Abstract
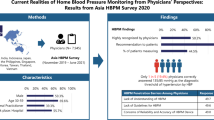
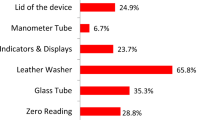
Obtaining accurate blood pressure readings is vital. However, students and health professionals do not always receive adequate training on blood pressure measurement, especially regarding new technologies, leading to insufficient knowledge. Therefore, the aim of this study is to analyze Brazilian health professionals’ perceptions and knowledge about automated blood pressure monitors. This cross-sectional study involved 1734 Brazilian nurses, nursing technicians, and doctors who reported having some experience of using automated monitors. Perceptions about differences between readings obtained through the auscultatory and oscillometric methods, influence of small differences in clinical decision-making, confidence in automated monitors, and knowledge about contraindications for the use of these devices were assessed. Most medical and nursing professionals considered differences of up to 5 mmHg (40.94%) between auscultatory and oscillometric measurements acceptable. Of these, 69.02% reported that even small differences can influence clinical decisions. Confidence in readings obtained using automated blood pressure monitors was reported by 53.92%. Among the motivations for making these devices available in health services, the most frequent was the saving of time (48.85%) and the least frequent, the perception that the use of this technology requires less training (9.40%). Arrhythmia was the most recognized contraindication for the use of automated monitors (28.49%), followed by obesity (28.14%) and blood pressure readings above 160 × 100 mmHg. In conclusion, there is a lack of knowledge about the functionalities and indications of blood pressure monitors and a low tolerance for measurements different from those obtained through manual mercury sphygmomanometers or aneroids.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Mansoor K, Shahnawaz S, Rasool M, Chaudhry H, Ahuja G, Shahanawaz S. Automated versus manual blood pressure measurement: a randomized crossover trial in the emergency department of a tertiary care hospital in Karachi, Pakistan: are third world countries ready for the change? Open Access Maced J Med Sci. 2016;4:404–9.
Myers MG, Kaczorowski J, Dawes M, Godwin M. Automated office blood pressure measurement in primary care. Can Fam Physician 2014;60:127–32.
González-López JJ, Ramírez JGA, García RT, Esteban AS, Barrio JÁ, Rodríguez-Artalejo F. Knowledge of correct blood pressure measurement procedures among medical and nursing students. Rev Esp Cardiol. 2009;62:568–71.
Crosley AM, Rose JRL. Knowledge of accurate blood pressure measurement procedures in chiropractic students. J Chiropr Educ 2013;27:152–7.
Hwang KO, Aigbe A, Ju HH, Jackson VC, Sedlock EW. Barriers to accurate blood pressure measurement in the medical office. J Prim Care Community Health. 2018;9:2150132718816929.
Myers MG, Valdivieso M, Kiss A. Use of automated office blood pressure measurement to reduce the white coat response. J Hypertens. 2009;27:280–6.
O’Brien E. Will mercury manometers soon be obsolete? J Hum Hypertens. 1995;9:933–334.
Markandu ND, Whitcher F, Arnold A, Carney C. The mercury sphygmomanometer should be abandoned before it is proscribed. J Hum Hypertens. 2000;14:31–36.
Varughese GI, Lip GYH. Goodbye mercury? Blood pressure measurement and its future. J R Soc Med. 2005;98:89–90.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the american college of cardiology/american heart association task force on clinical practice guidelines. Hypertension. 2018;71:e13–e115.
Williams B, Mancia G, Spiering W, Rosei EA, Azizi M, Burnier M, et al. The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur Heart J. 2018;39:3021–104.
World Medical Association. World medical association declaration of helsinki: ethical principles for medical research involving human subjects. JAMA 2013;310:2191–4.
O’Brien E, Petrie J, Littler WA, Swiet M, Padfield PL, Altman DG, et al. The British Hypertension Society protocol for the evaluation of blood pressure measuring devices. J Hypertens. 1993;11:S43–S63.
O’Brien O, Pickering T, Asmar R, Myers M, Parati G, Staessen J, et al. Working group on blood pressure monitoring of the european society of hypertension international protocol for validation of blood pressure measuring devices in adults. Blood Press Monit. 2002;7:3–17.
Non‐invasive sphygmomanometers – Part 2: clinical investigation of automated measurement type. American National Standards Institute. ANSI/AAMI/ISO 81060‐2; 2013. http://webstore.ansi.org. Accessed April 25, 2020.
Stergiou GS, Alpert B, Mieke S, Asmar R, Atkins N, Eckert S, et al. A universal standard for the validation of blood pressure measuring devices: Association for the Advancement of Medical Instrumentation/European Society of Hypertension/International Organization for Standardization (AAMI/ESH/ISO) Collaboration Statement. Hypertension 2018;71:368074.
Mirdamadi A, Etebari M. Comparison of manual versus automated blood pressure measurement in intensive care united, coronary care unit, and emergency room. ARYA Atheroscler. 2017;13:29–34.
Himmelfarb CR, Commodore-Mensah Y, Hill MN. Expanding the role of nurses to improve hypertension care and control globally. Annals of Global Health. 2016;82:243–53.
Trigg SA, Abreu D, Foronda BB, Foley FC, Gibson AL. Comparison of systolic blood pressure measurements by auscultation and visual manometer needle jump. Int J Exerc Sci. 2019;12:214–20.
Stergiou GS, Alpert BS, Mieke S, Wang J, O’Brien E. Validation protocols for blood pressure measuring devices in the 21st century. J Clin Hypertens (Greenwich). 2018;20:1096–9.
Stergiou GS, Dolan E, Kollias A, Poulter NR, Shennan A, Staessen JA, et al. Blood pressure measurement in special populations and circumstances. J Clin Hypertens (Greenwich). 2018;20:1122–7.
Palatini P, Benetti E, Fania C, Malipiero G, Saladini F. Rectangular cuffs may overestimate blood pressure in individuals with large conical arms. J Hypertens. 2012;30:530–6.
Arnold A, McNaughton A. Accuracy of non-invasive blood pressure measurements in obese patients. Br J Nurs. 2018;27:35–40.
Padwal R, Majumdar S. Comparability of two commonly used automated office blood pressure devices in the severely obese. Blood Press Monit. 2016;21:313–5.
Sekip A, Nevzat I, Nur K, Erkan A. Validation of the Omron M6 (HEM-7001-E) upper-arm blood pressure measuring device according to the International Protocol in adults and obese adults. Blood Press Monit. 2007;12:219–25.
Funding
The study was supported by the Brazilian Ministry of Science and Technology (CNPq National Research Council) and the Coordination for the Improvement of Higher Education Personnel (CAPES).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Albuquerque, N.S., Padwal, R. & Araujo, T.L. Brazilian health professionals’ perceptions and knowledge about automated blood pressure monitors. J Hum Hypertens 36, 681–688 (2022). https://doi.org/10.1038/s41371-021-00556-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-021-00556-x