, recumbent position. Group mean arterial pressure (MAP) and MAP standard deviation (MAP variation) for sitting and recumbent positions were compared.
Results:
Sitting the MAP for Group A was less than that of Group B; 87±9 versus 108±7 mmHg, P<0.01. However, MAP variability for Group A was greater than for Group B; 17±4 (20% of MAP) versus 13±2 mmHg (12% of MAP), P=0.04. In the recumbent position, the MAP for Group A was similar to that for Group B; 87±13 versus 97±7 mmHg, P=0.16. However, MAP variability for Group A remained higher than for Group B; 13±3 (20% of MAP) versus 8±2 mmHg (8% of MAP), P=0.02.
Conclusion:
Tetraplegic patients demonstrate unstable BP in either the sitting or recumbent position compared with low thoracic paraplegic patients.
Similar content being viewed by others
Introduction
Unstable blood pressure (BP) in the spinal cord injury (SCI) patient manifests as autonomic dysreflexia – a reaction characterized by headache, facial perfusion, risk of stroke, and extreme elevation of BP1, 2, 3 and postural hypotension (PH) – characterized by disturbances of vision and consciousness, dyspnea and neck pain, and failure to maintain BPs on sitting up.4, 5, 6 Both of these responses are clinically recognized in patients with the higher, more extensive spinal cord lesions.3, 4 It is reasonable to suspect that BP is unstable subclinically as well in the tetraplegic patient. This expectation is supported by the unstable cutaneous blood flow recently demonstrated in asymptomatic tetraplegic patients.7 It is also relevant to note that resting instability of BP has been found in some non-SCI patients with autonomic impairment and PH.8 Still, some physicians treat tetraplegic patients on the basis of very few BP recordings. It would therefore be useful to test the baseline BP stability of the tetraplegic patient by repeated recordings in both the sitting and recumbent positions.
Methods
Subjects
Automated, ambulatory BP recordings were carried out in SCI patients at this institution in 1993 and 1994. The subjects were not acutely ill or bedridden and had been chosen by their willingness to wear the monitoring apparatus. The stored records of these recordings were retrieved and reviewed as a retrospective study. From this cohort the BP records of patients who were neurologically complete (American Spinal Injury Association (ASIA) A) in their paralysis at the cervical (Group A) or low thoracic (Group B) levels and whose surveys were technically satisfactory were chosen. It was recognized that numerous variables, which could have affected BP stability in individuals – use of caffeine, psychological or physical stress, spasticity, and antispastic medications were not identified in this retrospective review. Abdominal binders, elastic stockings, and mineralocorticoids were seldom used to support BP at this institution. Sympathomimetic amines were used intermittently as needed, however. Such support on the day of BP monitoring was not determined. Also, the administration of long acting antihypertensive medication in the monitored subjects could not be ruled out in this review. The selected patients were described by cause of paralysis, age, and duration of paralysis at the time of monitoring.
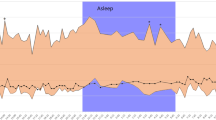
Blood pressure
BP monitoring had been conducted by the application of a pneumatic cuff with a microphone, a programmable air pump, and a solid-state recorder (Spacelabs Model 90207, Hospeq Inc., Miami, FL, USA) to the subject's arm. The monitoring was begun in the daytime with the patient in the sitting position. BP was recorded at 10–30 min intervals during the day while the patient was sitting in his wheelchair and changed to 30 min intervals in the recumbent position after the subject had transferred to bed for the night. Monitoring duration was generally 24 h, but night-time monitoring was not consistently carried out because the apparatus interrupted of sleep in some patients.
After recording, the BP readings were transferred to an electronic database for data compression and statistical description, using SpaceLabs software. For each patient the average sitting (daytime) and recumbent (night-time) systolic (SBP), diastolic (DBP), and mean arterial pressure (MAP) with standard deviations (SD) were calculated. The data were then divided between Group A and Group B. The mean SBP, DBP, and MAP for the groups were calculated. The mean SD for the individuals in each group were calculated for SBP, DBP, and MAP. The mean SD for these modalities for each group was called the variability of the group SBP, DBP, and MAP as it applied.
Group comparisons
Comparisons were made between the groups in the sitting and recumbent position for SBP, DBP, MAP and the variations of these modalities (the average of the individual SDs in each group). Comparisons were assessed by Student's t-test, using the software Primer of Biostatistics.9
Results
In all, 15 technically satisfactory recordings of patients with motor and sensory complete lesions were found, 10 classified as Group A and 5 as Group B. The patients in these groups were similar for age and duration of paralysis, although dissimilar for medical complications, Table 1.
Group A SBP, DBP, and MAP in the daytime, sitting position were lower than those of Group B, but Group A variabilities of the DBP and MAP were greater than those of Group B, Table 2. Group A night-time, recumbent SBP, DBP, and MAP were not lower than those of Group B; but their variabilities remained greater, Table 3.
Discussion
BP in the tetraplegic patient is unstable relative to that of low thoracic paraplegia. The BP variability of the tetraplegic patient was about 20 percent of each BP parameter in the sitting position, somewhat less in the recumbent. This variability was decisively greater than that of low paraplegia. As BP reflects the sum of microvascular blood flows in the various parts of the body and as microvascular variability of the skin has been demonstrated in tetraplegic patients, the observed BP variability associated with higher lesions was expected.7
Traumatic lesions of the cervical spinal cord10, 11 sever the sympathetic tracts descending from higher centers via the somatic corticospinal tracts and interrupt their distribution via the intermediolateral cell column of the thoracic spinal cord.12, 13 The healing of the cord lesions, which includes neuronal sprouting, fails to restore the original descending and ascending sympathetic integrity, and the usual modulation of BP through central control remains impaired.14 Baseline BP variability is plausible because central modulation is interrupted.
Neurochemical mechanisms of BP control may contribute to the observed instability. The blood levels of norepinephrine (NE) are low in tetraplegic patients, yet NE receptors become hypersensitive. Thus a BP elevation can be achieved in tetraplegic patients with less NE than is required in able-bodied controls.15, 16 This sensitivity is exploited in SCI patients with PH whose response to midodrine, a sympathomimetic amine, is prompt and greater than in controls.17, 18 It is suggested that subtle noxious stimuli, such as skin pressure or visceral activity that can trigger autonomic dysreflexia, may frequently release small doses of the short-lived NE to account for subclinical BP oscillations.19
An effect of position on this instability was found. Recumbent blood MAP variability was reduced in both the tetraplegic and the low thoracic paraplegic patients, although the greater instability of the tetraplegic BP was maintained. The general reduction in variability might be explained by the more even distribution of the stress of gravity and a relief of pressure points in recumbency. Thus noxious stimuli that trigger autonomic dysreflexia subclinically are reduced. Reduction in BP instability could not be explained by a supramedullary effect of sleep since the connection between the sleep centers of the medulla and the vasomotor system of the spinal cord is lost in tetraplegic patients.20
The average daytime, sitting BP in the tetraplegic patient was lower than that of the low thoracic paraplegic patient. A progressive reduction in BP with higher spinal cord lesions has been described.21 The low resting BP is also consistent with the reduced left ventricular size noted in tetraplegic patients.22 And although night-time, recumbent BPs were similar to those of paraplegia, this was only because the paraplegic BP diminished with sleep and the tetraplegic pressure did not. (The typical tetraplegic patient sleeps with his head elevated so that average night-time BP recordings may be spuriously low. A recent survey of bed positions at night in a resident care facility showed 10 degrees or more elevation in 11 of 15 patients who were motor complete tetraplegic but 0 of 5 who were paraplegic at the T10 level or lower, P=0.008.) This failure of the tetraplegic BP to diminish with sleep has been observed before.20
A possible limitation of this study is the number of the posturally hypotensive patients included in the survey. However, BP variability did not differ between patients with and without a history of PH. (The five tetraplegic patients with history of PH were compared with the five without. The daytime MAP and MAP variabilities were 86 and 9.7 versus 75 and 14.8 mmHg, P=0.47 and 0.71, respectively.) The effect of ephedrine, which may have been used by some patients, was not tested. The use of antispastics, tobacco and caffeine was not known for the patients surveyed, and these substances may have affected BP variability.23, 24 The use of antihypertensive medication in the paraplegic patients was not known. Conceivable inadvertent movement of the BP transducer from its position on the arm might have accounted for the variability noted. However, there is less chance for movement of the arms in the tetraplegic patients, the group with the greater variability. These uncertainties could be addressed in a prospective study.
For clinical purposes it may be useful to recognize the BP of the tetraplegic patient as relatively low and unstable. As such, an effect on organ perfusion might be expected. The function of the kidney, characterized by large annual differences in renal perfusion, measured over a short exposure to a tracer,25 is a case in point. The resistance of pressure-bearing skin to necrosis might vary.26 Hyper- or hypotensive readings may not persist in a given individual. BP monitoring should precede therapeutic decisions.
Conclusion
The tetraplegic patient, motor and sensory complete, sustains a BP that is lower and less stable than that of the low thoracic paraplegic patient, motor and sensory complete. This instability might alter organ function or reserve. It also suggests caution in the interpretation of a casual BP reading as an indication for the use of vasoactive medications.
References
Guttmann L, Whitteridge D . Effects of bladder distension on autonomic mechanisms after spinal cord injury. Brain 1947; 70: 361–404.
Thompson CE, Witham AC . Paroxysmal hypertension in spinal cord injuries. N Engl J Med 1948; 239: 291–294.
Krassioukov AV, Furlan JC, Fehlings MG . Autonomic dysreflexia in acute spinal cord injury: an under-recognized clinical entity. J Neurotrauma 2003; 20: 707–716.
Frisbie JH, Steele DJR . Postural hypotension and abnormalities of salt and water metabolism in myelopathy patients. Spinal Cord 1997; 35: 303–307.
Cariga P, Ahmed S, Mathias CJ, Gardner BP . The prevalence and association of neck (coat-hanger) pain and orthostatic (postural) hypotension in human spinal cord injury. Spinal Cord 2002; 40: 77–82.
Houtman S, Oeseburg B, Hughson RL, Hopman MT . Sympathetic nervous system activity and cardiovascular homeostasis during head-up tilt in patients with spinal cord injuries. Clin Autonom Res 2000; 10: 207–212.
Frisbie JH . Microvascular instability in tetraplegic patients: preliminary observations. Spinal Cord 2004; 42: 290–293.
Niarchos AP, Margini F, Tarazi RC, Bravo EL . Mechanisms of spontaneous supine blood pressure variations in chronic autonomic insufficiency. Am J Med 1978; 65: 547–552.
Glantz SA . Primer of Biostatistics, 4th edn, McGraw Hill: New York, NY 1997.
Wolman L . The disturbance of circulation in traumatic paraplegic in acute and late stages: a pathological review. Paraplegia 1964; 2: 213–226.
Wozniewicz B, Filipowiz K, Swiderska SK, Deraka K . Pathophysiological mechanism of traumatic cavitation of the spinal cord. Paraplegia 1983; 21: 312–317.
Coote JH, Macleod VH . The spinal route of sympatho-inhibitory pathways descending from the medulla oblongata. Pflugers Arch 1975; 359: 335–347.
Curt A, Weinhardt C, Dietz V . Significance of sympathetic skin response in the assessment of autonomic failure in patients with spinal cord injury. J Auton Nerv Syst 1996; 61: 175–180.
Llewellyn-Smith IJ, Weaver LC . Changes in synaptic inputs to sympathetic preganglionic neurons after spinal cord injury. J Comp Neurol 2001; 435: 226–240.
Mathias CJ, Frankel HL, Christensen NF, Spalding JMK . Enhanced pressor response to noradrenaline in patients with cervical spinal cord transection. Brain 1976; 99: 757–770.
Krum H, Louis WJ, Brown DJ, Howes LG . Pressor dose responses and baroreflex sensitivity in quadriplegic spinal cord injury patients. J Hypertens 1992; 10: 245–250.
Mukand J, Karlin L, Barrs K, Lublin P . Midodrine for the management of orthostatic hypotension in patients with spinal cord injury: a case report. Arch Phys Med Rehabil 2001; 82: 694–696.
Senard JM, Arias A, Berlan M, Tran MA, Rascol A, Montastruc JL . Pharmacological evidence of alpha 1- and alpha 2-adrenergic supersensitivity in orthostatic hypotension due to spinal cord injury: a case report. Eur J Clin Pharmacol 1991; 41: 593–596.
Karlsson AK, Friberg P, Lonnroth P, Sullivan L, Elam M . Regional sympathetic function in high spinal cord injury during mental stress and autonomic dysreflexia. Brain 1998; 121: 1711–1719.
Krum H, Louis WJ, Brown DJ, Jackman GP, Howes LG . Diurnal blood pressure variation in quadriplegic chronic spinal cord injury patients. Clin Sci 1991; 80: 272–276.
Frankel HL, Michaelis LS, Golding DR, Beral V . The blood pressure in paraplegia. Paraplegia 1972; 10: 193–300.
Eysmann SB, Douglas PS, Katz SE, Sarkarati M, Wei JY . Left ventricular mass and diastolic filling patterns in quadriplegia and implications for effects of normal aging on the heart. Am J Cardiol 1995; 75: 201–203.
Okuno T, Sugiyama T, Tominaga M, Kojima S, Ikeda T . Effects of caffeine on microcirculation of the human ocular fundus. Jpn J Ophthalmol 2002; 46: 170–176.
Monfrecola G, Riccio G, Savarese C, Posteraro G, Procaccini EM . The acute effect of smoking on cutaneous microcirculation blood flow in habitual smokers and nonsmokers. Dermatology 1998; 197: 115–118.
Kuhlemeier KV, Huang CT, DeVivo MJ, Lloyd LK . Year-to-year changes in effective renal plasma flow in asymptomatic spinal cord injury patients. Urology 1986; 28: 270–274.
Schubert V, Schubert PA, Breit G, Intaglietta M . Analysis of arterial flowmotion in spinal cord injured and elderly subjects in an area at risk for the development of pressure sores. Paraplegia 1995; 33: 387–397.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Frisbie, J. Unstable baseline blood pressure in chronic tetraplegia. Spinal Cord 45, 92–95 (2007). https://doi.org/10.1038/sj.sc.3101920
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101920
Keywords
This article is cited by
-
Poor specificity of National Early Warning Score (NEWS) in spinal cord injuries (SCI) population: a retrospective cohort study
Spinal Cord (2020)
-
Relationship between autonomic cardiovascular control and obstructive sleep apnoea in persons with spinal cord injury: a retrospective study
Spinal Cord Series and Cases (2018)
-
Use of ambulatory blood pressure monitoring in adolescents with SCI: a case series
Spinal Cord Series and Cases (2017)
-
The prevalence of pulmonary embolism in chronically paralyzed subjects: a review of available evidence
Spinal Cord (2012)