Abstract
Aim: The sphygmomanometer is an essential piece of diagnostic equipment, used in many routine consultations in primary care. Its accuracy depends on correct maintenance and calibration. This study was designed to: (1) assess the maintenance and calibration of sphygmomanometers in use in primary care; (2) assess the clinical, ethical, legal and public health implications of our findings.
Method: A researcher assessed the accuracy of mercury and aneroid sphygmomanometers in use in 231 English general practices. He also made enquires about arrangements for the maintenance and calibration of sphygmomanometers. We conducted a small telephone survey in general practices across the country to determine maintenance and calibration arrangements across the country. We carried out a modelling exercise to explore the clinical, ethical and public health implications of our findings.
Results: Of 1462 sphygmomanometers, 9.2% gave readings were more than 5 mm Hg inaccurate. No practice had arrangements for maintenance and calibration of sphygmomanometers. Nationally, one of 54 practices had an arrangement for maintenance and calibration. True hypertension is very uncommon in women under 35, a blood pressure which is measured as high is much more likely to be caused by calibration error than by hypertension.
Conclusion: It is rare for sphygmomanometers used in primary care to be maintained and calibrated. Because of this women under 35 are at risk of misclassification and inappropriate treatment. This has ethical and public health implications. Clinicians using equipment which has not been maintained and calibrated may be medically negligent.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Specification for aneroid and mercury non-automated sphygmomanometers. BS2743: 1990, British Standards Institute, London
Hussain A, Cox JG An audit of the use of sphygmomanometers Br J Clin Pract 1996 50 136–137
Maskrey N, Parker C, Powell S THINYCE – Treating Hypertension Through Clinical Effectiveness in North Yorkshire, October 1998. North Yorkshire Clinical Advisory Service: North Yorkshire Health Authority
Cranney M, Barton S, Walley T Auditing the management of hypertension in British general practice: a critical literature review Br J Gen Pract 1998 48 1424–1428
Jones JS, Ramsey W, Hetrick T Accuracy of prehospital sphygmomanometers J Emergency Med 1987 5 23–27
Hahn LP, Folsom AR, Sprafka JM, Prineas RJ Prevalence and accuracy of home sphygmomanometers in an urban population Am J Pub Health 1987 77 1459–1461
Specification for Aneroid and mercury non-automated sphygmomanometers. BS2743: 1990, British Standards Institute, London
Ramsay LE et alBritish Hypertension Society guidelines for hypertension management 1999: summary BMJ 1999 319 630–635
Department of Health Health survey for England ’96 Stationery Office: London 1998
Reeves RA Does thispatient have hypertension? How to measure blood pressure J Am Med Assoc 1995 273 12118
van de Mheen PJ, Bonneux L, Gunning-Schepers LJ Variation in reported prevalences of hypertension in The Netherlands: the impact of methodological variables J Epidemiol Community Health 1995 49 277–280
McCarron P et alChanges in blood pressure among students attending Glasgow University between 1948 and 1968: analyses of cross sectional surveys BMJ 2001 322 885–889
Anderson KA, Wilson PWF, Odell PM, Kannel WB An updated coronary risk profile. A statement for health professionals Circulation 1991 83 356–362
Unwin N et alThe implications of applying widely accepted cholesterol screening and management guidelines to a British adult population: results from a cross sectional study of cardiovascular disease and risk factors BMJ 1998 317 1125–1130
Department of Health Health survey for England ’98 Stationery Office: London 2000
Acknowledgements
Thanks are due to Mr Brian Pritchard for carrying out the survey of sphygmomanometers.
Andrew Rouse obtained data on sphygmomanometer calibration error, made a crude estimate of the prevalence of misclassification error and contributed to writing the paper.
Tom Marshall developed models for estimating the prevalence of misclassification due to uncalibrated sphygmomanometer error and contributed to writing the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rouse, A., Marshall, T. The extent and implications of sphygmomanometer calibration error in primary care. J Hum Hypertens 15, 587–591 (2001). https://doi.org/10.1038/sj.jhh.1001241
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jhh.1001241
Keywords
This article is cited by
-
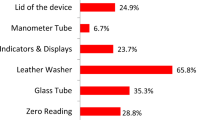
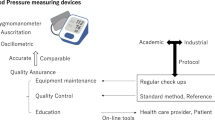
Results of a project to calibrate mercury sphygmomanometer blood pressure-measuring devices in Egypt
Journal of Human Hypertension (2021)
-
Predicted impact of various clinical practice strategies on cardiovascular risk for the treatment of hypertension: a clinical trial simulation study
Journal of Pharmacokinetics and Pharmacodynamics (2014)
-
Misclassification and discordance of measured blood pressure from patient’s true blood pressure in current clinical practice: a clinical trial simulation case study
Journal of Pharmacokinetics and Pharmacodynamics (2012)
-
Calibration accuracy of hospital-based non-invasive blood pressure measuring devices
Journal of Human Hypertension (2010)
-
Variation in recorded blood pressure terminal digit bias in general practice
Journal of Human Hypertension (2008)