Abstract
Study design:
Clinical case report.
Objectives:
To present the first case of incomplete tetraplegic spinal cord injury (SCI) in which complex regional pain syndrome (CRPS) type I was present in all four of the patient's extremities.
Setting:
Ankara Physical Medicine and Rehabilitation Education and Research Hospital, Ankara, Turkey.
Methods:
A 49-year-old man with incomplete tetraplegia (American Spinal Injury Association (ASIA) C) was admitted to our clinic for rehabilitation. According to the patient's history, pain and edema began in his right foot 1½ months after his injury. After 10 days later the same symptoms appeared in his left foot as well. In the third week after pain and edema appeared in the right foot, these were also observed in both hands, markedly in the left.
Results:
Three-phase bone scan images supported a diagnosis of stage 3 CRPS type I in all four extremities. After the diagnosis was made, passive range of motion (PROM) exercises were started. Transcutaneous electrical nerve stimulation and whirlpool sessions were used for pain and edema control. Drug therapy included Calcitonin, Naproxen sodium and Amitriptyline. After 6 weeks of treatment, the patient's visual analog scale pain score had decreased to 38 mm from an initial score of 85 mm at the onset of the treatment, and PROM of wrists/hands, fingers and ankles had become full and painless.
Conclusion:
We conclude that CRPS type I might be more common in SCI than is usually suspected, and that tetraplegic patients should be carefully evaluated for the presence of CRPS type I in upper and lower extremities.
Similar content being viewed by others
Introduction
Pain is a frequent complication of spinal cord injury (SCI).1 The diagnosis and classification of pain following SCI are important for the patient's optimal participation in a rehabilitation program and achievement of self-care goals. Function-limiting pain occurs in 11–34% of SCI patients.2, 3 Neuropathic pain was formerly classified under names such as reflex sympathetic dystrophy (RSD) and causalgia, but according to the classification system proposed by the International Association for the Study of Pain (IASP), these are now both classified as complex regional pain syndromes (CRPS).4 CRPS type I, formerly known as RSD, is characterized by pain (usually excessive or prolonged), vasomotor and other autonomic disturbances, soft tissue swelling and trophic changes.2, 5 According to IASP criteria the characteristic features required to establish the diagnosis of CRPS type I are as follows: (1) the presence of an initiating noxious event or a cause of immobilization; (2) continuing pain, allodynia, or hyperalgesia with pain disproportionate to any inciting event; (3) evidence at some time of edema, changes in skin blood flow, or abnormal sudomotor activity in the region of the pain; and (4) the exclusion of medical conditions that would otherwise account for the degree of pain and dysfunction.6 Additionally, three-phase bone scan (TPBS) has been shown to be a useful adjunct in the diagnosis of CRPS type I.7
In the last decade, several authors have contributed to the increasing recognition that CRPS type I can follow cervical SCI. However, in the literature, there is no reported case of an SCI patient who has CRPS type I in both upper and lower extremities. Here we report the first case of incomplete tetraplegia in which CRPS type I occurred in all four extremities. Another objective here is to emphasize the importance of considering CRPS type I in the diagnosis of pain in SCI patients.
Case report
A 49-year-old man was admitted to our hospital for rehabilitation with the diagnosis of C7 incomplete tetraplegia (ASIA C). He had undergone Cloward anterior discectomy and fusion in a local hospital due to the dislocation and fracture of his C5–6 vertebrae, which had occurred 7½ months prior in a traffic accident.
According to the patient's history, pain and edema had started in his right foot 1½ months after the accident. After 10 days, the same symptoms appeared in his left foot as well. In the third week after pain and edema appeared in the right foot, these were also observed in both hands, markedly in the left. The patient described the pain as burning and throbbing. He also said he had insomnia because of the pain.
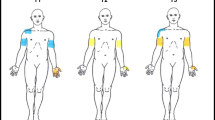
Physical examination at admission showed sensory and motor signs of incomplete C7 tetraplegia (ASIA C). All deep tendon reflexes were active bilaterally. The patient had edema in both hands and feet (Figure 1). Both lower extremities were cold. There were no trophic changes. Range of motion was limited in shoulders, wrists and ankles. Left and right lower extremities did not differ in diameter. Examinations performed for differential diagnosis included lower extremity venous Doppler ultrasonography and routine biochemistry (alkaline phosphatase, C-reactive protein, erythrocyte sedimentation rate and total blood count). All results were normal. Diffuse osteopenia was observed in bilateral anterior–posterior, hand–wrist and foot–ankle radiographs (Figures 2a and b).
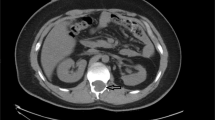
In TPBS, images from the anterior and posterior positions in the third phase showed increased activity in the intraphalangeal and metacarpophalangeal joints in both hands, in both wrists (markedly in the left one), and in both ankles (markedly in the right one). These observations support a diagnosis of stage 3 CRPS type I (Figure 3a and b).
After the diagnosis of CRPS type I was established in all four extremities, passive range of motion (PROM) exercises were started. Extremities with edema were elevated. Transcutaneous electrical nerve stimulation (TENS) and whirlpool sessions were used to control pain and edema. Drug therapy included intramuscular calcitonin 100 UI/day, naproxen sodium 550 mg/day and amitriptyline 75 mg/day.
After 6 weeks of treatment, the patient's visual analog scale score for pain had decreased by more than 50%, dropping to 38 mm from an initial score of 85 mm at the onset of treatment. PROM of wrists/hands, fingers and ankles had become full and painless. Edema in the hands and feet had decreased, and skin temperature had returned to normal.
With a recommendation to continue treatment for CRPS type I, the patient was discharged with a knee–ankle–foot orthosis on the right, an ankle–foot orthosis on the left, and a pair of lofstrand crutches for walking.
Discussion
Although CRPS type I is encountered quite frequently in hemiplegic patients, its incidence among SCI patients is relatively low.8, 9 Gellman et al10 identified a 10% incidence of CRPS type I in their series of 60 patients with tetraplegia. Cremer et al2 showed an association between CRPS type I and traumatic myelopathy in five cases. Wainapel11 described two patients who developed upper extremity CRPS type I with a clinical presentation of central cord syndrome following traumatic cervical myelopathy. Lefkoe and Cardenas presented one patient with CRPS type I in the lower extremity.12
In the literature published so far, CRPS type I in tetraplegic patients has mostly occurred in the upper extremities, with lower extremity involvement mentioned in only one report. To the best of our knowledge, no reports have been published of patients who have tetraplegia and CRPS type I existing simultaneously in upper and lower extremities.
Among the reasons for low incidence of CRPS type I in tetraplegic patients are early and prompt mobilization, regular application of PROM exercises (which tend to have a preventive effect), and corticosteroid treatment during the post-traumatic period.11, 12 That the use of systemic corticosteroids may be prophylactic against CRPS type I is discussed by many authors.7, 13, 14
Some authors have suggested that the reported incidence of CRPS type I in tetraplegic patients is low because it is misdiagnosed as pain of alternate etiology. Dysesthetic or central pain can easily be confused with CRPS type I.11 Autonomic dysfunction resulting from cervical cord injury may also add to the diagnostic confusion in the patient with suspected CRPS type I.12 In the diagnosis of CRPS type I in the lower extremity, it is important to distinguish it from more frequently encountered complications such as deep vein thrombosis and heterotopic ossification.
TPBS is frequently used to support the clinical diagnosis of CRPS type I. The sensitivity and specificity of this test in CRPS type I are reported to be 60 and 86%, respectively.7 However, it should be noted that bone scintigraphy is only positive for significant changes during the subactive period.8
A factor in the development of CRPS type I in this patient may have been his late commencement of a rehabilitation program, in addition to his immobilization that resulted from incomplete tetraplegia. Treatment of CRPS type I should be immediate and, most importantly, should be directed toward restoration of full function of the extremity.9 Multiple treatment modalities in CRPS type I have been described. In our patient, we used TENS together with Amitriptyline and Calcitonin in pain control. TENS inhibits A delta and C neuronal transmission by selectively stimulating the A beta neurons. Stimulation of sensory neurons with low-frequency TENS causes beta endorphin and enkephalin secretion, thereby providing pain relief.15 Tricyclic antidepressants inhibit reuptake of monoaminergic transmitters. There is solid evidence that Amitriptyline (which blocks reuptake of serotonin and noradrenaline) and Desipramine (which selectively blocks noradrenaline) produce pain relief in diabetic or postherpetic neuropathy. The mean dose that is often sufficient for pain reduction (eg Amitriptyline 25–75 mg/day) is smaller than doses necessary to achieve antidepressive effects.16 Calcitonin decreases bone resorption and may help protect the structure of bony architecture. It has an analgesic effect through the central serotonergic system.17
Conclusions
This is the first reported patient with tetraplegia in whom CRPS type I was present simultaneously in upper and lower extremities. We conclude that CRPS type I might be more common in SCI than is usually suspected, and that tetraplegic patients should be carefully evaluated for the presence of CRPS type I. As we have shown in this case report, the possibility that CRPS type I may simultaneously exist in upper and lower extremities should also be taken into account in the treatment of patients with tetraplegia.
References
Siddall PJ, Taylor DA, McClelland JM, Rutkowski SB, Cousins MJ . Pain report and the relationship of pain to physical factors in the first 6 months following spinal cord injury. Pain 1999; 81: 187–197.
Cremer SA, Maynand F, Davidoff G . The reflex sympathetic dystrophy syndrome associated with traumatic myelopathy: report of 5 cases. Pain 1989; 37: 187–192.
Davis R . Pain and suffering following spinal cord injury. Clin Orthop 1975; 112: 76–80.
Merskey H, Bogduk N . Classification of chronic pain; descriptions of chronic pain syndromes and definition of terms. IASP Press: Seattle 1995.
Schott GD . Reflex sympathetic dystrophy. J Neurol Neurosurg Psychiatry 2001; 71: 291–295.
Galer BS, Schwartz L, Allen RJ . Complex regional pain syndromes-type I: Reflex sympathetic dystrophy, and type II: Causalgia. In: Loeser JD (ed). Bonica's Management of Pain, 3rd edn. Lippincott Williams & Wilkins: Philadelphia 2001, pp 388–411.
Kozin F, Soin JS, Ryan LM, Carerra GF, Wortmann RF . Bone scintigraphy in the reflex sympathetic dystrophy syndrome. Radiology 1982; 138: 437–443.
Chalsen GG, Fitzpatrick KA, Navia RA, Bean SA, Reding MJ . Prevalence of the shoulder–hand pain syndrome on an in-patient stroke rehabilitation population; a quantitive cross-sectional study. J Neurol Rehabil 1987; 1: 137–141.
Wasner G, Schattscheider J, Binder A, Baron R . Complex regional-diagnostic, mechanisms, CNS involvement and therapy. Spinal Cord 2003; 41: 61–75.
Gellman H, Eckert RR, Botte MJ, Sakimura I, Waters RL . Reflex sympathetic dystrophy in cervical spinal cord injury patients. Clin Orthop 1988; 233: 126–131.
Wainapel SF . Reflex sympathetic dystrophy following traumatic myelopathy. Pain 1984; 18: 345–349.
Lefkoe TP, Cardenas DD . Reflex sympathetic dystrophy of the lower extremity in tetraplegia; case report. Spinal cord 1996; 4: 239–242.
Davis SW, Petrillo CR, Eichberg RD, Chu DS . Shoulder–hand syndrome in a hemiplegic population, a five years retrospective study. Arch Phys Med Rehabil 1977; 58: 353–356.
Christensen K, Jensen EM, Noer I . The reflex dystropy syndrome respone to treatment systemic corticosteroids. Acta Chir Scand 1982; 148: 653–655.
Kumar K, Nath RK, Toth C . Spinal cord stimulation is effective in management of reflex sympathetic dystrophy. Neurosurgery 1997; 40: 503–509.
Max MB, Lynch SA, Muir J, Shoaf SE, Smoller B, Dubner R . Effects of desipramine, amitriptyline and fluoxetine on pain in diabetic neuropathy. N Engl J Med 1992; 326: 1250–1256.
Clemento G, Amico Roxas M, Rasiparda E . The analgesic activity of Calcitonin and the central serotonergic system. Eur J Pharmacol 1985; 108: 71–75.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Sutbeyaz, S., Koseoglu, B. & Yeşiltepe, E. Simultaneous upper and lower extremity complex regional pain syndrome type I in tetraplegia. Spinal Cord 43, 568–572 (2005). https://doi.org/10.1038/sj.sc.3101742
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101742