Abstract
Objectives:
To investigate (1) the characteristics of shoulder pain following discharge from rehabilitation for tetraplegia, (2) the relationship between pain and any associated risk factors and (3) the relationship between pain and functional activities, and pain and quality of life.
Design:
Longitudinal study.
Setting:
Spinal Injuries Unit, Australia.
Methods:
Participants (n=27) were surveyed between 2 and 4 years postinjury. Prospective data on shoulder pain during rehabilitation had been collected previously and allowed comparison with the follow-up data. Data collected included pain intensity and quality, the Wheelchair User's Shoulder Pain Index (WUSPI) and perceived effect of pain on quality of life.
Results:
Shoulder pain prevalence was 70%. Pain was associated with discharge motor level of C6–T1 (P=0.003). Pain was most commonly located in the shoulder joint. Pain was primarily aggravated by movement and cold weather and relieved by rest. The most painful activity was lifting an object from overhead. Quality of life was affected by pain in 68.4% of participants.
Conclusion:
Shoulder pain is common following rehabilitation for tetraplegia and is associated with injury level. Pain is reported during daily tasks and adversely affects quality of life. Areas for further research are identified.
Similar content being viewed by others
Introduction
Shoulder pain following tetraplegia is a common problem. Prevalence rates of 46–59% have been reported at least 1 year postinjury.1, 2, 3 The degree of functional independence that a person with tetraplegia can achieve is influenced by shoulder musculoskeletal integrity.4, 5, 6 Shoulder pain may therefore be functionally and economically equivalent to a higher lesion level.2
A previous study found that 85% of people with acute tetraplegia have shoulder pain during rehabilitation.7 There is a lack of information on the period shortly after rehabilitation as previous studies have included participants with widely varying durations of tetraplegia.1, 2, 3 Little is known about factors which may predispose to the development of pain and therefore, who should be targeted for early intervention. Pain may have a detrimental effect on functional performance and quality of life,6, 8 but little research has been conducted into this.
Previous authors have not found an association between the prevalence of shoulder pain and age1, 3 or level of injury (high versus low tetraplegia).3 Pain has been reported to disturb sleep and to increase with wheelchair propulsion, especially uphill or for prolonged periods1 and with upper extremity dressing, transfers and reaching.3 A number of studies have investigated the characteristics of pain following spinal cord injury (SCI)9, 10, 11 but there is a paucity of research specifically on the characteristics of shoulder pain following rehabilitation. Qualitative pain information may provide some insight into underlying mechanisms of pain.
This study aimed to (1) investigate whether there is a relationship between shoulder pain during rehabilitation and shoulder pain between 2 and 4 years after onset of tetraplegia, (2) describe the characteristics of shoulder pain after discharge, (3) identify factors which may predispose to the development of shoulder pain after discharge, (4) determine whether shoulder pain affects the performance of functional activities and (5) determine whether shoulder pain impacts on quality of life.
Methods
Participants
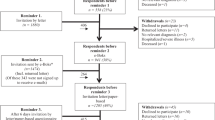
A survey was posted to all participants who participated in an earlier study of shoulder pain while they were undergoing inpatient rehabilitation in a Spinal Injuries Unit.7 Participants were previously allocated to one of four groups to describe pain during rehabilitation: pain-pain (pain on admission and on discharge), pain-no pain (pain on admission but not on discharge), no pain-pain (no pain on admission but pain on discharge) and no pain-no pain (no pain on admission or discharge). Subject selection criteria were previously described.7 The survey was sent between two and 4 years postinjury. A follow-up telephone call was made to participants who did not respond, offering them the opportunity to participate via telephone.
Measurements
Demographics
Demographic data collected included age, gender and details of SCI. Neurological function was assessed on admission and discharge from rehabilitation using the American Spinal Injury Association (ASIA) International Standards of Classification.12 This included motor level (most caudal segment with normal motor function) and sensory level (most caudal segment with normal sensory function). The ASIA impairment scale categorised participants as complete SCI (absence of motor and sensory function below the level of the lesion) or incomplete SCI (varying grades of motor and/or sensory function below the level of the lesion). ASIA scores were also calculated by adding up muscle testing grades for the key muscle group at each spinal level with higher ASIA scores indicating greater overall muscle function.
Pain
Participants were asked about pain onset and area. Pain intensity was recorded with the Numerical Rating Scale 101 (NRS-101),13 which quantifies the perceived level of pain intensity on a scale of 0 (no pain) to 100 (worst possible pain). This scale was selected as it is verbal and thus suited for a telephone interview. The McGill Pain Questionnaire (MPQ)14 was used to provide information on pain quality. This included verbal descriptors of pain, area of pain and aggravating and relieving factors. Pain rating index scores (PRI) were calculated for the sensory (PRIS), affective (PRIA), evaluative (PRIE) and miscellaneous (PRIM) categories as well as the overall total (PRIT).14
The Wheelchair User's Shoulder Pain Index (WUSPI) was used to measure pain during functional activities.15 This was adapted to a verbal scale using the NRS-101 instead of the visual analogue scale to enable the survey to be performed verbally. Participants rated the severity of their pain during 15 functional activities with 0 representing no pain and 100 representing worst possible pain for each activity. Not all participants performed all activities due to differences in functional ability unrelated to shoulder pain therefore the average WUSPI was calculated for each subject by dividing their total score by the number of activities performed.
Other
Participants were asked whether their shoulder pain affected their quality of life (QOL). A four-point scale was used with 1 representing ‘strongly disagree’, 2 ‘disagree’, 3 ‘agree’ and 4 ‘strongly agree’. Participants were asked to rate their independence for mobility, transfers and dressing. Information was also collected about any treatment received.
The data from the survey were linked to data obtained from the earlier study of pain and range of motion (ROM) during rehabilitation.7
Ethical approval was obtained from the Princess Alexandra Hospital and the University of Queensland Medical Research Ethics Committees.
Statistics
Descriptive statistics were used for pain prevalence and area. The relationships between pain presence on follow-up and neurological level, ASIA impairment scale, pain prevalence and pain groups during rehabilitation, QOL and functional level were assessed using Spearman's Rank Order Correlation test. Independent samples t-tests were used to test for differences between the pain and no pain groups for age, ASIA scores, WUSPI scores, pain intensity, MPQ total score and ROM during rehabilitation. Spearman's Rank Order Correlations were used to examine the relationship between QOL and pain intensity, WUSPI and MPQ totals. Owing to multiple comparisons, a significance level of P⩽0.01 was used to protect against Type 1 errors.
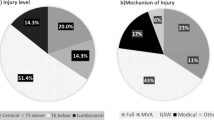
Results
Of the original 35 participants, 27 agreed to complete the survey. There was no significant difference between those who responded and those who did not with respect to any demographic variables or pain variables during rehabilitation (P>0.1). The average age of respondents was 42.5±19.9 (mean±SD) years with a range of 16–88 years. Of them, 20 were male. The effect of dominance could not be assessed as only four participants were left-handed.
In total, 19 participants (70%) reported pain on follow-up; 11 of the 19 reported bilateral pain, three had pain on the left only and five participants reported right side only. All participants with pain reported that pain onset commenced before or within 6 months of discharge.
Of the 10 participants in the previous study who reported pain on admission and discharge from rehabilitation, eight responded to the follow-up and all eight reported pain at the time of follow-up. Approximately 1/2 of the participants in each of the other groups reported pain on follow-up. Only two participants reported constant pain on discharge; therefore, the effect of this on pain prevalence at follow-up could not be assessed. The presence of pain on follow-up was not related to prevalence of pain on admission or discharge or pain group during rehabilitation (P>0.2). There was no relationship between the presence of pain on follow-up and pain intensity or MPQ total score on admission or discharge from rehabilitation (P>0.6).
Participants with a discharge motor level of C6–T1 (r=−0.545, P=0.003) were more likely to report pain on follow-up. There was no relationship between pain on follow-up and completeness of lesion (ASIA impairment scale) on admission or discharge or between pain on follow-up and sensory level on admission or discharge. Age was not significantly related to pain.
Range of motion for flexion, abduction and external rotation at 90° abduction as collected in the previous study7 was not significantly different between the pain and no pain groups.
Of the 19 participants with pain, 16 completed the MPQ. Average scores for each section of the MPQ are shown in Table 1. The percentage of participants who chose words from each category is presented in Table 2. Each category was selected by at least one subject. ‘Sharp’, ‘tight’, ‘nagging’ and ‘tender’ were selected by at least 50% of the participants with ‘aching’ and ‘hot’ chosen by 1/3 of participants.
Pain was located in the shoulder joint in 12 participants, the scapula in seven participants, the upper trapezius area in three participants and the upper arm in three participants. Six participants reported pain in more than one area. There was no association between neurological function (level or completeness of injury) and the side of pain or whether pain was bilateral or unilateral. The most common descriptors for each area of pain are presented in Table 3. Pain was primarily aggravated by movement and cold weather. Rest was the most commonly used method for pain relief followed by heat, stretching and massage.
Walking was the primary means of mobility for the majority of the group (n=14) followed by attendant-propelled or powerdrive wheelchair (n=9) with only four participants self-propelling a manual wheelchair. In all, 16 participants performed a standing transfer, five performed a seated transfer and 6 used a hoist. There was no significant difference in independence level between the pain and no pain groups for mobility or transfers. All participants with pain completed the WUSPI. Table 4 illustrates the average score for each item, the number of participants who performed each activity, the number of these with pain and the number with pain greater than 50 on the NRS, considered to be ‘moderate-severe pain’ for this study. There was a positive correlation between pain intensity and total WUSPI (r=0.723, P=0.000) and pain intensity and total MPQ score (r=0.625, P=0.01) on Spearman's correlation. Pain intensity and WUSPI total scores were not significantly related to independence level (P>0.2). Of the 19 participants with pain, 13 reported that their pain affected their QOL.
All participants except one sought treatment for their shoulder pain. Figure 1 shows the number of participants who chose each treatment and whether the treatments were reported to be helpful.
Discussion
The proportion of participants with pain (70%) is greater than previous studies (46–59%).1, 2, 3 This may be due to differences in inclusion criteria between the current subject group and previous groups. Other studies have included participants with a wide range of SCI duration (up to 48 years),1, 2, 3 whereas all participants in this study were between 2 and 4 years postinjury. Many of the current group were ASIA D (motor incomplete SCI), whereas others have either studied ASIA D as a separate group and included paraplegia8 or did not define completeness of injury.1, 2, 3 Half the current subject group walked as their primary means of mobility whereas others have specified minimum periods of wheelchair use1 or did not define mobility.2, 3, 8 Some studies have combined tetraplegia and paraplegia,3, 8, 16 however, it is difficult to evaluate these studies as there may be different factors contributing to pain such as neurological weakness of shoulder muscles, nerve root involvement and lack of trunk stability. Finally, some authors report on upper extremity pain in general with few specifics on the shoulder.2, 16, 17
All participants with shoulder pain reported that the pain started during rehabilitation or within 6 months of discharge. Previous studies have reported an incidence of pain in 20% of the group commencing within 1 year in a combined sample of tetraplegia and paraplegia3 and 53% reporting pain within 5 years.2 In comparison, Siddall11 failed to find a relationship between pain at 6 months and pain at 5 years in their survey of musculoskeletal pain, however, their study included areas of pain other than the shoulder. The difference in prevalence rates may be related to the differences between subject groups previously discussed. All participants without pain reported being pain-free within 6 months of discharge, which suggests that the time during and shortly after rehabilitation may be an important determinant of the likelihood of developing pain. Participants who had pain on both admission and discharge from rehabilitation continued to have pain on follow-up; however, the small numbers in this subgroup limits the generalisation of this finding.
Motor levels on discharge were related to pain. This conflicts with earlier reports,3, 8 however, the previous studies assessed injury level at the time of follow-up and one study was by participants' self-report of injury level3 which may be inaccurate. Level of injury may change with time causing difficulty comparing results between studies. Injury level in previous studies was broadly divided into C1–C4 and C5–T1. Muscle innervation and expected functional outcomes varies according to injury level so discrimination between injury levels may be important but this may also limit statistical significance due to small numbers of participants. Participants with a discharge level of C6–T1 were more likely to report shoulder pain on follow-up. People with lower injury levels, and therefore more upper limb movement may be more active and therefore more prone to developing pain of a musculoskeletal origin.6, 18
Most of the words available on the MPQ were used, which indicates the diversity of the pain experience. This may be due in part to the variety of probable causes of shoulder pain. ‘Tight’, ‘tender’, ‘sharp’ and ‘nagging’ were most commonly chosen. ‘Tender’ has been used to describe diverse conditions, such as trauma pain,19 cervicogenic headache,20 hyperalgesia20 and acute postoperative pain.21 It has previously been reported that the word ‘tight’ may be used to describe cervicogenic headaches, decreased joint mobility and increased muscle activity20 as well as musculoskeletal pain following SCI.9 The evaluative word ‘nagging’ was also attributed to musculoskeletal pain.9 ‘Aching’ was chosen by one-third of participants. Aching' may describe musculoskeletal pain,9, 22 but was found by Cardenas10 to describe both musculoskeletal and SCI pain (defined as neurologic pain below the lesion level in an area without normal sensation). ‘Tingling’ has been considered a descriptor for neuropathic pain9, 10, 22 and was not a common choice in this study. Words such as ‘hot’ and ‘burning’ may describe SCI pain more than musculoskeletal pain10 and these words may indicate a neuropathic component to some pain.
Shoulder joint pain was the most common area of pain and was variously described as ‘throbbing’, ‘sharp’, ‘aching’, ‘tight’ and ‘tender’. These words may describe or relate to trauma or inflammation to various structures within the shoulder joint or the capsule as they may describe pain of musculoskeletal origin.9, 18, 19, 22
Pain in the upper trapezius region was described as ‘sharp’, ‘pinching’, ‘pulling’, ‘hot’ and ‘tender’. Descriptors of heat may refer to neuropathic pain referred from the cervical spine.10, 23 Pain in this area may also be a result of muscle overactivity due to neurological weakness in other shoulder muscles and repetitive actions such as wheelchair propulsion. These biomechanical causes would be more likely in the later stages of SCI rather than acutely following injury.
The arm pain reported by participants may be referred from the neck or related to shoulder impingement.24 It was predominantly unilateral and was not related to level of neurological function. The descriptors of ‘shooting’, ‘stabbing’, ‘cramping’, ‘burning’ and ‘radiating’ suggest a neuropathic component.9, 10, 22
Scapula pain was described as ‘pinching’, ‘taut’, ‘sharp’, ‘dull’ and ‘tight’ as well as ‘exhausting’. Scapula pain may result from myofascial disorders,24 thoracic spine problems or be referred from spinal structures between C5 and T6.25, 24 Arm and scapula pain were the only areas in which a number of participants tended to use affective descriptors such as ‘tiring’, ‘exhausting’ and ‘troublesome’, which indicates different pain experiences to those with pain in other areas.
Overuse injuries from wheelchair propulsion and transfers have commonly been cited as a major cause of shoulder pain but this does not account for the high proportion of nonwheelchair users with pain. Poor proximal stability and scapular control may predispose the shoulder joint to pathology due to abnormal movement patterns.6, 26, 27 This poor muscle control may result from neurological impairment, pain and/or incorrect movement patterns. Pain was aggravated by movement and improved with rest, heat and stretching, indicative of musculoskeletal pain.23 Cold weather also worsened the pain suggestive of neuropathic pain with cold hyperalgesia.28 Further investigations need to be conducted to clarify these mechanisms and enable appropriate selection of treatment.
The majority of participants agreed that pain affected their QOL. This concurs with a previous study of self-reported general health.8
Total WUSPI correlated significantly with pain intensity. The most painful activity was lifting overhead. Activities such as sleeping, driving, pushing a wheelchair, transfers, putting on a t-shirt and work activities also scored highly as has been found by others.1, 3 Caution must be taken when interpreting some of these results due to the small number of participants who performed some of the activities (especially wheelchair skills). Overhead lifting did not score particularly highly in Curtis'1 study. It may be that the current participants, many of whom walk, may live primarily in an able-bodied person's environment requiring more overhead activities compared with a person in a wheelchair in a modified home.
All but one participant in this study had sought treatment for their pain in contrast to the study by Curtis'1 where the majority of participants did not. The patients in the current study were more recently injured and therefore more recently exposed to medical and other treatments while in hospital and may be more likely to seek help for pain. People with long-term SCI may be more likely to self-treat or to expect to have some pain and not seek treatment. The most popular treatments were physiotherapy, massage and heat. Positive responses to these modalities suggest a musculoskeletal component to pain, however, all patients continued to have pain despite treatment. This suggests that treatment may not have been sufficiently comprehensive or that pain mechanisms may be more complex and that a multifactorial approach may be needed.
Limitations
Small participant numbers, particularly in subgroups of pain and area of pain limit the ability to find statistically significant results and therefore limits generalisation. There was a high proportion of people who walk and relatively few participants who regularly performed activities such as seated transfers and wheelchair skills making it difficult to accurately assess the effect of pain on these activities. The WUSPI was adapted to enable it to be administered verbally, therefore we cannot compare absolute scores with other authors although the relative difficulty of an activity due to pain can still be compared. Questions have been raised about the factor structure of the MPQ29, 30 and overlap between subclasses.31, 32 At the time this study was commenced the MPQ was the most comprehensive, validated tool available to qualitatively describe pain. Information about specific pain qualities may be lost when only section totals are given so we have reported on individual subclasses. No investigative diagnostic tests were performed (eg ultrasound, MRI), which would have aided diagnosis of pain causes. A combination of diagnostic tests and pain characteristics may help to explain the pain mechanisms involved.
Conclusions
This is the first study to qualitatively describe shoulder pain following discharge from rehabilition following acute tetraplegia. Traditionally, shoulder pain after SCI has been partly blamed on shoulder joint weight bearing during transfers or use of walking aids, wheelchair propulsion and wheelchair posture. The results of this study indicate that a high proportion of people with SCI who do not use wheelchairs still complain of shoulder pain. Therefore, there must be other factors contributing to shoulder pain posttetraplegia. Future research needs to focus on identifying the relative contribution that these different factors may have in the development and continuation of shoulder pain. This will help to direct appropriate and effective prevention and management strategies.
References
Curtis K et al. Shoulder pain in wheelchair users with tetraplegia and paraplegia. Arch Phys Med Rehabil 1999; 80: 453–457.
Sie I et al. Upper extremity pain in the postrehabilitation spinal cord injured patient. Arch Phys Med Rehabil 1992; 73: 44–48.
Subbarao J, Klopfstein J, Turpin R . Prevalence and impact of wrist and shoulder pain in patients with spinal cord injury. J Spinal Cord Med 1995; 18: 9–13.
Campbell C, Koris M . Aetiologies of shoulder pain in cervical spinal cord injury. Clin Orthopaed Relat Res 1996; 322: 140–145.
MacKay-Lyons M . Shoulder pain in patients with acute quadriplegia. Physiother Canada 1994; 46: 255–258.
Silfverskiold J, Waters R . Shoulder pain and functional disability in spinal cord injured patients. Clin Orthopaed Relat Res 1991; 272: 141–145.
Salisbury S, Low Choy N, Nitz J . Shoulder pain, range of motion and functional motor skills after acute tetraplegia. Arch Phys Med Rehabil 2003; 84: 1480–1485.
Ballinger D, Rintala D, Hart K . The relation of shoulder pain and range of motion problems to functional limitations, disability and perceived health of men with spinal cord injury: a multifaceted longitudinal study. Arch Phys Med Rehabil 2000; 81: 1575–1581.
Dudgeon B et al. Describing pain with physical disability: narrative interviews and the McGill Pain Questionnaire. Arch Phys Med Rehabil 2005; 86: 109–115.
Cardenas D et al. Classification of chronic pain associated with spinal cord injuries. Arch Phys Med Rehabil 2002; 83: 1708–1714.
Siddall P et al. A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain 2003; 103: 249–257.
Maynard F et al. International standards for neurological and functional classification of spinal cord injury. Spinal Cord 1997; 35: 266–274.
Jensen M, Karoly P, Brauer S . The measurement of clinical pain intensity: a comparison of six methods. Pain 1986; 27: 117–126.
Melzack R . Pain measurement and assessment. Raven Press: New York 1983, pp 277–299.
Curtis K et al. Development of the wheelchair user's shoulder pain index. Paraplegia 1995; 33: 290–293.
Dalyan M, Cardenas D, Gerard B . Upper extremity pain after spinal cord injury. Spinal Cord 1999; 37: 191–195.
Turner J et al. Chronic pain associated with spinal cord injuries: a community survey. Arch Phys Med Rehabil 2001; 82: 501–508.
Miyahara M, Sleivart G, Gerrard D . The relationship of strength and muscle balance to shoulder pain and impingement syndrome in elite quadriplegic wheelchair rugby players. Int J Sports Med 1998; 19: 210–214.
Melzack R, Wall P, Ty T . Acute pain in an emergency clinic: latency of onset and descriptor patterns related to different injuries. Pain 1982; 14: 33–43.
Niere K . Pain descriptors used by headache patients presenting for physiotherapy. Physiotherapy 2002; 88: 409–415.
Fortin J, Schwartz-Barcott D, Rossi S . The post-operative pain experience. Clincal Nursing Research 1992; 1: 292–304.
Putzke J et al. Pain classification following spinal cord injury: the utility of verbal descriptors. Spinal Cord 2002; 40: 118–127.
Siddall P, Taylor D, Cousins M . Classification of pain following spinal cord injury. Spinal Cord 1997; 35: 69–75.
Haig S . Shoulder pathophysiology: rehabilitation and management. Aspen Publishers Inc.: Maryland 1996, pp 7–15.
Fukui S et al. Referred pain distribution of the cervical zygapophyseal joints and cervical dorsal rami. Pain 1996; 68: 79–83.
Burnham R et al. Shoulder pain in wheelchair athletes. Am J Sports Med 1993; 21: 238–242.
Burnham R, Curtis K, Reid D . Shoulder problems in the wheelchair athlete. In: Pettrone A (ed). Athletic Injuries of the Shoulder. McGraw-Hill Inc.: USA 1995, pp 375–381.
Lancelotta M, et al. Severity and duration of hyperalgesia in rat vaires with type of nerve lesion. Neurosurgery 2003; 53: 1200–1209.
Holroyd K et al. A multi-centre evaluation of the McGill Pain Questionnaire: results from more than 1700 chronic pain patients. Pain 1992; 48: 301–311.
Leavitt F et al. Affective and sensory dimensions of back pain. Pain 1978; 4: 273–281.
Fernandez E, Boyle G . Affective and evaluative descriptors of pain in the McGill Pain Questionnaire. J Pain 2001; 2: 318–325.
Toomey T, Gover V, Jones B . Site of pain: relationship to measures of pain description, behaviour and personality. Pain 1984; 19: 389–397.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Salisbury, S., Nitz, J. & Souvlis, T. Shoulder pain following tetraplegia: a follow-up study 2–4 years after injury. Spinal Cord 44, 723–728 (2006). https://doi.org/10.1038/sj.sc.3101908
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101908
Keywords
This article is cited by
-
ARbility: re-inviting older wheelchair users to in-store shopping via wearable augmented reality
Virtual Reality (2023)
-
The Danish Spinal Cord Injury Shoulder (DanSCIS) cohort: methodology and primary results
Spinal Cord (2021)
-
Subscapularis motor point block for spastic shoulders in patients with cervical cord injury
Spinal Cord (2009)