Abstract
Design: This paper describes a treatment paradigm to facilitate functional gait in a quadriplegic, ASIA C spinal cord injured (SCI), wheelchair-dependent subject who presented with some large fiber sensation, sub-functional motor strength in all lower limb muscles, and moderate spasticity. The study utilizes partial weight bearing therapy (PWBT) followed by epidural spinal cord stimulation (ESCS) with the assumption that both treatments would be necessary to elicit a well organized, near effortless functional gait with a walker. Function is defined in terms of accomplishing task-specific activities in the home and community.
Objectives: To demonstrate the feasibility and benefits of combined PWBT and ESCS therapies aimed at promoting functional gait in a wheelchair-dependent ASIA C SCI subject.
Setting: The Clinical Neurobiology and Bioengineering Research Laboratories at Good Samaritan Regional Medical Center, Phoenix, Arizona, USA, and the Department of Bioengineering, Arizona State University, Tempe, Arizona, USA.
Methods: The study began with the application of PWBT. The subject walked on the treadmill until a plateau in gait rhythm generation was reached. Subsequently, ESCS, applied to the lumbar enlargement, was utilized to facilitate PWBT and, later, over-ground walking for a standard distance of 15 m. Gait performance was analyzed by measuring average speed, stepping symmetry, sense of effort, physical work capacity, and whole body metabolic activity.
Results: PWBT led to improved stereotypic stepping patterns associated with markedly reduced spasticity, but was insufficient for over-ground walking in terms of safety, energy cost, and fatigue. ESCS with PWBT generated immediate improvement in the subject's gait rhythm when appropriate stimulation parameters were used. When compared to the non-stimulated condition, over-ground walking with ESCS across a 15 m distance was featured by a reduction in time and energy cost of walking, sense of effort, and a feeling of ‘lightness’ in the legs. After a few months of training, performance in speed, endurance, and metabolic responses gradually converged with/without ESCS at this short distance, suggesting a learned response to these conditions. However, at longer distances (eg, 50–250 m), performance with ESCS was considerably superior. The subject was able to perform multiple functional tasks within the home and community with ESCS.
Conclusion: We propose that ESCS augments the use-dependent plasticity created by PWBT and may be a valuable adjunct to post-SCI treadmill training in ASIA C subjects. We also conclude that ESCS elicits greater activation of an oxidative motor unit pool, thereby reducing the subject's sense of effort and energetic cost of walking.
Similar content being viewed by others
Introduction
Among the approximately 250 000 spinal cord injured (SCI) living in the USA, there is a considerable population of chronic incomplete SCI (ISCI) who are designated as ASIA B or C, (some sensory sparing, B indicates abolished motor power and C refers to sub-functional motor power in the lower extremities), and are wheelchair-dependent, ie they are not consistent functional ambulators with respect to homebound or community walking.1
Two novel strategies have been individually employed to augment locomotion rhythm generation, making use of the adaptability and capacity for retraining/learning of spinal cord circuits:2 Partial Weight Bearing Therapy (PWBT) and Epidural Spinal Cord Stimulation (ESCS). PWBT has evolved from observations of chronic spinal animals whereby, a moving treadmill can initiate and sustain locomotion when the body is supported.3 As a consequence, various afferent inputs into the intrinsic spinal circuitry contribute to a coordinated locomotion pattern with state- and phase-dependent reflexes.4 While it is well respected that PWBT facilitates functional walking among chronic ASIA D patients (significant functional motor power), to our knowledge, there is no data regarding the effect of PWBT among ASIA B and C patients in transforming walking on the treadmill to restoration of functional ambulation in terms of household or community walking.3
Non-patterned ESCS, which modulates segmental spinal and/or brain stem-spinal pathways in the ISCI, has also shown potential in initiating and sustaining locomotion among MS and ASIA D patients.5,6 Using stimulus parameters consisting of low frequency, long pulse duration, and supra-motor threshold intensity, ESCS of the lumbar enlargement in animals induced hind-limb locomotion patterns following an acute mid-thoracic spinal cord transection.7 These parameter settings, however, contrast with Dimitrijevic's observations in acute human experiments with clinically complete SCI in a supine position.8
Assuming that PWBT or ESCS alone does not induce functional walking in ISCI patients classified as ASIA B or C, we posited that in a subset of ASIA C patients (ie, all muscles of the lower extremity are sub-functional) a combination of the two novel therapies (PWBT and ESCS) would be more effective than either therapy alone in restoring functional walking.
Methods
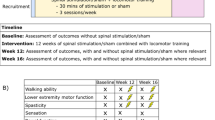
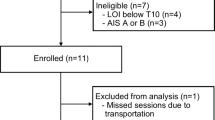
A 43-year-old male C5-6 ISCI (ASIA C) wheelchair-dependent quadriplegic subject (3.5 years post injury) was recruited. Spasticity was characterized by muscle spasms and rigidity. PWBT was performed using the LiteGait™ system (Mobility Research, Tempe, AZ, USA). Under the guidance of physical therapists, the subject underwent progressive training with increasing treadmill rates (0.5 mile/hour to 2.0 mile/hour) and degrees of weight bearing (60% to 90%) to a plateau in performance.
A pair of Pisces-Quadplus electrodes (in combination with the X-TREL stimulation system by Medtronic Inc., Minneapolis) were inserted into the dorsal epidural space over the upper lumbar enlargement of the spinal cord. Each electrode was placed 1–2 mm off the mid-line. After surgical wound healing and retraining with PWBT to the pre-surgery level, a variety of electrical parameter sets were examined to test the efficacy of ESCS on promoting gait. Gait performance was assessed by measuring average speed, stepping symmetry, sense of effort (approximating the Borg Scale,9 −/10 with the higher numbers representing an increased sense of effort), and physical work capacity. Whole body metabolic rate and fuel oxidation were measured at rest and during walking using indirect calorimetry. Expired air was collected in meteorological balloons and analyzed for volume and gas composition (CO2 and O2). The calculated O2 consumption rate (VO2) and CO2 production rate (VCO2) were inserted into the equations of Frayn10 to calculate carbohydrate and fat oxidation rates.
The study was approved by the local Institutional Review Boards at the Good Samaritan Regional Medical Center (GSRMC) and Arizona State University (ASU) and received permission to proceed from the food and Drug Administration. The patient gave his informed consent.
Results
PWBT led to an improved stereotypic stepping pattern on the treadmill and reduced spasticity during an over-ground 15 m walk. The over-ground locomotion pattern was associated with extremely low speeds, poor endurance, and a marked sense of effort (8/10). After combining PWBT and ESCS, we observed an immediate improvement, a propensity to exhibit a well-organized smoother stepping pattern at higher treadmill rates and self-supported body weight, considerable improvement in endurance and speed during over-ground walking, and reduced sense of effort (2/10). These changes were not ascribed to a change in spasticity, as spasticity was markedly reduced by PWBT prior to the application of ESCS.
Vital ESCS parameters appeared to be electrode distance, pulse duration, and amplitude. We observed that long pulse durations (eg, 0.8 msec) were essential while frequencies (eg, 20–60 Hz) were comparatively less sensitive. The amplitude was above sensory threshold (sense of ‘parasthesia or vibration’) but below that causing motor contraction. Parasthesia was bilateral and symmetrical. The span across the four contacts of each electrode was at least 15 mm to cover a wide segment of the spinal cord lumbar enlargement.
Early in the transition from PWBT to over-ground walking, pulmonary gas exchange revealed that ESCS reduced the O2 (energy) cost of walking by 36% (to walk the same distance) and 27% (to walk for the same duration, Figure 1A). Carbon dioxide production, VCO2, was more markedly reduced by ESCS. Consequently, the fat oxidation rate elicited by walking, calculated using the VCO2 and VO2 above the resting level (same under both conditions), was increased by as much as eightfold by ESCS (Figure 1B).
Without ESCS the patient walked 42 meters in 7.2 min. Gas exchange was measured in both conditions, without stimulation and with ESCS over the same distance (42 m) and duration (7.2 min) that resulted in exhaustion in the NON-ESCS condition. (A) The O2 cost of walking (ml O2 ·km−1· kg−1) was calculated as O2 consumption rate during walking (ml· kg−1· min−1) divided by walking speed (km· min−1). (B) Resting VO2 and VCO2 values were essentially identical for both trials. Net VO2 and VCO2 were calculated as the exercise-induced (net) increases above these resting values. Net VO2 and net VCO2 were then inserted into the equations of Frayn10 to calculate the apparent fuel oxidation elicited by walking. ESCA resulted in roughly sixfold (same duration) to eightfold (same distance) greater fat oxidation during walking
ESCS was associated with increased walking speed and decreased sense of effort by a factor of three. With 1.5 months of continual training, the average walking speed, the gas exchange responses, as well as endurance, converged between the two conditions (ESCS and non-ESCS). Figure 2 shows the time required to ambulate over 15 m. The polynomial (‘poly’) trend line demonstrated a continued improvement for the non-ESCS condition. Yet, at longer distances, ESCS was associated with better endurance, decreased sense of effort, and a feeling of ‘lightness of the legs’. After four months of over-ground training, the subject could ambulate 270 m. He demonstrated an ability to perform community and homebound functional ambulation.
Duration of time for the subject to traverse a distance of 15 m at different stages of the treatment. Walking speed increased to a limited degree during PWBT treatment (6/1–10/1/2000) but the patient remained dysfunctional. ESCS was associated with an immediate impact on walking speed (1/1–4/1/2001). The difference in performance between the stimulation and non-stimulation conditions noted on 1/1/2001 was substantially reduced after four months of training for the short distance walking
Discussion
The mechanism of PWBT may be ascribed to retraining spinal cord circuits to promote the sensitivity of the system for locomotion rhythmic related signals, within the context of both motor drives and sensory-motor reflexes. When the injury is severe (ASIA B or C), signals from motor drives and sensors are weak. By means of PWBT (treadmill training), the non-functional motor capacity gradually developed into coordinated intra- and inter-limb movements with signs of activity (use)-dependent plasticity.2 However, such movements remained non-functional as the attempt to transfer the learned coordinated movements to efficient over-ground walking for homebound and community walking failed. When ESCS was applied in conjunction with PWBT, the electrical current appeared to provide the modulation/amplification of the neural circuits responsible for locomotion rhythm generation by further exciting segmental afferent inputs and facilitating a ‘stored’ locomotion program. This led to a near-effortless, coordinated locomotion pattern over substantial distances (eg, 270 m) and to homebound and community walking.
The gas exchange data indicated that ESCS reduced the energy cost of walking by roughly 20% to 30%. The impact of ESCS on CO2 production was more pronounced. If acid-base balance during walking is assumed, gas exchange data indicated eightfold-greater exercise-induced fat oxidation rate to walk the same distance with ESCS. Alternatively, lower CO2 production during ESCS-assisted walking could have reflected less accumulation of blood lactate and associated bicarbonate titration. Both interpretations imply that ESCS reduced dependence of exercising muscle on glycolysis, and hence, accounted for the marked improvement in muscle endurance observed in the ESCS condition. We conclude that ESCS may elicit greater activation of an oxidative motor unit pool in the spinal cord (possibly via modulating afferent input, eg, Ia fibers which can alter motor unit recruitment patterns11) thereby reducing the sense of effort12 and the energetic cost of walking, and expanding physical work capacity.
We propose that ESCS augmented the use-dependent plasticity created by PWBT and concur with the view that ESCS ‘has the potential for serving as a valuable adjunct to post SCI treadmill training and other therapeutic interventions’.7 In our view, the patient's ‘sensation of lightness’ associated with a sensation of a ‘low sense of effort’, was a feature in the difference between the stimulation and non-stimulation conditions. These behaviors were also noted by Cook and Weinstein,5 who used ESCS to facilitate locomotion among MS patients.
Though the results reported here are derived from only one subject, it is clear that the combined PWBT and ESCS therapy can facilitate restoration of functional ambulation of a wheelchair-dependent ISCI patient. Further trials of these therapeutic techniques are required in ASIA C patients. Pending their success, future studies should be expanded to include ASIA B patients.
References
Lapointe R, Lajoie Y, Serresse O, Barbeau H . Functional community ambulation requirements in incomplete spinal cord injured subjects Spinal Cord 2001 39: 327–335
Wolpaw JR, Tennissen AN . Activity-dependent spinal cord plasticity in health and disease Annu Rev Neurosci 2001 24: 807–843
Barbeau H, Ladouceur M, Norman KE, Pepin A, Leroux A . Walking after spinal cord injury: evaluation, treatment, and functional recovery Arch Phys Med Rehabil 1999 80: 225–235
Muir GD, Steeves JD . Sensorimotor stimulation to improve locomotor recovery after spinal cord injury TINS 1997 20: 72–77
Cook AW, Weinstein SP . Chronic dorsal column stimulation for the treatment of movement disorders NY State J Med 1973 73: 2868–2872
Davis R, Gray E, Kudzma J . Beneficial augmentation following dorsal column stimulation in some neurological diseases Appl Neurophysiol 1981 44: 37–49
Iwahara T, Atsuta Y, Garcia-Rill E, Skinner RD . Spinal cord stimulation-induced locomotion in the adult cat Brain Res Bull 1992 28: 99–105
Dimitrijevic MR, Gerasimenko Y, Pinter MM . Evidence for a spinal central pattern generator in humans In: Kiehn O, Harris-Warrick RM, Jordan LM, Hultborn H, Kudo N (eds) Neuronal Mechanisms for Generating Locomotor Activity. Ann N Y Acad Sci. Vol. 860: New York: New York Academy of Sciences 1998 pp 360–376
Robertson RJ, Goss FL, Metz KF . Perception of physical exertion during dynamic exercise Percept Mot Skills 1998 86: 183–191
Frayn KN . Calculation of substrate oxidation rate in vivo from gas exchange J Appl Physiol 1983 55: 628–634
Burke RE, Edgerton VR . Motor unit properties and selective involvement in movement Exerc Sport Sci Rev 1975 3: 31–81
Granit R . Constant errors in the execution and appreciation of movement Brain 1972 95: 649–660
Acknowledgements
We gratefully acknowledge the funding supports from the GSRMC and ASU. We also recognize the assistance of the physical therapy staff at GSRMC, Qingjun Wang, Gary Yamaguchi, James Sweeney and Jeffrey Thrasher to this project. We appreciate Amir Seif-Naraghi for his valuable insight in this project, Medronic for contributing the stimulation device, and the Whitaker Foundation's partial support.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Herman, R., He, J., D'Luzansky, S. et al. Spinal cord stimulation facilitates functional walking in a chronic, incomplete spinal cord injured. Spinal Cord 40, 65–68 (2002). https://doi.org/10.1038/sj.sc.3101263
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101263
Keywords
This article is cited by
-
Neuroprosthetics: from sensorimotor to cognitive disorders
Communications Biology (2023)
-
Activity-dependent spinal cord neuromodulation rapidly restores trunk and leg motor functions after complete paralysis
Nature Medicine (2022)
-
Motor improvements enabled by spinal cord stimulation combined with physical training after spinal cord injury: review of experimental evidence in animals and humans
Bioelectronic Medicine (2021)
-
Transcutaneous Spinal Neuromodulation Reorganizes Neural Networks in Patients with Cerebral Palsy
Neurotherapeutics (2021)
-
Functional magnetic resonance imaging (fMRI) of the sensorimotor cortex in spinal cord injury patient after intensive rehabilitation
Research on Biomedical Engineering (2020)