Abstract
The effects of halothane and ketamine anesthesia on [11C]raclopride binding were assessed in the cat striatum at basal conditions and after drug- or depolarization-induced dopamine (DA) release using Positron Emission Tomography. At baseline, Scatchard analyses revealed that the higher [11C]raclopride binding found under halothane anesthesia was mainly attributable to a higher radioligand apparent affinity. Decreased [11C]raclopride binding was demonstrated following amphetamine under ketamine but not under halothane anesthesia. Under ketamine anesthesia transient DA overflows induced by direct stimulations of DA neurons through an intracerebral electrode induced transient changes in [11C]raclopride binding with a remarkable spatiotemporal accuracy. No effect was observed under halothane anesthesia. The failure to detect competition between DA and [11C]raclopride for binding on D2-receptors under halothane anesthesia might reflect, as already reported for other brain receptor systems, a halothane-promoted conversion of D2-receptors to a state of lower affinity for DA. It is suggested that the affinity state of receptors is a factor to be considered in in vivo ligand-activation studies.
Similar content being viewed by others
Main
Over the last decade, in vivo neuroreceptor imaging techniques such as Positron Emission Tomography (PET) and Single-Photon Emission Computed Tomography (SPECT) have been used extensively to evaluate drug-induced changes in endogenous dopamine (DA) levels from changes in radioligand binding. Numerous studies have shown that the binding of [11C]raclopride and [123I]-(S)-2-hydroxy-3-iodo-6-methoxy-[(1-ethyl-2-pyrrolidinyl)methyl]benzamide ([123I]IBZM), two D2-receptor antagonists used in PET and SPECT imaging studies, respectively, is consistently decreased by drugs that elevate synaptic DA, while the opposite effect is observed with drugs that decrease synaptic DA (Innis et al. 1992; Dewey et al. 1993, 1995; Ginovart et al. 1997; Laruelle et al. 1997).
Competition between endogenous DA and radioligand for binding on D2-receptors has been regarded as the underlying mechanism to explain the changes in [11C]raclopride and [123I]IBZM bindings observed following changes in DA levels. Although the DA competition model has been used as the main explanation for these binding changes, a number of inconsistencies have emerged that questioned the validity of the model (reviewed in Laruelle 2000). For instance, it seems that the DA-induced change in binding is peculiar to benzamide radioligands, rather than being a general principle governing all D2-radioligands. Whereas the binding of benzamide compounds (raclopride, IBZM, fallypride) to D2-receptors is always affected by endogenous DA in a manner consistent with the model, the binding of butyrophenone compounds (spiperone, N-methyl-spiperone, pimozide) to D2-receptors shows either no change or even paradoxical increase in the face of higher DA (Baudry et al. 1977; Bischoff and Gunst 1997; Hartvig et al. 1997). This observation has led to the conclusion that factors others than endogenous DA also alter radioligand binding in vivo.
Several hypotheses have been raised in an attempt to identify these factors. It has been proposed that the higher affinity of butyrophenones, such as [11C]NMSP, for D2-receptors might explain their lower sensitivity to endogenous DA as compared with [11C]raclopride (Seeman et al. 1989). However, as proposed by Farde et al. (1990), the vulnerability of a radiotracer to a competitive inhibitor such as DA is not dependent on its affinity as long as binding quantification is performed at tracer dose. It has also been proposed that benzamides and butyrophenones do not bind to the same binding site on D2-receptors (Seeman et al. 1989; Hall et al. 1990). However, no unequivocal explanation has emerged that could account for the different behaviors of these radioligands with regards to competition with endogenous DA.
Another inconsistency in the validity of the DA competition model is the temporal discrepancies between changes in radioligand binding as measured with PET and SPECT and changes in DA levels as measured with microdialysis. Microdialysis studies in rodents and non-human primates have shown that amphetamine elevates striatal DA levels with peak values occurring within 20 min and that DA levels return to control values within 120 min (Sharp et al. 1987; Butcher et al. 1988; Laruelle et al. 1997). Amphetamine-induced elevation in DA levels is thus rapid and transient and contrasts with the long-lasting decrease in both [11C]raclopride and [123I]IBZM binding observed in vivo. Indeed, [11C]raclopride and [123I]IBZM bindings have been shown to be still reduced to their minimal levels at 5.5 h and 8 h, respectively, following a single dose of amphetamine in non-human primates (Carson et al. 2000) and in healthy humans (S. Kapur, personal communication). Such an inconsistency suggests that even for benzamides, factors other than endogenous DA might play a significant role in the alteration in BP observed following DA manipulation.
A critical factor that has to be considered in in vivo competition studies when performed in animals is that they require anesthesia for sedation and fixation of the animal during the PET or SPECT measurement. It has been proposed that anesthesia is often associated with significant changes in striatal DA levels, and may influence the response to dopaminergic drugs. One of the most commonly used anesthetic, ketamine, is a non-competitive N-methyl-D-aspartate antagonist that induces psychotic symptoms in humans. This effect is thought to be due to a facilitation of DA neurotransmission although several studies indicate that ketamine has no significant effect on striatal DA levels (Ylitalo et al. 1976; Koshikawa et al. 1988; Lannes et al. 1991; Micheletti et al. 1992; Onoe et al. 1994; Mantz et al. 1994; Irifune et al. 1997; Tsukada et al. 2000). Volatile anesthetics such as halothane have been consistently shown to release striatal DA (Ford and Marsden 1986; Savaki et al. 1986; Spampinato et al. 1986; Osborne et al. 1990; Stahle et al. 1990; Miyano et al. 1993; Mantz et al. 1994; Shiraishi et al. 1997; Keita et al. 1999). In addition, several authors showed that anesthesia by itself might have a significant influence on radioligand binding in vivo and that this effect might introduce severe bias in the interpretation of results obtained from in vivo competition studies. A recent PET study performed in non-human primates showed that ketamine dose-dependently reduced [11C]raclopride binding in the striatum without any significant change in DA extracellular concentration (Tsukada et al. 2000). Isoflurane, another volatile anesthetic, has been shown to potentiate the effect of DA enhancer drugs, such as cocaine and GBR12909, on [11C]raclopride binding in the striatum of anesthetized as compared with awake monkeys (Tsukada et al. 1999). These studies strengthen the idea that, even for benzamides, endogenous DA is not the only parameter to affect radioligand binding in vivo and one might question to which extent radioligand binding parameters are affected by anesthesia.
The current study was designed to investigate the effects of halothane and ketamine anesthesia on [11C]raclopride binding in the cat striatum both at basal conditions and after drug- or depolarization-induced DA release. The objective of this study was 3-fold: (1) to compare the effect of ketamine and halothane anesthesia on [11C]raclopride binding parameters at baseline; (2) to examine whether a rapid, transient (few minutes) and discrete increase in synaptic DA levels induced by direct stimulation of DA neurons has the same effect on striatal [11C]raclopride binding as the more sustained (few hours) increase in neurotransmitter levels induced by amphetamine administration; and (3) to compare the influence of both anesthetics on DA-induced changes in [11C]raclopride binding.
The within subject effect of ketamine- versus halothane-induced anesthesia on [11C]raclopride binding was examined in cats. Scatchard analyses based on four or five PET experiments were applied to determine whether potential differences in [11C]raclopride binding between both anesthetic conditions reflected a change in D2-receptor density or apparent affinity. In addition, a cat was chronically implanted with a bipolar electrode in the left medial forebrain bundle (MFB) allowing a direct and unilateral stimulation of DA nigrostriatal fibers. The effect of electrically-evoked DA release on [11C]raclopride binding was compared with that obtained after administration of the DA releasing drug amphetamine.
MATERIALS AND METHODS
Animals
A total of four Domestic male cats (noted cats #1, cat #2, cat #3, and cat #4) weighing about 4 kg were obtained from Iffa-Credo, Lyon, France. Animal studies were performed by licensed investigators in accordance with French (87-848, Ministère de l'Agriculture et de la Forêt) and European Economic Community (86-609, EEC) guidelines for care of laboratory animals. All efforts were made to minimize animal suffering and to use only the number of animals necessary to produce reliable scientific data.
In vivo Voltammetry Studies
One cat (cat #4) was simultaneously implanted with: (1) a stimulating bipolar electrode placed in the MFB allowing a direct and unilateral stimulation of DA nigrostriatal fibers; and (2) a recording carbon-fiber electrode placed in the ipsilateral striatum allowing measurement of DA release in response to axonal stimulation.
DA overflow was monitored with voltammetry by the carbon fiber microelectrode, the active part of which was the surface of a carbon fiber 8 μm in diameter and 250 μm long (Chergui et al. 1994; Dugast et al. 1994). Prior to implantation, the carbon-fiber microelectrode was electrochemically pre-treated as previously described by Gonon et al. (1984) and calibrated in vitro in a 50 mM phosphate-buffered saline (PBS) solution containing 50 nM DA and 100 μM ascorbic acid. The potential value corresponding to the oxidation of DA was determined in vitro by differential normal pulse voltammetry (DNPV) using a pulse voltammetric system (Biopulse, SOLEA Tacussel, France) as previously described by Gonon and Buda (1985).
The cat was anesthetized with halothane (4%). As soon as deep anesthesia was obtained, an endotracheal intubation was performed and anesthesia was maintained with halothane (2.5%). The cat was then placed in a stereotaxic frame system (Unimecanique, France). Carbon dioxide concentration in expired gases and heart rhythm were controlled and body temperature was kept at 37°C during the experiment. The surgical procedure for implantation of brain electrodes was made using an operating microscope. The skull was exposed and cleaned. Three stainless steel anchoring screws (2 × 5 mm) were fixed to the skull and two ipsilateral burr holes (2–3 mm diameter) were made in the skull overlying the striatum and the MFB on the left side hemisphere.
The recording carbon-fiber microelectrode was first implanted in the left striatum 16.0 mm anterior to the interaural bar, 5.0 mm lateral to midline and 12.0 mm from the dura (Jasper and Ajmone-Marsan 1954). The microelectrode was connected to a pulse voltammetric system (Biopulse, SOLEA Tacussel, France). The oxidation potential for DA was first determined with DNPV (about 80 mV) and the oxidation current was monitored every second with differential pulse amperometry (DPA; Gonon 1988). Electrical stimulations of the MFB were applied through a bipolar electrode connected to an optically isolated stimulator (A-M system, USA). The bipolar electrode was implanted ipsilateral to the carbon-fiber electrode, 10.0 mm anterior to the interaural bar, 3.2 mm lateral from the midline, and 23.0 mm below the dura. A train of biphasic constant current square wave with a pulse duration of 0.5 msec and an amplitude of 450 μA was applied to the stimulating electrode (20 pulses every second, 40 Hz in frequency). To optimize the position of the stimulating electrode, it was progressively lowered until a maximal evoked release of DA was observed in the striatum (Kuhr et al. 1984).
Electrical stimulations of different duration (15 s, 30 s, and 45 s) were applied to the MFB, at 5-min intervals, and concomitant changes in extracellular DA concentration were recorded. When a reproducible signal was obtained following each electrical stimulation, the carbon-fiber microelectrode was retracted and the assembly of fixing screws and stimulating electrode was embedded in dental cement and allowed to dry. The cat was allowed to regain consciousness, care being taken to ensure maintenance of body temperature and rehydration. The cat was then allowed to recover from surgery for two weeks before to participate to PET experiments.
Extracellular concentration of DA at baseline was obtained by converting the peak current obtained using DNPV to concentration, based on precalibration of the carbon-fiber microelectrode in PBS containing 50 nM DA.
PET Studies
PET System
PET studies were performed on a Siemens ECAT Exact HR+ used in 3-dimensional mode. The system covers an axial distance of 15.5 cm (Brix et al. 1997). The transaxial resolution of the reconstructed images is about 4.1 mm full width at half-maximum in the center. Transmission scans were acquired with three rotating 68Ge-68Ga sources and used to correct the emission scans for the attenuation of 511 keV photon rays through tissue and head support.
PET Examinations
Anesthesia of the cats was induced using either halothane (4%) or ketamine (50 mg/kg/h; i.m.). As soon as deep anesthesia was obtained, an endotracheal intubation was performed and anesthesia was then maintained with halothane (2.5%) or with ketamine (50 mg/kg/h; i.m.). Carbon dioxide concentration in expired gases, heart rhythm, and body temperature were continuously monitored. A head fixation system was used to secure a fixed and reproducible position of the cat's head during the PET measurements. The head fixation system consists in a stereotaxic holding device made with Plexiglas where ear-bars, orbital and hard palate pieces allowed a stereotaxic positioning of the head. The horizontal plane was defined as including the interaural axis and the infraorbital ridges. A cannula was inserted in the sural vein for radiotracer injection.
[11C]raclopride was synthesized as previously described by methylation of the desmethyl precursor using [11C]methyl iodide (Ehrin et al. 1987). [11C]raclopride (2 to 2.2 mCi) was injected as a bolus during 2 s immediately followed by a flush with 2 ml saline. In all PET experiments, except the ones performed to study the effect of MFB stimulations on radioligand binding, radioactivity was measured in a series of sequential time frames of increasing duration (from 30 s to 10 min). The total time for measurement of radioactivity in the brain was 67 min.
Scatchard Analysis
Two cats (cat #1 and cat #2) each participated to two experimental series of four or five PET experiments. The first experimental series was performed under halothane anesthesia and the second under ketamine anesthesia. In each experimental series, D2-receptor density and apparent affinity were determined from a Scatchard analysis of four or five PET experiments using [11C]raclopride with high (range: 350–650 Ci/mmol), intermediate (range: 131–218 Ci/mmol) and low specific radioactivity (SR) (range: 38–65 Ci/mmol). All PET experiments were performed on different experimental days with at least one week apart.
Pretreatment with d-Amphetamine Sulfate
Two cats (cat #1 and cat #3) were each examined on two experimental days. On the first experimental day, two PET experiments were performed using [11C]raclopride before and after pretreatment with amphetamine (2 mg/kg; i.v.) under halothane anesthesia. On the second experimental day, the same protocol was repeated but under ketamine anesthesia. The period between the first and second experimental day was at least two weeks.
Electrical Stimulations of the MFB
Two weeks after surgery, the cat (cat #4) chronically implanted with a stimulating electrode was examined using PET on three experimental days. On the first experimental day, two PET experiments were performed using [11C]raclopride under ketamine anesthesia: the first was performed at basal conditions; during the second experiment, two 45-s stimulations (450 mA; 40 Hz) of the MFB were applied. One week later, the same protocol was repeated but under halothane anesthesia. Two weeks later, the same protocol was repeated once again under ketamine anesthesia.
In these experiments, the scanning protocol was adapted to allow detection of potential changes in [11C]raclopride binding following stimulation of the MFB. Indeed, if such changes occurred, they should be rapid and transient, reflecting the rapid and transient changes in DA levels induced by the stimulation. Temporal course data obtained with voltammetry on changes in DA levels following MFB stimulation were used to define the optimal scanning frame sequence. On the first experimental day, radioactivity was measured in a series of sequential time-frames of increasing duration (from 30 s to 3 min) for the first 19 min following [11C]raclopride administration. From 19 to 40 min, the time-frames were shortened to 1.5 min. Thereafter the time-frames were increased to 3 min until the end of the experiment. The first and second MFB stimulations were initiated at 19 and 28 min following [11C]raclopride administration, respectively. On the second and third experimental days, the scanning frame sequence was slightly modified: a series of sequential time-frames of increasing duration (from 30 s to 3 min) was used for the first 19 min, time-frames were shortened to 1 min from 19 to 36 min, and subsequently increased to 3 min until the end of the experiment. The first and second MFB stimulations were initiated at 20 and 30 min following [11C]raclopride administration, respectively. The total time for measurement of radioactivity in the brain was 70 min
In each experiment, the difference between time-activity curves obtained in the non-stimulated striatum (right side) and the stimulated striatum (left side) was calculated. For each set of experiments, the difference between time-activity curves obtained at baseline was compared with the difference between time-activity curves obtained when stimulations were applied using a repeated-measures analysis of variance (ANOVA). Significance was tested on data acquired between 10 and 45 min following radioligand injection.
Data Analysis
Regions of interest (ROI) for the right and left striatum and the cerebellum were drawn on the reconstructed PET images according to an atlas of the cat brain (Jasper and Ajmone-Marsan 1954). Regional radioactivity concentration (nCi/ml) was determined for each frame, corrected for decay and plotted versus time.
In all experiments except in the Scatchard experiments, quantification of [11C]raclopride binding potentials (BP) was performed using the simplified reference tissue model developed by Lammertsma and Hume (1996). In this approach, the time-activity curves in a reference region such as cerebellum is used as an indirect input function to estimate the free radioligand concentration and non-specific binding in brain. The major assumptions of this approach are that the exchange rates between the non-displaceable and specific compartments are so fast that they are combined in one single compartment, and the distribution volume in the reference region is the same than in the target regions. An expression relating radioligand concentration in a target region to the radioligand concentration in the reference region can be derived, which includes BP. Best estimates of BP values are obtained from non-linear least squares fitting analyses of the time-activity curves measured in the reference and in the target regions.
In the Scatchard experiments, quantification of [11C] raclopride binding was performed using the transient equilibrium method (Farde et al. 1989, 1990). Briefly, the time curve for specific radioligand binding (B(t)) was defined as the radioactivity in the striatum minus that in the cerebellum. A set of three exponential functions was fitted to the time curves for B(t) and F(t). Time for equilibrium was defined as the moment when B(t) peaked, i.e. dB/dt = 0. The value of B and F obtained at equilibrium was divided by the SR of injected [11C]raclopride to obtain the specifically bound radioligand concentration (B; pmol/ml) and the free radioligand concentration (F; pmol/ml). The B/F ratios obtained for each experiment were plotted versus B in a Scatchard graph and a straight line was drawn through the plotted points. The receptor density (Bmax) is defined at the intercept with the X axis and the apparent equilibrium dissociation constant (KDapp) by the inverse of the slope. The apparent equilibrium dissociation constant is given by the equation:  where KD is the equilibrium dissociation constant, [DA] is the concentration of endogenous DA in the extracellular space and KDA is the dissociation constant of DA for radioligand binding.
where KD is the equilibrium dissociation constant, [DA] is the concentration of endogenous DA in the extracellular space and KDA is the dissociation constant of DA for radioligand binding.
RESULTS
Comparison of [11C]raclopride Binding under Halothane and Ketamine Anesthesia
Figure 1 shows the time-activity curves of [11C]raclopride binding in the striatum of two cats (cat #1 and cat #2) anesthetized with either halothane or ketamine. In each cat, uptake of radioactivity in cerebellum was similar when both anesthetic conditions were compared. In the striatum, uptake of radioactivity initially increased, reached a maximal level within 30 min following radioligand injection and then decreased slowly with time. When comparing [11C]raclopride binding in the striatum of two cats, radioligand BP was 13 and 21% lower under ketamine than under halothane anesthesia, in cat #1 and cat #2, respectively.
Comparison of regional time-radioactivity curves obtained in two different cats (cat #1 and cat #2) after i.v. injection of [11C]raclopride. Each cat was examined under either halothane (closed symbols) or ketamine (open symbols) anesthesia. All time-activity curves are normalized to an injected dose of 2 mCi.
Scatchard Analyses
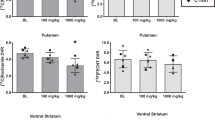
The Scatchard analyses indicated that the higher BP observed under halothane as compared with ketamine anesthesia reflected a lower KDapp, and thus a higher apparent affinity (Figure 2 ). In the first cat (cat #1), KDapp values were 8.3 nM (standard error of estimated parameter in linear regression, SE = 1.4) under halothane and 11.0 nM (SE = 0.8) under ketamine anesthesia. In the second cat (cat #2), KDapp values were 9.2 nM (SE = 0.9) under halothane and 11.7 nM (SE = 1.0) under ketamine anesthesia. No differences in Bmax were observed between the two anesthetic conditions. In cat #1, Bmax values were 25.6 pmol/ml (SE = 0.6) and 25.5 pmol/ml (SE = 0.5) under halothane and ketamine anesthesia, respectively. In cat #2, Bmax values were 28.3 pmol/ml (SE = 0.5) and 26.3 pmol/ml (SE = 0.7) under halothane and ketamine anesthesia, respectively.
Amphetamine Challenge
The effect of amphetamine-induced increase in endogenous DA levels on [11C]raclopride binding was investigated in the striatum of two cats (cat #1 and cat #3) anesthetized with either ketamine or halothane. A decrease in radioligand binding was observed in the striatum of the two cats under ketamine anesthesia as compared with baseline (Figure 3 ). There was no evident effect of amphetamine on radioactivity in the cerebellum. [11C]raclopride BP was decreased by 15% and 26% in cat #1 and cat #3, respectively. In contrast, amphetamine pretreatment did not produce any detectable changes in radioligand binding under halothane anesthesia (Figure 4 ).
Regional time-radioactivity curves (nCi/ml) ob- tained in two different cats (cat #1 and cat #3) after i.v. injection of [11C]raclopride at baseline conditions (plain symbols) and 30 min following a single dose of d-amphetamine sulfate (2 mg/kg; i.v.) (open symbols). Experiments were performed under ketamine anesthesia. All time-activity curves are normalized to an injected dose of 2 mCi.
Regional time-radioactivity curves (nCi/ml) ob- tained in two different cats (cat #1 and cat #3) after i.v. injection of [11C]raclopride at baseline conditions (plain symbols) and 30 min following a single dose of d-amphetamine sulfate (2 mg/kg; i.v.) (open symbols). Experiments were performed under halothane anesthesia. All time-activity curves are normalized to an injected dose of 2 mCi.
Voltammetry Measures of DA Overflow Following MFB Stimulation
The basal extracellular concentration of DA measured in the striatum of cat #4 was 15 nM. Figure 5 shows representative DA overflow curves in the striatum following MFB electrical stimulations of varying duration. Each stimulation caused a massive release of DA in the striatum, followed by a rapid clearance of released DA from the extracellular space. DA overflow was closely time-correlated with the stimulation: DA overflow began with the stimulation and stopped when stimulation was ceased. DA levels subsequently returned to baseline value within the next 5 min. Increasing stimulation duration from 15 to 45 s resulted in an increase in the duration and amplitude of DA overflow.
Kinetics of the DA overflow evoked by MFB electrical stimulations in the striatum of a cat (cat #4).The DA overflow evoked by MFB electrical stimulations (450 mA, 40 Hz) was electrochemically monitored using voltammetry. The figure shows representative recordings. Note that increasing stimulation duration resulted in an increase in DA overflow and that DA was quickly eliminated after each stimulation. Voltammetry measurements were performed under halothane anesthesia.
Effect of MFB Stimulation on [11C]raclopride Binding
The effect of transient stimulation-induced changes in striatal DA levels on [11C]raclopride binding was investigated in the same cat (cat #4) under ketamine and under halothane anesthesia. At baseline, the time-activity data obtained in the left striatum were similar to those obtained in the contralateral structure under both ketamine (Figure 6 , panels A and C) and halothane (Figure 7 ) anesthesia. Under ketamine anesthesia, when two 45-s stimulations of the nigrostriatal ascending fibers were applied during the PET measurement, each stimulation induced concomitant changes in [11C]raclopride binding in the ipsilateral striatum as compared with the contralateral side (Figure 6, panels B and D). The difference between time-activity curves in the right and left striatum was statistically different from that obtained at baseline (Figure 6, panels A and B; repeated-measures ANOVA: F1,34 = 19.05, p < .001; Figure 6, panels C and D; repeated-measures ANOVA: F1,42 = 6.97, p < .02). For each stimulation, radioligand binding levels in the ipsilateral striatum first decreased as compared with levels measured in the non-stimulated contralateral structure and then returned to contralateral levels. The stimulation-induced changes in radioligand binding thus showed an opposite but similar temporal pattern to the stimulation-induced changes in DA overflow measured with voltammetry (Figure 5). Moreover, a small but detectable increase in [11C]raclopride binding was observed in the contralateral structure (Figure 6, panel D).
Effect of transient changes in striatal DA levels induced by direct axonal stimulation on [11C]raclopride binding in the striatum of a cat (cat #4). Panel A shows regional time-radioactivity curves (nCi/ml) for [11C]raclopride binding in the cerebellum and in the right and left striatum at baseline conditions. Panel B shows regional time-radioactivity curves obtained 2 h later in the same animal but when two unilateral electrical stimulations (left side; 450 mA, 40 Hz) of the nigrostriatal fibers were applied during the PET measurements through a bipolar electrode chronically implanted in the MFB. The same set of experiments were repeated in the same animal two weeks later and are presented in panels C and D. Note that each axonal stimulation induced significant transient changes in [11C]raclopride binding in the ipsilateral striatum as compared with the contralateral side (panel A and B; repeated-measures ANOVA: F1,34 = 19.05, p < .001; panel C and D; ANOVA: repeated-measures ANOVA: F1,42 = 6.97, p < .02). Experiments were performed under ketamine anesthesia. All time-activity curves are normalized to an injected dose of 2 mCi.
Regional time-radioactivity curves (nCi/ml) for [11C]raclopride binding in the cerebellum and in the right and left striatum obtained in a cat at baseline conditions (left panel) and when two unilateral electrical stimulations (left side; 450 mA, 40 Hz) of the nigrostriatal fibers were applied during the PET measurements (right panel). No significant stimulation-induced change in [11C]raclopride binding was observed in the ipsilateral striatum as compared with the contralateral side (repeated-measures ANOVA: F1,42 = 0.77; p = .38). Experiments were performed under halothane anesthesia. All time-activity curves are normalized to an injected dose of 2 mCi.
As observed after amphetamine pretreatment, changes in DA levels induced by MFB stimulation did not produced detectable changes in [11C]raclopride binding under halothane anesthesia (Figure 7; repeated-measures ANOVA: F1,42 = 0.77; p = .38).
DISCUSSION
The present study further supports the view that competition with endogenous DA is not the only factor to play a significant role in the alterations of [11C]raclopride binding observed following DA manipulations in vivo. Three observations strongly suggest that changes in the intrinsic affinity of endogenous DA for D2-receptors might also affect [11C]raclopride binding. First, basal [11C]raclopride binding in the striatum was lower under ketamine than under halothane anesthesia. This observation is concordant with Kobayashi et al. (1995) who reported that [11C]raclopride binding was higher under isoflurane than under ketamine anesthesia in rhesus monkeys. Decreased levels of endogenous DA under halothane as compared with ketamine anesthesia are not likely to explain the differences in [11C]raclopride binding observed between the two anesthetic conditions. No data in the literature support this hypothesis. In contrast, a number of studies have consistently shown that halothane increases striatal DA levels (Ford and Marsden 1986; Savaki et al. 1986; Spampinato et al. 1986; Osborne et al. 1990; Stahle et al. 1990; Miyano et al. 1993; Mantz et al. 1994; Shiraishi et al. 1997; Keita et al. 1999) whereas ketamine has no effect (Ylitalo et al. 1976; Koshikawa et al. 1988; Lannes et al. 1991; Micheletti et al. 1992; Onoe et al. 1994; Mantz et al. 1994; Irifune et al. 1997; Tsukada et al. 2000).
Second, evaluation of [11C]raclopride binding parameters under both anesthetic conditions revealed that the higher radioligand binding observed under halothane anesthesia was not attributable to a higher density of striatal D2-receptors but to a higher apparent affinity. As seen in equation 1, KDapp, which is inversely related to the apparent affinity of the radioligand, is determined by both the concentration of extracellular DA and the inhibition constant of DA for radioligand binding. In other words, changes in KDapp can either reflect changes in extracellular DA levels or changes in the intrinsic affinity of DA for receptors, or both. The higher apparent affinity of [11C]raclopride under halothane anesthesia could reflect a decreased intrinsic affinity of DA, and in consequence, a decreased competition with endogenous DA. Conversely, the lower apparent affinity of [11C]raclopride under ketamine anesthesia could also reflect an increased intrinsic affinity of DA. Previous studies have shown that ketamine decreased the striatal binding of [11C]raclopride in human subjects (Breier et al. 1998; Smith et al. 1998). A subsequent study in non-human primates showed that this ketamine-induced decrease in [11C]raclopride binding was not due to change in extracellular DA concentration as measured with microdialysis (Tsukada et al. 2000). This latter study thus suggests that an increase in D2-receptor intrinsic affinity might be involved in the ketamine-induced alteration of [11C]raclopride binding in vivo. However, it is difficult at this stage to discriminate from our results whether [11C]raclopride binding is increased under halothane anesthesia or whether it is decreased under ketamine anesthesia (or both) since no data on [11C]raclopride binding levels in the awake state are available in our study for comparison.
Third, analysis of amphetamine pretreatment on striatal [11C]raclopride binding gave different results when the two anesthetic conditions were compared. Amphetamine pretreatment induced a significant decrease in [11C]raclopride binding under ketamine anesthesia, with a magnitude similar to that previously reported in nonhuman primates (Hartvig et al. 1997; Dewey et al. 1993). The same pretreatment did not produce detectable changes in [11C]raclopride binding under halothane anesthesia. Previous studies in rodents and humans have shown a marked enhancement of amphetamine-induced DA release by pretreatment by MK801 and ketamine, suggesting that amphetamine pretreatment may have a larger effect on [11C]raclopride binding under ketamine as compared with halothane anesthesia (Miller and Abercrombie 1996; Kegeles et al. 2000). However, amphetamine has also been reliably shown to cause a several-fold elevation in DA levels under halothane anesthesia (Zetterstrom et al. 1986; Fink-Jensen et al. 1994). So, even if lower, the effect of amphetamine on [11C]raclopride binding should still be detected under halothane anesthesia. Our results rather showed that competition between endogenous DA and [11C]raclopride for binding on D2-receptors can be evidenced in vivo using ketamine but not using halothane anesthesia. A similar conclusion can be drawn from our third set of experiments.
In the third set of experiments, striatal DA release was evoked by electrical stimulations of the MFB. The stimulation frequency used in this study (40 Hz) is high when compared with the firing frequency of DA neurons in vivo. Electrophysiological studies have shown that most of the nigrostriatal neurons have a slow firing rate (from 0 to 6 spikes/sec). In addition, some neurons fire with a burst activity and the maximal spike frequency within the bursts reaches 20 Hz (Grace and Bunney 1984; Freeman and Bunney 1987). In the present exploratory study we choose to apply high frequency stimulations because they were shown to be the most effective to induce striatal DA overflow in vivo and to enhance DA extracellular concentration up to 10 μM (Gonon and Buda 1985). We verified that, in our experimental conditions, high frequency unilateral stimulations of the MFB induced transient DA overflows in the ipsilateral striatum. In ketamine-anesthetized cat, such stimulations induced transient decreases in [11C]raclopride binding in the ipsilateral striatum, with a temporal course that mirrored the changes in DA levels. Moreover, a small increase in [11C]raclopride binding was also observed in the contralateral structure. This latter result is concordant with a previous study showing that unilateral activation of nigrostriatal pathway is accompanied by a concomitant inhibition of the contralateral pathway (Leviel et al. 1979). The stimulation-induced decreases in radioligand binding likely reflect changes in extracellular DA levels rather than alterations in cerebral blood flow (CBF). Simultaneous measurements of DA levels and oxygen consumption in the rat striatum have shown an elevation of local CBF during stimulation of the MFB in vivo (Zimmerman et al. 1992). In another study, Chugani et al. (1988) showed that CBF was not altered in the striatum following electrical nigrostriatal stimulations as measured with [14C]iodoantipyrine. Although it is difficult to draw conclusions from these two conflicting studies it is reasonable to assume that MFB stimulations, by activating dopaminergic neurons, might increase CBF to these neurons, if any effect is assumed. This would increase delivery of the tracer to these neurons and therefore increase radiotracer binding, thus possibly offsetting the inhibitory effect of endogenous DA competition. That is, blood flow effect would have an opposite effect on radioligand binding as compared with the competitive effect of DA. The decreased radioligand binding observed in ketamine-anesthetized animals during stimulation cannot thus be ascribed to changes in CBF and more likely reflect changes in extracellular DA levels. As observed after amphetamine pretreatment, the stimulation-induced changes in DA levels did not produced detectable changes in [11C]raclopride binding under halothane anesthesia.
The failure to detect DA competition under halothane anesthesia leads us to speculate that the intrinsic affinity of D2-receptors for DA under halothane is too low to observe such a phenomenon in vivo. The dopamine D2-receptor exists in a high and a low-affinity state for DA (D2-high and D2-low; Sibley et al. 1982; Gingrich and Caron 1993). The high-affinity state is believed to arise from coupling with a G protein and is disrupted by the addition of GTP in vitro (Wreggett and Seeman 1984). DA has a 1,000 fold higher affinity for the D2-high than for the D2-low sites, while [11C]raclopride binds to both sites with the same affinity (Seeman et al. 1994). The overall affinity of DA for D2-receptors thus strongly depends on the ratio of D2-high to D2-low sites. We proposed that this ratio might be different under ketamine and halothane anesthesia. D2-low sites would be in a large majority under halothane and DA would be unable to compete with [11C]raclopride for binding on these sites. This hypothesis is supported by a number of radioligand binding studies showing that halothane converts several G protein-coupled receptors to states of lower agonist affinity by interfering with receptor-G protein interactions. For example, Martin et al. (1991) have shown that halothane inhibits [3H]8-OH-DPAT agonist binding to serotonin 5HT1A receptors in rat hippocampal membranes and [3H]CHA agonist binding to adenosine A1-receptors in rat forebrain membranes. Similarly, halothane decreased the high affinity binding of the agonist [3H]oxotremorine to muscarinic receptors in rat brainstem membranes (Dennison et al. 1987) without affecting the number of muscarinic antagonist binding sites (Aronstam et al. 1986). In mouse cortical membranes, halothane was shown to decrease the agonist affinity of [3H]clonidine for the α2-receptors without affecting the number of binding sites (Wikberg et al. 1987). In vitro binding experiments performed on rat and human myocardium membranes also reliably showed that halothane, but not isoflurane, shifts the β-adrenoreceptor from its high- to low-agonist affinity state (Bohm et al. 1993; Schotten et al. 1998) and that the decrease in agonist affinity binding was not accompanied by changes in β-adrenoreceptors density (Bernstein et al. 1981; Schotten et al. 1993). Only limited data are available that might explain the molecular mechanisms by which halothane promotes the conversion of G-protein coupled receptors from their high to their low agonist affinity state. However, it appears from the aforementioned studies that this effect is not receptor-specific and rather occurs throughout the brain. This observation is concordant with a recent study which revealed that [14C]halothane binds to specific binding sites that are widespread within the brain but appear to be located in region of high synaptic density (Eckenhoff and Eckenhoff 1998). It is thus possible that halothane, as observed in other systems, has analogous effects on dopamine D2-receptors and promotes their conversion to states of lower agonist affinity.
A striking observation was the remarkable spatiotemporal concordance between changes in striatal DA levels as measured with voltammetry and changes in [11C]raclopride binding as measured with PET in ketamine-anesthetized cat. [11C]raclopride binding decreased as long as the stimulation was applied suggesting a rapid radioligand dissociation from the receptors. Once the stimulation was ceased, radioligand reassociated to receptors as DA concentration fell, presumably from the pool of free radioligand still available for re-binding. The observation of [11C]raclopride reassociation is consistent with the view that changes in radioligand binding primarily reflect changes in DA occupancy of the D2-receptors. Our experimental data support the view that [11C]raclopride binding kinetics (i.e. association and dissociation constants) are fast enough to follow transient changes in DA levels and contrast with the prolonged decrease in [11C]raclopride and [123I]IBZM bindings reported following amphetamine challenge (Carson et al. 2000; Laruelle et al. 1997). It is possible that this long-lasting effect of amphetamine reflects an agonist-mediated internalization of D2-receptors leading to a decreased receptor density at the cell surface. Such a mechanism has already been proposed to explain the changes in D2-radioligand binding observed following manipulations of the DA system in vivo (Chugani et al. 1988). We postulate that the long-lasting changes in [11C]raclopride binding observed following amphetamine challenge reflect a D2-receptor internalization triggered by sustained (1 to 2 h) agonist stimulation while transient (few minutes) increase in synaptic DA induced by axon stimulation is too short to trigger such a phenomenon.
The present study showed that increases in synaptic DA levels do not always correlate with opposite changes in [11C]raclopride binding. The failure to detect such a correlation under halothane anesthesia might reflect, as already reported for other brain receptor systems, a halothane-promoted conversion of D2-receptors to states of lower affinity for DA. In addition, previous data in the literature suggest that D2-receptor intrinsic affinity might also be, in contrast, increased under ketamine anesthesia (Tsukada et al. 2000). It is suggested that the agonist affinity state of the receptor is a factor that should be considered in in vivo ligand-activation studies, especially those performed in psychiatric conditions such as schizophrenia in which hyperdopaminergia is postulated. Difference in the affinity state of receptors under pathological conditions could make it difficult to compare the effect of pharmacological manipulation between patients and control subjects. A higher proportion of high affinity D2-receptor sites in schizophrenics might, for example, underlie the higher DA-radioligand competition found in patients as compared with controls following amphetamine challenge, as opposed to the postulated elevated release of endogenous DA (Laruelle et al. 1996; Breier et al. 1997). Since DA is not expected to compete with D2-receptors in the low affinity state, a higher proportion of D2-receptors in the high-affinity state in schizophrenics would imply that a higher number of D2-receptors are vulnerable to competition with endogenous DA. Consequently, similar increases in endogenous DA above baseline levels should induce more pronounced decreases in [11C]raclopride binding in schizophrenics as compared with controls.
Future studies are thus needed to disentangle whether differences in in vivo radioligand apparent affinity found between experimental conditions or between groups of subjects only reflect differences in endogenous neurotransmitter levels or can also be accounted by differences in the affinity state of the targeted receptors. The development of suitable in vivo agonist radioligands for the D2-receptor could lead to studies aiming at the measurements of the high and low affinity sites populations. Such studies would make profound contributions to the understanding of DA neurotransmission in the living human brain.
References
Aronstam RS, Anthony BL, Dennison RL Jr . (1986): Halothane effects on muscarinic acetylcholine receptor complexes in rat brain. Biochem Pharmacol 35: 667–672
Baudry M, Martres MP, Schwartz JC . (1977): In vivo binding of 3H-pimozide in mouse striatum: effects of dopamine agonists and antagonists. Life Sci 21: 1163–1170
Bernstein KJ, Gangat Y, Verosky M, Vulliemoz Y, Triner L . (1981): Halothane effect on beta-adrenergic receptors in canine myocardium. Anesth Analg 60: 401–405
Bischoff S, Gunst F . (1997): Distinct binding patterns of [3H]raclopride and [3H]spiperone at dopamine D2 receptors in vivo in rat brain. Implications for pet studies. J Recept Signal Transduct Res 17: 419–431
Bohm M, Schmidt U, Schwinger RH, Bohm S, Erdmann E . (1993): Effects of halothane on beta-adrenoceptors and M-cholinoceptors in human myocardium: radioligand binding and functional studies. J Cardiov Pharmacol 21: 296–304
Breier A, Su TP, Saunders R, Carson RE, Kolachana BS, deBartolomeis A, Weinberger DR, Weisenfeld N, Malhotra AK, Eckelman WC, Pickar D . (1997): Schizophrenia is associated with elevated amphetamine-induced synaptic dopamine concentrations: evidence from a novel positron emission tomography method. Proc Natl Acad Sci USA 94: 2569–2574
Breier A, Adler CM, Weisenfeld N, Su TP, Elman I, Picken L, Malhotra AK, Pickar D . (1998): Effects of NMDA antagonism on striatal dopamine release in healthy subjects: application of a novel PET approach. Synapse 29: 142–147
Brix G, Zaers J, Adam LE, Bellemann ME, Ostertag H, Trojan H, Haberkorn U, Doll J, Oberdorfer F, Lorenz WJ . (1997): Performance evaluation of a whole-body PET scanner using the NEMA protocol. National Electrical Manufacturers Association. J Nucl Med 38: 1614–1623
Butcher SP, Fairbrother IS, Kelly JS, Arbuthnott GW . (1988): Amphetamine-induced dopamine release in the rat striatum: an in vivo microdialysis study. J Neurochem 50: 346–355
Carson RE, Channing MA, Vuong B-K, Watabe H Herscovitch, Eckelman WC . (2000): Amphetamine-induced dopamine release: duration of action assessed with [11C]raclopride in anesthetized monkeys. In Gjedde A, Hansen SB, Knudsen GM, Paulson OB (eds), Physiological Imaging of the Brain with PET. London, Academic Press, pp 205–209
Chergui K, Suaud-Chagny MF, Gonon F . (1994): Nonlinear relationship between impulse flow, dopamine release and dopamine elimination in the rat brain in vivo. Neuroscience 62: 641–645
Chugani DC, Ackermann RF, Phelps ME . (1988): In vivo [3H]spiperone binding: evidence for accumulation in corpus striatum by agonist-mediated receptor internalization. J Cereb Blood Flow Metab 8: 291–303
Dennison RL, Anthony BL, Narayanan TK, Aronstam RS . (1987): Effects of halothane on high affinity agonist binding and guanine nucleotide sensitivity of muscarinic acetylcholine receptors from brainstem rat. Neuropharmacol 26: 1201–1205
Dewey SL, Smith GS, Logan J, Brodie JD, Fowler JS, Wolf AP . (1993): Striatal binding of the PET ligand 11C-raclopride is altered by drugs that modify synaptic dopamine levels. Synapse 13: 350–356
Dewey SL, Smith GS, Logan J, Alexoff D, Ding YS, King P, Pappas N, Brodie JD, Ashby CR Jr . (1995): Serotonergic modulation of striatal dopamine measured with positron emission tomography (PET) and in vivo microdialysis. J Neuroscience 15: 821–829
Dugast C, Suaud-Chagny MF, Gonon F . (1994): Continuous in vivo monitoring of evoked dopamine release in the rat nucleus accumbens by amperometry. Neuroscience 62: 647–654
Eckenhoff MF, Eckenhoff RG . (1998): Quantitative autoradiography of halothane binding in rat brain. J Pharmacol Exp Ther 285: 371–376
Ehrin E, Gawell L, Högberg T, de Paulis T, Ström P . (1987): Synthesis of [Methoxy-3H]- and [Methoxy-11C]- labelled raclopride. Specific dopamine-D2 receptor ligands. J Labelled Compd Radiopharm 24: 931–940
Farde L, Eriksson L, Blomqvist G, Halldin C . (1989): Kinetic analysis of central [11C]raclopride binding to D2-dopamine receptors studied by PET - A comparison to the equilibrium analysis. J Cereb Blood Flow Metab 9: 696–708
Farde L, Wiesel FA, Stone-Elander S, Halldin C, Nordstrom AL, Hall H, Sedvall G . (1990): D2 dopamine receptors in neuroleptic-naïve schizophrenic patients. A positron emission tomography study with [11C]raclopride. Arch Gen Psychiatry 47: 213–219
Fink-Jensen A, Ingwersen SH, Nielsen PG, Hansen L, Nielsen EB, Hansen AJ . (1994): Halothane anesthesia enhances the effect of dopamine uptake inhibition on interstitial levels of striatal dopamine. Naunyn Schmiedebergs Arch Pharmacol 350: 239–244
Ford AP, Marsden CA . (1986): Influence of anaesthetics on rat striatal dopamine metabolism in vivo. Brain Res 379: 162–166
Freeman AS, Bunney BS . (1987): Activity of A9 and A10 dopaminergic neurons in unrestrained rats: further characterization and effects of apomorphine and cholecystokinin. Brain Res 405: 46–55
Gingrich JA, Caron MG . (1993): Recent advances in the molecular biology of dopamine receptors. Ann Rev Neurosci 16: 299–321
Ginovart N, Farde L, Halldin C, Swahn CG . (1997): Effect of reserpine-induced depletion of synaptic dopamine on [11C]raclopride binding to D2-dopamine receptors in the monkey brain. Synapse 25: 321–325
Gonon F, Navarre F, Buda M . (1984): In vivo monitoring of dopamine release in the rat brain with differential normal pulse voltammetry. Anal Chem 56: 573–575
Gonon F, Buda M . (1985): Regulation of dopamine release by impulse flow and by autoreceptors as studied by in vivo voltammetry in the rat striatum. Neuroscience 14: 765–774
Gonon F . (1988): Non linear relationship between impulse flow and dopamine released by rat midbrain dopaminergic neurons as studied by in vivo electrochemistry. Neuroscience 24: 19–28
Grace AA, Bunney BS . (1984): The control of firing pattern in nigral dopamine neurons: burst firing. J Neurosci 4: 2877–2890
Hall H, Wedel I, Halldin C, Kopp J, Farde L . (1990): Comparison of the in vitro receptor binding properties of N- [3H]methylspiperone and [3H]raclopride to rat and human brain membranes. J Neurochem 55: 2048–2057
Hartvig P, Torstenson R, Tedroff J, Watanabe Y, Fasth KJ, Bjurling P, Langstrom B . (1997): Amphetamine effects on dopamine release and synthesis rate studied in the Rhesus monkey brain by positron emission tomography. J Neural Transm 104: 329–339
Innis RB, Malison RT, al-Tikriti M, Hoffer PB, Sybirska EH, Seibyl JP, Zoghbi SS, Baldwin RM, Laruelle M, Smith EO, Charney DS, Heninger G, Elsworth JD, Roth JH . (1992): Amphetamine-stimulated dopamine release competes in vivo for [123I]IBZM binding to the D2 receptor in nonhuman primates. Synapse 10: 177–184
Irifune M, Fukuda T, Nomoto M, Sato T, Kamata Y, Nishikawa T, Mietani W, Yokoyama K, Sugiyama K, Kawahara M . (1997): Effects of ketamine on dopamine metabolism during anesthesia in discrete brain regions in mice: comparison with the effects during the recovery and subanesthetic phases. Brain Res 763: 281–284
Jasper HH, Ajmone-Marsan C . (1954): A Stereotaxic Atlas of the Diencephalon of the Cat. The National Research Council of Canada, Ottawa, Canada
Keita H, Henzel-Rouelle D, Dupont H, Desmonts JM, Mantz J . (1999): Halothane and isoflurane increase spontaneous but reduce the N-methyl-D- aspartate-evoked dopamine release in rat striatal slices: evidence for direct presynaptic effects. Anesthesiology 91: 1788–1797
Kegeles LS, Abi-Dargham A, Zea-Ponce Y, Rodenhiser-Hill J, Mann JJ, Van Heertum RL, Cooper T B, Carlsson A, Laruelle M . (2000): Modulation of amphetamine-induced striatal dopamine release by ketamine in humans: implications for schizophrenia. Biol Psychiatry 48: 627–640
Kobayashi K, Onoue O, Watanabe Y, Onoe H, Langström B . (1995): Difference in response of D2 receptor binding between 11C-N-methylspiperone and 11C-raclopride against anesthetics in rhesus monkey brain. J Neural Transm 100: 147–151
Koshikawa N, Tomiyama K, Omiya K, Kobayashi M . (1988): Ketamine anaesthesia has no effect on striatal dopamine metabolism in rats. Brain Res 444: 394–396
Kuhr WG, Ewing AG, Caudill WL, Wightman RM . (1984): Monitoring the stimulated release of dopamine with in vivo voltammetry. I: Characterization of the response observed in the caudate nucleus of the rat. J Neurochem 43: 560–569
Lammertsma AA, Hume SP . (1996): Simplified reference tissue model for PET receptor studies. Neuroimage 4: 153–158
Lannes B, Micheletti G, Warter J, Kempf E, Di Scala G . (1991): Behavioural, pharmacological and biochemical effects of acute and chronic administration of ketamine in the rat. Neurosci Lett 128: 177–181
Laruelle M, Abi-Dargham A, Van Dyck CH, Gil R, D'Souza CD, Erdos J, McCance E, Rosenblatt W, Fingado C, Zoghbi SS, Baldwin RM, Seibyl JP, Krystal JH, Charney DS, Innis RB . (1996): Single photon emission computerized tomography imaging of amphetamine-induced dopamine release in drug-free schizophrenic subjects. Proc Natl Acad Sci USA 93: 9235–9240
Laruelle M, Iyer RN, Al-Tikriti MS, Zea-Ponce Y, Malisson R, Zoghbi SS, Baldwin RM, Kung HF, Charney DS, Hoffer PB, Innis RB . (1997): Microdialysis and SPECT measurements of amphetamine-induced dopamine release in nonhuman primates. Synapse 25: 1–14
Laruelle M . (2000): Imaging synaptic neurotransmission with in vivo binding competition techniques: a critical review. J Cereb Blood Flow Metab 20: 423–451
Leviel V, Cheramy A, Glowinski J . (1979): Role of the dendritic release of dopamine in the reciprocal control of the two nigro-striatal dopaminergic pathways. Nature 280: 236–239
Mantz J, Varlet C, Lecharny JB, Henzel D, Lenot P, Desmont JM . (1994): Effects of volatile anesthetics, thiopental, and ketamine on spontaneous and depolarization-evoked dopamine release from striatal synaptosomes in the rat. Anesthesiology 80: 352–363
Martin DC, Dennison RL, Introna RP, Aronstam RS . (1991): Influence of halothane on the interaction of serotonin1 and adenosine1 receptors with G protein in rat brain membranes. Biochem Pharmacol 42: 1313–1316
Micheletti G, Lannes B, Haby C, Borrelli E, Kempf E, Warter JM, Zwiller J . (1992): Chronic administration of NMDA antagonists induces D2 receptor synthesis in rat striatum. Brain Res Mol Brain Res 14: 363–368
Miller DW, Abercrombie ED . (1996): Effects of MK-801 on spontaneous and amphetamine-stimulated dopamine release in striatum measured with in vivo microdialysis in awake rats. Brain Res Bull 40: 57–62
Miyano K, Tanifuji Y, Eger EI . (1993): The effect of halothane dose on striatal dopamine: an in vivo microdialysis study. Brain Res 605: 342–344
Onoe H, Inoue O, Suzuki K, Tsukada H, Itoh T, Mataga N, Watanabe Y . (1994): Ketamine increases the striatal N-[11C]methylspiperone binding in vivo: positron emission tomography study using conscious rhesus monkey. Brain Res 663: 191–198
Osborne PG, O'Connor WT, Drew KL, Ungerstedt U . (1990): An in vivo microdialysis characterization of extracellular dopamine and GABA in dorsolateral striatum of awake freely moving and halothane anaesthetised rats. J Neurosci Methods 34: 99–105
Savaki HE, Girault JA, Spampinato U, Truong NA, Glowinski J, Besson MJ . (1986): Release of newly synthesized 3H-dopamine in the striatum: an adaptation of the push-pull cannula method to awake restrained and anesthetized rats. Brain Res Bull 16: 149–154
Schotten U, Schumacher C, Sigmund M, Rose H, Kammermeier H, Hanrath P . (1993): Beta-adrenoreceptor of isolated adult rat cardiomyocytes are not changed by halothane. Eur Heart J 14(Suppl): 299
Schotten U, Schumacher C, Sigmund M, Karlein C, Rose H, Kammermeier H, Sivarajan M, Hanrath P . (1998): Halothane, but not isoflurane, impairs the beta-adrenergic responsiveness in rat myocardium. Anesthesiology 88: 1330–1339
Seeman P, Guan HC, Niznik HB . (1989): Endogenous dopamine lowers the dopamine D2 receptor density as measured by [3H]raclopride: Implications for positron emission tomography of the human brain. Synapse 3: 96–97
Seeman P, Sunahara RK, Niznik HB . (1994): Receptor-receptor link in membranes revealed by ligand competition: example for dopamine D1 and D2 receptors. Synapse 17: 62–64
Sharp T, Zetterstrom T, Ljungberg T, Ungerstedt U . (1987): A direct comparison of amphetamine-induced behaviours and regional brain dopamine release in the rat using intracerebral dialysis. Brain Res 401: 322–330
Shiraishi M, Kamiyama Y, Huttemeier PC, Benveniste H . (1997): Extracellular glutamate and dopamine measured by microdialysis in the rat striatum during blockade of synaptic transmission in anesthetized and awake rats. Brain Res 759: 221–227
Sibley DR, de Lean A, Creese I . (1982): Anterior pituitary dopamine receptor. Demonstration of interconvertible high and low affinity states of the D2-dopamine receptor. J Biol Chem 257: 6351–6361
Smith GS, Schloesser R, Brodie JD, Dewey SL, Logan J, Vitkun SA, Simkowitz P, Hurley A, Cooper T, Volkow ND, Cancro R . (1998): Glutamate modulation of dopamine measured in vivo with positron emission tomography (PET) and 11C-raclopride in normal human subjects. Neuropsychopharmacol 18: 18–25
Spampinato U, Girault JA, Danguir J, Savaki HE, Glowinski J, Besson MJ . (1986): Apomorphine and haloperidol effects on striatal 3H-dopamine release in anesthetized, awake restrained and freely moving rats. Brain Res Bull 16: 161–166
Stahle L, Collin AK, Ungerstedt U . (1990): Effects of halothane anaesthesia on extracellular levels of dopamine, dihydroxyphenylacetic acid, homovanillic acid and 5-hydroxyindolacetic acid in rat striatum: a microdialysis study. Arch Pharmacol 342: 136–140
Tsukada H, Nishiyama S, Kakiuchi T, Ohba H, Sato K, Harada N, Nakanishi S . (1999): Isoflurane anesthesia enhances the inhibitory effects of cocaine and GBR12909 on dopamine transporter: Pet studies in combination with microdialysis in the monkey brain. Brain Res 849: 85–96
Tsukada H, Harada N, Nishiyama S, Ohba H, Sato K, Fukumoto D, Kakiuchi T . (2000): Ketamine decreased striatal [11C]raclopride binding with no alterations in static dopamine concentrations in the striatal extracellular fluid in the monkey brain: multi-parametric PET studies combined with microdialysis analysis. Synapse 37: 95–103
Wreggett KA, Seeman P . (1984): Agonist high and low affinity states of the D2 dopamine receptor in calf brain. Partial conversion by guanine nucleotide. Mol Pharmacol 25: 10–17
Wikberg JE, Hede AR, Post C . (1987): Effects of halothane and other chlorinated hydrocarbons on alpha-2 adrenoreceptors in the mouse cortex. Pharmacol Toxicol 61: 271–277
Ylitalo P, Saarnivaara L, Ahtee L . (1976): Effect of ketamine anaesthesia on the content of monoamines and their metabolites in the rat brain. Acta Anaesthesiol Scand 20: 216–220
Zetterstrom T, Sharp T, Ungerstedt U . (1986): Further evaluation of the mechanism by which amphetamine reduces striatal dopamine metabolism: a brain dialysis study. Eur J Pharmacol 132: 1–9
Zimmerman JB, Kennedy RT, Wightman RM . (1992): Evoked neuronal activity accompanied by transmitter release increases oxygen concentration in rat striatum in vivo but not in vitro. J Cereb Blood Flow Metab 12: 629–637
Acknowledgements
This work was supported by grants and fellowships (N.G.) from the Fondation de France and the France Parkinson foundations. The assistance of the members of the CERMEP group involved in the PET experiments is also gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ginovart, N., Hassoun, W., Le Cavorsin, M. et al. Effects of Amphetamine and Evoked Dopamine Release on [11C]raclopride Binding in Anesthetized Cats. Neuropsychopharmacol 27, 72–84 (2002). https://doi.org/10.1016/S0893-133X(02)00285-3
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1016/S0893-133X(02)00285-3
Keywords
This article is cited by
-
Amphetamine challenge decreases yohimbine binding to α2 adrenoceptors in Landrace pig brain
Psychopharmacology (2012)
-
Ventral Striatal Dopamine Release in Response to Smoking a Regular vs a Denicotinized Cigarette
Neuropsychopharmacology (2009)
-
Effect of Increased Serotonin Levels on [18F]MPPF Binding in Rat Brain: Fenfluramine vs the Combination of Citalopram and Ketanserin
Neuropsychopharmacology (2005)
-
Imaging the Dopamine System with In Vivo [11C]raclopride Displacement Studies: Understanding the True Mechanism
Molecular Imaging and Biology (2005)