Abstract
Study design: Prospective, observational study.
Setting: Country General Hospital, Singapore.
Objective: Intraoperative monitoring (IOM) with motor-evoked potentials (MEPs) assesses the integrity of cortical spinal tracts during scoliosis surgery. MEPs are sensitive to the effects of inhalational anesthetic agents. We evaluate the use of desflurane in combination with multipulse cortical stimulation in this study.
Methods:In all, 10 consecutive neurologically normal subjects underwent scoliosis surgery with desflurane anesthesia (0.5 maximum alveolar concentration) and five pulse cortical stimulation (250 Hz) from two stimulators in parallel configuration, delivering a maximum intensity of 160 mA.
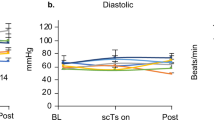
Results: Consistent MEPs were obtained from the abductor hallucis and tibialis anterior in nine of ten and five of five of subjects, respectively. Baseline coefficients of variations were below 16% for both muscles.
Conclusion: This combination of anesthetic and stimulation protocols is efficacious for IOM during spinal cord surgery. Our findings support the use of desflurane for successful acquisition of MEPs during scoliois surgery as an alternative anesthetic regime.
Similar content being viewed by others
Introduction
Intraoperative monitoring (IOM) with motor-evoked potentials (MEPs) is a means of assessing corticospinal tract integrity during spinal surgery. 1 Several techniques have been developed to improve the consistency of MEPs in the operating theater,2,3 usually involving delivery of multiple electrical stimulation pulses.
MEPs are sensitive to the effects of inhalational anesthetic agents, which offer the advantages of rapid induction and recovery with its low solubility.4 To improve the quality of MEP monitoring, electrical stimulation protocols and anesthesia management are of equal importance intraoperatively. In this study, we evaluate the use of a volatile halogenated anesthetic in combination with a multipulse technique of cortical stimulation and report its efficacy in IOM.
Methods
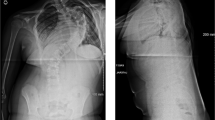
In all, 10 consecutive patients (all females, mean age: 18 years, range: 14–23 years) undergoing elective scoliosis surgery were entered into the study with informed consent. Contraindications to cortical stimulation (seizures, pacemaker, cranial surgery or implants) were excluded. All patients were neurologically normal, as determined preoperatively by an experienced neurologist.
Multipulse transcranial electrical stimulation was performed using two constant-current stimulators connected in parallel configuration from a Dantec Keypoint EMG machine (Dantec, Skovlunde, Denmark). A train of five square wave stimuli 0.5 ms in duration was delivered at 4 ms (250 Hz) interstimulus intervals. Stimulating electrodes consisted of 9 mm gold-plated disc electrodes at C3C4 (International 10-20 system) affixed with collodion. Occasionally, the C1C2 position was utilized to improve MEP responses intraoperatively. Stimulation output was increased from 50 mA in steps of 5 mA until a reproducible MEP was elicited. The intensity was then increased and fixed at 10% above this threshold intensity. Each stimulator was capable of delivering a maximum output of 100 mA (200 mA in total). MEP recordings were obtained with 13 mm disposable subdermal needles (Technomed Europe, Beek, Netherlands) in the abductor hallucis (AH) bilaterally. In five patients, MEP recordings were also made from the tibialis anterior (TA) bilaterally. Filter settings were set at 10 and 2 kHz. Input impedance of stimulating and recording electrodes were maintained below 5 kΩ.
For induction of anesthesia, sodium thiopentone at 4 mg/kg and fentanyl at 2 μg/kg was administered. A dose of 0.8 mg/kg of intravenous atracurium was used to facilitate endotracheal intubation. No further doses of neuromuscular blocking agents were used subsequently. Anesthesia was maintained using 60% nitrous oxide in oxygen. Desflurane was introduced through a calibrated vaporizer up to an end-tidal concentration of 2.1–4.4%, with a mean concentration of 3.3% (approximately 0.5 maximum alveolar concentration (MAC)). This was measured using an Ohmeda respiratory gas monitor 5250 (BOC Group, Louisville, KY, USA). Closed-circuit mechanical ventilation was adjusted to maintain end-tidal carbon dioxide levels between 32 and 35 mmHg. Monitoring included electrocardiography, pulse oximetry, capnography and direct radial artery pressures. All patients were kept normothermic with a warming blanket. Normotensive anesthesia was maintained throughout the operation.
After approximately 45 min post-induction, a train of four twitch assessment was performed using a nerve stimulator (Fischer Paykel NS242, UK). Cortical stimulation was commenced only when the amplitude of the fourth was visibly similar to the first. An interval of 3–5 min was allowed between two trains of cortical stimulation. This alternated with monitoring of somatosensory-evoked potentials from posterior tibial nerve stimulation.
Peak to peak amplitudes (between the two largest peaks opposite in polarity) and onset latency were utilized for all MEP responses. Within each patient, 10 consecutive MEPs obtained before insertion of pedicle screws were used as a baseline for the calculation of coefficients of variation (CV). During insertion of pedicle screws and instrumentation, a 50% reduction of MEP amplitude or 10% prolongation of latency was brought to the surgeon's attention.
Results
There were no complaints of headache, seizures or skin burns postoperatively; all patients had normal neurological examination.
MEPs were obtained from nine of 10 patients using AH recordings bilaterally. All five patients with TA recordings had MEPs elicited bilaterally. The stimulation intensity required was up to 80 mA per stimulator (80 mA+80 mA=160 mA in total via two stimulators).
None of the nine patients had MEP amplitude or latency changes exceeding our set limits so as to require immediate surgical attention during and after pedicle screw insertion and spinal instrumentation. Table 1 summarizes MEP results for both muscles. The examples of MEPs obtained from both muscles are shown in Figure 1.
Discussion
The need for IOM in scoliosis surgery is justified by the risk of spinal cord damage during insertion of pedicle screws, instrumentation and rod tightening,5 particularly in healthy young subjects with no preoperative neurological deficits. In this study, we were able to obtain reproducible MEPs in 90% of subjects using AH and 100% of subjects using TA recordings.
Jones et al 6 obtained consistent MEPs in 21 of 22 (96%) patients using infused propofol with alfentanil as anesthesia, supplemented with nitrous oxide. Pelosi et al7 studied 50 operations and reported consistent MEPs (CV: 22%) in 97% of patients during propofol anesthesia. However, this dropped to 61% (CV: 29%) when isoflurane was used as an inhalational anesthetic. These results compare well with those from our study, which obtained CVs below 16% from both AH and TA recordings. It can also be seen that the introduction of isoflurane significantly affected the success of MEP monitoring, in comparison with the use of propofol. However, it should be noted that direct comparison between studies may not be totally feasible, in view of inherent differences in methodology.
Both the above studies utilized constant-voltage stimulators (D 185, Digitimer, Welwyn Garden City, Hertfordshire, UK), generating 3–6 stimuli 50 μs in duration at 2 ms intervals. Stimulating voltages were up to 1000 V. Hausmann et al,8 also using a similar stimulation protocol, obtained MEPs in 15 of 18 (83.3%) patients. They compared this with the use of a five-pulse stimulation protocol almost similar to our technique, but at a faster frequency of 400 Hz, which yielded similar results. Again, these results were obtained with intravenous anesthetic regimes. Mean amplitudes and CVs were not reported, but variation in MEP areas were in the region of 22%. Ubags et al9 employed 0.6% end-tidal isoflurane, approximately equivalent to 0.5 MAC of desflurane, and obtained MEPs in 9 of 10 patients. However, several essential differences prevail. Firstly, the stimulation regime utilized a D185 stimulator, which gives a different charge delivery compared with ours.8 Secondly, the two anesthetic agents are different compounds with different molecular structures. Hence, direct comparison will be difficult given that the two concentrations of 0.6 and 0.5% MAC are not totally equivalent. Moreover, our 0.5 MAC represents a mean value of the 10 patients, whereas Ubags et al employed a relatively fixed 0.6% concentration.
Comparison with these previous studies suggests that our use of desflurane did play a significant role in increasing the yield and consistency of MEPs obtained. What are the possible underlying reasons? Isoflurane is well recognized to affect MEP recordings significantly.10,11,12 Desflurane has been shown to alter the amplitude of somatosensory-evoked potentials in rats13 and MEPs at 1 MAC. At 2 MAC, MEPs were completely unobtainable.14 However, it remains unclear as to why our use of desflurane resulted in a high percentage of stable MEPs elicited. A comprehensive literature search did not reveal any obvious reason as to how desflurane affects MEPs. However, desflurane is well documented to depress spinal motorneuron excitability,15 which may also affect MEPs. In our protocols, desflurane concentrations were in the region of 0.5 MAC. Hence, it is possible that we have achieved a suitable ‘concentration window’ enabling effective anesthesia, in addition to successful MEP monitoring. However, the exact mechanisms, including comparisons with its spinal cord actions,16 remain to be determined in future animal and human studies.
This paper, to our knowledge, is the first to report the use of desflurane in combination with a multiple cortical stimulation regime. Our findings support the use of N20/desflurane for successful acquisition of MEPs during scoliois surgery. This new finding is of interest as an alternative anesthetic regime, particularly when desflurane is well known to allow faster awakening and earlier psychomotor recovery17,18 when compared to other agents. Additionally, further studies based on variations of similar strategies aimed at improving current results are justified.
References
Burke D, Hicks RG . Surgical monitoring of motor pathways. J Clin Neurophysiol 1998; 15: 194–205.
Inoue S et al. Intraoperative monitoring of myogenic motor-evoked potentials from the external anal sphincter muscle to transcranial electrical stimulation. Spine 2002; 27: 454–459.
MacDonald DB . Safety of intraoperative transcranial electrical stimulation motor evoked potential monitoring. J Clin Neurophysiol 2002; 19: 416–429.
Young CJ, Apfelbaum JL . Inhalational anesthetics: desflurane and sevoflurane. J Clin Anesth 1995; 7: 564–577.
MacDonald DB, Al Zayed Z, Khoudeir I, Stigsby B . Monitoring scoliosis surgery with combined multipulse transcranial electric motor and cortical somatosensory evoked potentials from the lower and upper extremities. Spine 2003; 28: 194–203.
Jones SJ, Harrison R, Koh CF, Mendoza N, Crockard HA . Motor evoked potential monitoring during spinal surgery: responses of distal limb muscles to transcranial cortical stimulation with pulse trains. Electroencephalogr Clin Neurophysiol 1996; 100: 375–383.
Pelosi L, Stevenson M, Hobbs GJ, Jardine A, Webb JK . Intraoperative motor evoked potentials to transcranial electrical stimulation during two anesthetic regimens. Clin Neurophysiol 2001; 112: 1076–1087.
Hausmann ON, Min K, Boos N, Ruetsch YA, Erni T, Curt A . Transcranial electrical stimulation: significance of fast versus slow charge delivery for intraoperative monitoring. Clin Neurophysiol 2002; 113: 1532–1535.
Ubags LH, Kalkman CJ, Been HD . Influence of isoflurane on myogenic motor evoked potentials to single and multiple transcranial stimuli during nitrous oxide/opioid anesthesia. Neurosurgery 1998; 43: 90–94.
Calancie B, Klose KJ, Baier S, Green BA . Isoflurane-induced attenuation of motor evoked potentials caused by electrical motor cortex stimulation during surgery. J Neurosurg 1991; 74: 897–904.
Pechstein U, Nadstawek J, Zentner J, Schramm J . Isoflurane plus nitrous oxide versus profofol for recording of motor evoked potentials after high frequency repetitive electrical stimulation. Electroencephalogr Clin Neurophysiol 1998; 108: 175–181.
Zhou HH, Zhu C . Comparison of isoflurane effects on motor evoked potential and F wave. Anesthesiology 2000; 93: 32–38.
Haghighi S, Sirintrapun SJ, Johnson JC, Keller BR, Oro JJ . Suppression of spinal and cortical somatosensory evoked potentials with desflurane anesthesia. J Neurosurg Anesthesiol 1996; 8: 148–153.
Haghighi S, Sirintrapun SJ, Keller BP, Oro JJ, Madsen R . Effects of desflurane anesthesia on transcortical motor evoked potentials. J Neurosurg Anesthiol 1996; 8: 47–51.
Rampil IJ, King BS . Volatile anesthetics depress spinal motor neurons. Anesthesiology 1996; 85: 129–134.
Pereon Y, Bernard JM, Nguyen S, Genet R, Petitfaux F, Guiheneuc P . The effects of desflurane on the nervous system: from spinal cord to muscles. Anesth Analg 1999; 89: 490–495.
Ghouri AF, Bodner M, White PF . Recovery profile after desflurane-nitrous oxide versus isoflurane-nitrous oxide in outpatients. Anesthesiology 1991; 74: 419–424.
Apfelbaum JL, Lichtor JL, Lane BS, Coalson DW, Korttila KT . Awakening, clinical recovery, and psychomotor effects after desflurane and profofol anesthesia. Anesth Analg 1996; 83: 721–725.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Lo, Y., Dan, Y., Tan, Y. et al. Intra-operative monitoring in scoliosis surgery with multi-pulse cortical stimuli and desflurane anesthesia. Spinal Cord 42, 342–345 (2004). https://doi.org/10.1038/sj.sc.3101605
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101605
Keywords
This article is cited by
-
Somatosensory evoked potential loss due to intraoperative pulse lavage during spine surgery: case report and review of signal change management
Journal of Clinical Monitoring and Computing (2020)
-
The contribution of neurophysiology in the diagnosis and management of cervical spondylotic myelopathy: a review
Spinal Cord (2016)
-
A comparison of the effects of desflurane versus propofol on transcranial motor-evoked potentials in pediatric patients
Child's Nervous System (2014)
-
Intraoperative monitoring study of ipsilateral motor evoked potentials in scoliosis surgery
European Spine Journal (2006)
-
A prospective study of the utility of preoperative somatosensory evoked potentials in spinal surgery
European Spine Journal (2005)