Abstract
Birth weight significantly determines newborns immediate and future health. Globally, the incidence of both low birth weight (LBW) and macrosomia have increased dramatically including sub-Saharan African (SSA) countries. However, there is limited study on the magnitude and associated factors of birth weight in SSA. Thus, thus study investigated factors associated factors of birth weight in SSA using multilevel multinomial logistic regression analysis. The latest demographic and health survey (DHS) data of 36 sub-Saharan African (SSA) countries was used for this study. A total of a weighted sample of 207,548 live births for whom birth weight data were available were used. Multilevel multinomial logistic regression model was fitted to identify factors associated with birth weight. Variables with p-value < 0.2 in the bivariable analysis were considered for the multivariable analysis. In the multivariable multilevel multinomial logistic regression analysis, the adjusted Relative Risk Ratio (aRRR) with the 95% confidence interval (CI) was reported to declare the statistical significance and strength of association. The prevalence of LBW and macrosomia in SSA were 10.44% (95% CI 10.31%, 10.57%) and 8.33% (95% CI 8.21%, 8.45%), respectively. Maternal education level, household wealth status, age, and the number of pregnancies were among the individual-level variables associated with both LBW and macrosomia in the final multilevel multinomial logistic regression analysis. The community-level factors that had a significant association with both macrosomia and LBW were the place of residence and the sub-Saharan African region. The study found a significant association between LBW and distance to the health facility, while macrosomia had a significant association with parity, marital status, and desired pregnancy. In SSA, macrosomia and LBW were found to be major public health issues. Maternal education, household wealth status, age, place of residence, number of pregnancies, distance to the health facility, and parity were found to be significant factors of LBW and macrosomia in this study. Reducing the double burden (low birth weight and macrosomia) and its related short- and long-term effects, therefore, calls for improving mothers' socioeconomic status and expanding access to and availability of health care.
Similar content being viewed by others
Introduction
The birth weight of a baby is a critical indicator of their health in the short and long term1,2. An estimated 38% of all under-five deaths globally were reported to have occurred in Sub-Saharan Africa (SSA)3. Macrosomia affects 3–15% of pregnancies worldwide, with high-income countries having the highest percentage (5–20%)4,5. An estimated 20 million (14.6%) newborns worldwide suffer from low birth weight6.
According to a global consensus, a low birth weight (LBW) is defined as a baby's weight of less than 2500 g at birth and macrosomia if the birth weight greater than 4000 g, ideally measured in the first hour of life7. Given that they are more susceptible to dying than heavier ones, it is one of the main causes of neonatal, infant, and childhood mortality and morbidity7,8. In sub-Saharan Africa, the incidence of low birth weight has risen from 4.4 million in 2000 to 5 million in 20159.
Both macrosomia and low birth weight are strongly linked with early childhood mortality and future risks of chronic morbidities10,11,12. Long-term health consequences like impaired motor function, poor cognitive development, and an increased risk of chronic illnesses like diabetes, cancer, and cardiovascular diseases are all closely associated with them13,14,15. In addition to neonatal and infant mortality, low birth weight has a substantial impact on physical and developmental health issues in subsequent childhood and adulthood16,17. It causes stunted growth in children and a higher prevalence of chronic illnesses in adults, including cancer, diabetes mellitus, hypertension, and cardiovascular disease18,19.
Moreover, it has long-term effects like impaired cognitive function and poor academic achievement20,21,22. Low birth weight is generally used as a summary indicator of multilayered public health issues like poor utilisation of pregnancy-related health services, illness, and malnutrition in mothers.
Previous studies have found that advanced maternal age23,24,25, multiple pregnancies26,27, multiparity28,29, obstetric complications30,31, underlying maternal chronic conditions (i.e. hypertensive disorder of pregnancy, gestational diabetes)32,33, infections (such as malaria, HIV)34,35, maternal nutritional status36,37 and substance use38 were found significant determinants of birth weight. The highest prevalence of LBW and macrosomia can demonstrate poor maternal health status, maternal malnutrition (undernutrition and overnutrition), inappropriate pregnancy care, and deprived socio-economic status of mothers39,40,41.
According to previous studies, macrosomia was linked to chronic conditions like diabetes, heart disease, and obesity42,43. Research has shown that LBW, preterm, early neonatal death, and infant and under-five mortality are all associated with compromised maternal reproductive health44,45. Similarly, poor maternal health like obesity, underlying medical conditions (e.g. Diabetic mellitus, hypertension, cardiovascular disease), and substance use like smoking will also lead to increased risk of macrosomia42,46.
Hence, both macrosomia and LBW have long-term effects that place a significant financial strain on Sub-Saharan Africa (SSA) unless public health initiatives are made to address the major risk factors associated with them. Consequently, in order to develop efficient preventive measures to lower the incidence of LBW and macrosomia, underlying factors should be identified. In order avoid information loss and obtain a reliable estimate, we therefore used the multilevel multinomial logistic regression model. The present study employed a methodology that utilised the pooled DHS data of 36 sub-Saharan African countries, resulting in a substantial sample size. This could potentially enhance the study's external validity and power. A comprehensive view of SSA can be obtained by utilising a multilevel approach that takes the neighbourhood effect into account. Furthermore, birth weight has been categorised as a binary outcome in earlier research by being assigned the labels LBW/normal. But as you can see, there is a loss of information because macrosomia is a problem that might not be similar to normal birth weight, so treating macrosomia and normal birth weight as normal is not statistically appropriate.
Methods
Data source and sampling procedure
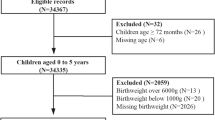
This study was a community based cross-sectional study based on the Demographic and Health Survey (DHS) data of 36 sub-Saharan African countries. To obtain the samples, the DHS consistently employed a multi-stage sampling technique for each country. The primary sampling unit and secondary sampling unit were Enumeration Areas (EAs) and households, respectively. This study made use of the Kids Record dataset (KR file). This survey's details, such as its design, questionnaires, and sampling methods, have been publicly released47. Table 1 presents the weighted sample size for each country (Table 1).
Measurement of variables
The study's outcome variable was birth weight, which was classified as low, normal, and macrosomia. We included live births for whom birth weights were recorded. Maternal education status, household wealth status, age, media exposure, sex of the head of the household, women's autonomy in making health care decisions, marital status, wanted child, child's sex, number of pregnancies, parity, distance to health facility, duration of birth interval, number of ANC visits, sub-Saharan African region and residence were the independent variables considered in the study (Table 2).
Data management and analysis
All the analysis was based on the weighted data. Data management and analysis were done using STATA-17 software. The outcome variable (birth weight) has three categories; LBW, normal and macrosomia.
A multilevel multinomial logistic regression model was fitted to examine the association between individual and community-level variables with macrosomia and LBW, using normal birth weight groups as a reference category. Compared to the standard multinomial logistic regression model, the multilevel multinomial logistic regression analysis has advantages. It reduces parameter overestimation and obtain more accurate estimates of the model parameters because the DHS survey is hierarchical. To estimate the variation between clusters, we used clusters/EAs as a random variable. Furthermore, multilevel modelling can estimate cluster-level effects, also known as random effects, concurrently with measures of associations of community-level variables, such as residence, and region of sub-Saharan Africa. Additionally, birth weight was treated as a binary outcome in previous studies on factors related to birth weight (LBW vs normal)48,49. While birth weight has a multinomial nature (low birth weight, normal, and macrosomia). Therefore, treating birth weight as binary in nature results in a loss of information and is not informative scientifically and not biologically plausible. Given the above-mentioned rationales, multilevel multinomial modeling was fitted. Considering the nature of outcome variable, we fitted both multilevel binary logistic regression and multilevel multinomial logistic regression models by treating birth weight as binary and multiple categories, respectively. Given the analysis results obtained from the these regressions, we choose multilevel multinomial logistic regression model (Supplementary File 1).
Using a multinomial family and logit link, Generalised Structural Equation Modelling (GSEM) was used to implement the multilevel multinomial logistic regression analysis. For the multilevel multinomial logistic regression analysis, four models were built. To find out how much cluster variation there was in the birth weight categories, the first model was an empty one with no explanatory variables. Individual-level variables were used to adjust the second model, community-level variables were used to adjust the third model, and both individual- and community-level variables were fitted simultaneously to the fourth model. The model with the smallest deviance was selected.
The percentage of the total observed individual variation in low birth weight and macrosomia that can be attributed to cluster variations is measured by the intra-class correlation coefficient (ICC), which measures the degree of heterogeneity of birth weight categories between clusters. ICC= \({\partial }^{2}/({\partial }^{2}+\frac{{\pi }^{2}}{3} \)50, where;
\(\partial \)2 indicates that cluster variance.
In the multilevel model, PCV quantifies the overall variation attributable to both individual- and community-level factors in contrast to the null model.
In the bivariable analysis, variables with p-value < 0.2 were chosen and considered for the multivariable analysis. In the final model, the Adjusted Relative Risk Ratio (aRRR) with a 95% Confidence Interval (CI) was reported to define the significance of the association.
Ethical consideration
In the case of this study, we have been granted an authorized letter from the measure DHS program for the use the data. DHS is publicly available de-identified data; ethical approval is not needed.
Results
A total of 207,548 live births with birth weight measurements were included in this study. Of them, 121,192 (58.39%) were from rural areas. More than one-fourth (26.29%) of the mothers had no formal education. About 15.59% and 18.21% of the mothers belonged to the poorest and poorest household quintiles, respectively. The majority (66.04%) of the mothers claimed that perceived distance to the health facility was a big problem. Regarding the number of ANC visits, about 100,616 (48.48%) had 4 ANC visits and above (Table 3).
The prevalence of LBW and macrosomia in sub-Saharan Africa were 10.44% (95% CI 10.31%, 10.57%) and 8.33% (95% CI 8.21%, 8.45%), respectively. The prevalence has varied by country, with LBW prevalence ranging from 6.30% in Rwanda to 16.21% in Comoros and macrosomia prevalence ranging from 1.73% in Chad to 26.68% in Burkina Faso.
Multilevel multinomial regression analysis results
The ICC indicated that a clustering effect existed, which should be addressed with advanced statistical models such as multilevel modelling to obtain an unbiased standard error and draw meaningful conclusions. The null model's ICC value was 11%, meaning that 89% of the variation in birth weight was attributable to individual variability and that only 11% was caused by cluster variability. Additionally, the final model's PCV value of 0.97 indicated that it explained approximately 97% of the variation in birth weight. Then four models were fitted and compared using LLR and deviance as they were nested. The final model (a model with individual and community-level characteristics) was the best-fitted model for the data since it had the lowest deviance value (Table 4).
To identify factors associated with birth weight i.e. low birth weight and macrosomia, a multilevel multinomial logistic regression analysis was fitted. Considering the nature of the DHS data, both individual and community-level variables were considered as independent variables in the model.
Maternal educational status, household wealth status, parity, women's health care decision-making autonomy, sex of household head, marital status, media exposure, maternal age, occupational status, distance to the health facility, sub-Saharan African region, residence, and number of pregnancies had p-value < 0.2 in the bivariable multilevel multinomial regression analysis and considered for the multivariable multilevel multinomial logistic regression analysis. In the multivariable analysis; maternal educational status, household wealth status, maternal age, parity, number of pregnancies, distance to the health facility, residence, and sub-Saharan African region were significantly associated with low birth weight. Mothers who attained primary education, secondary education, and higher had 10% [RRR = 0.90, 95% CI 0.86, 0.93], 21% [aRRR = 0.79, 0.75, 0.83], and 31% [aRRR = 0.69, 95% CI 0.63, 0.76] lower risk of delivering a low birth weight baby compared to mothers who had no formal education, respectively. The risk of having a low birth weight baby decreases with the higher wealth index; poorer [aRRR = 0.94, 95% CI 0.89, 0.98], middle [aRRR = 0.89, 95% CI 0.85, 0.94], richer [aRRR = 0.85, 95% CI 0.81, 0.89] and richest [aRRR = 0.76, 95% CI 0.71, 0.80] had significant reductions. The risks of having low birth weight baby among respondents aged 25–34 and 35–49 years were decreased by 19% [aRRR = 0.81, 95%CI 0.77, 0.84] and 15% [aRRR = 0.85, 95% CI 0.81, 0.90] compared to mothers aged 15–24 years, respectively. Being multiparous was significantly associated with a decreased risk of delivering a low birth weight baby than primiparous mothers. Regarding the number of pregnancies, mothers who had multiple pregnancies were 8.03 times [aRRR = 8.03, 95% CI 7.64, 8.44] a higher risk of having a low birth weight baby than mothers who had single pregnancy. Being a rural resident increased the risk of delivering a low birth weight baby by 1.14 times [aRRR = 1.14, 95% CI 1.09, 1.18] than their counterparts. The risk of giving a low birth weight baby among women who perceived distance to a health facility as a big problem was 1.06 times [aRRR = 1.06, 95% CI 1.03, 1.10] higher compared to those who perceived it as not a big problem. Compared with the East African region, respondents living in Southern Africa [aRRR = 1.14, 95% CI 1.06, 1.22], and West African regions [aRRR = 1.06, 95% CI 1.01, 1.17] were more likely to have children with low birth weight (Table 5).
In the final multilevel multinomial logistic regression analysis; maternal educational status, household wealth status, maternal age, parity, number of pregnancies, marital status, wanted pregnancy, residence, and sub-Saharan African region were significantly associated with macrosomia. Maternal level of education has a significant association with macrosomia; mothers who attained primary education, secondary education, and higher education were 1.25 [aRRR = 1.25, 95% CI 1.20, 1.31], 1.11 times [aRRR = 1.11, 95% CI 1.06, 1.17] and 1.15 times [aRRR = 1.15, 95% CI 1.04, 1.26] times higher risk of having a macrosomic baby than those who didn't attain formal education, respectively. Mothers in the poorer household wealth [aRRR = 1.06, 95% CI 1.01, 1.12] and richest household wealth status [aRRR = 1.14, 95% CI 1.07, 1.21] had an increased risk of delivering a macrosomic baby compared to those in the poorest households. The risk of having a macrosomic baby among mothers aged 35–49 years was decreased by 7% [aRRR = 0.93, 95% CI 0.87, 0.98] than those aged 15–24 years. Babies born to married and divorced/widowed/separated mothers had 1.10 times [aRRR = 1.10, 95% CI 1.02, 1.19] and 1.33 times [aRRR = 1.33, 95% CI 1.23, 1.45] higher risk of macrosomia compared to unmarried women, respectively. Regarding parity and number of pregnancies, the risk of having a macrosomic baby increased as parity increased, and mothers with multiple pregnancies had a lower risk of giving a macrosomic baby [aRRR = 0.47, 95% CI 0.41, 0.54] compared to the singletons. Being rural decreased the risk of macrosomia by 14% [aRRR = 0.86, 95% CI 0.83, 0.97] compared to urban. Compared to the East African region, mothers living in southern Africa and west African regions had a lower risk of delivering a macrosomic baby while those in the Central African region had a higher risk of macrosomia (Table 5).
Discussion
In this study, we investigated into the birth weight-related factors in sub-Saharan Africa, specifically low birth weight and macrosomia. Birth weight was significantly correlated with the following factors: maternal education, household wealth status, maternal age, parity, number of pregnancies, residence, wanted birth, and sub-Saharan Africa region.
A significant association was found between low birth weight and macrosomia and the mother's place of residence. Mothers living in a rural area had a higher risk of delivering low birth weight babies in contrast they were at lower risk of giving a macrosomic baby. This was consistent with studies reported in Developing countries51, Bangladesh52, India53, and the United States of America54. This might be because reproductive health care services in SSA are highly skewed in urban areas, and therefore rural pregnant mothers have poor access to these health care services, health information related to pregnancy, and nutritional awareness55,56. In addition, rural resident pregnant mothers are more susceptible to psychosocial stress, which in turn increases the release of cortisol, and catecholamine, which is linked with low birth weight57,58. The risk of giving low birth weight babies was lower among educated mothers than those who didn't have formal education while the risk of macrosomia was higher among educated than those who didn't have formal education. This is consistent with findings reported in Malawi28, Brazil59, and Eastern Nepal60.
Similarly, the risk of having a low birth weight baby was decreased, and the risk of having a macrosomic baby was increased as the household wealth status increased. It was supported by evidence reported in China61,62, and Ethiopia63. This could be due to pregnant mothers who are less educated are commonly have poor socio-economic status, which in turn results in poor maternal diet which is responsible for low birth weight64,65. In contrast, those who are educated are aware of maternal nutrition like diversified food which is a feature of good household wealth, this might cause excessive pregnancy weight gain and is responsible for increased fetal size62. The lower level of education has also been linked with corresponding limited access to maternal health care66. We speculated that educated women are more likely to adhere to health messages either because of the cognitive priming that education affords. Another important predictor of low birth weight and macrosomia was multiple pregnancies. It was consistent with study findings in Korea67. This could be because multiple pregnancies are identified as high-risk pregnancies, closely linked with a higher risk of maternal and fetal morbidity and mortality68.
Studies showed that multiple pregnancies are at increased risk of preterm birth, congenital anomalies, and twin-twin transfusion syndrome1. Additionally, multiparity was found to be associated with a lower risk of low birth weight and a higher risk of macrosomia. This was in line with many previous researches69,70,71, the possible reason is that multiparous mothers have experience in improving pregnancy outcomes and adhering to pregnancy care. Moreover, advanced maternal age was significantly associated with a lower risk of low birth weight and macrosomia. This was supported by previous studies25,72, it could be due to the increased risk of chronic medical conditions like hypertension, and diabetes as well as nutritional depletion could be responsible for the increased risk of low birth weight and macrosomia73.
Another significant predictor was pregnancy wantedness, which was consistent with studies reported in Ecuador74 and Colombia75. This could be because mothers with wanted pregnancies have more adhered to maternal health care services like antenatal care and nutritional supplementations76. A woman who perceives distance to a health facility as a big problem has a higher risk of delivering a low birth weight baby. It was consistent with study findings in China77, Thailand78, and India79. This could be due to the reason that the healthcare access problem is the main factor for adverse birth outcomes like low birth weight, it highlights that there is a need to make maternal healthcare services available and accessible to the community80. This study has both strengths and limitations. The present study employed a methodology that utilised the pooled DHS data of 36 sub-Saharan African countries, resulting in a substantial sample size. This could potentially enhance the study's external validity and power. A comprehensive view of SSA can be obtained by utilising a multilevel approach that takes the neighbourhood effect into account. Furthermore, birth weight has been categorised as a binary outcome in earlier research by being assigned the labels LBW/normal. But as you can see, there is a loss of information because macrosomia is a problem that might not be similar to normal birth weight, so treating macrosomia and normal birth weight as normal is not statistically appropriate. Despite the above strengths, the DHS data is cross-sectional, and as such causal relationships cannot be made. Because the retrospective data on their prior history was gathered, it is therefore vulnerable to recall bias. Furthermore, as we conducted a secondary data analysis important variable like maternal medical conditions were not available.
Conclusion
In this study, low birth weight and macrosomia were major public health problems in SSA. We identified several factors associated with low birth weight and macrosomia. Higher level of education, improved wealth, multiparity, multiple pregnancies, perceived distance to a health facility as a big problem, and being a rural resident was significantly associated with low birth weight. Similarly, a higher level of education, improved wealth, multiparity, multiple pregnancies, advanced maternal age, wanted pregnancy, maternal age, and being a rural resident were significant predictors of macrosomia. Therefore, MNCH programs in SSA should target high risk groups the prevention of low birth weight and macrosomia.
Data availability
The datasets generated and/or analysed during the current study are available in the https://dhsprogram.com/data/dataset_admin/login_main.cfm.
Abbreviations
- aRRR:
-
Adjusted relative risk ratio
- DHS:
-
Demographic health survey
- CI:
-
Confidence interval
- EAs:
-
Enumeration areas
- ICC:
-
Intra-cluster correlation coefficient
- LLR:
-
Log likelihood ratio
- SSA:
-
Sub-Saharan Africa
References
Almond, D., Chay, K. Y. & Lee, D. S. The costs of low birth weight. Q. J. Econ. 120(3), 1031–1083 (2005).
Paneth, N. S. The problem of low birth weight. Future Child. 5, 19–34 (1995).
Owili, P. O. et al. Cooking fuel and risk of under-five mortality in 23 Sub-Saharan African countries: A population-based study. Int. J. Environ. Health Res. 27(3), 191–204 (2017).
Koyanagi, A. et al. Macrosomia in 23 developing countries: an analysis of a multicountry, facility-based, cross-sectional survey. Lancet 381(9865), 476–483 (2013).
Henriksen, T. The macrosomic fetus: A challenge in current obstetrics. Acta Obstetr. Gynecol. Scand. 87(2), 134–145 (2008).
World Health Organization. UNICEF-WHO Low Birthweight Estimates: Levels and Trends 2000–2015 (World Health Organization, 2019).
Hughes, M. M., Black, R. E. & Katz, J. 2500-g low birth weight cutoff: History and implications for future research and policy. Matern. Child Health J. 21(2), 283–289 (2017).
Lewit, E. M. et al. The direct cost of low birth weight. Future Child. 5, 35–56 (1995).
McAllister, D. A. et al. Global, regional, and national estimates of pneumonia morbidity and mortality in children younger than 5 years between 2000 and 2015: A systematic analysis. Lancet Glob. Health 7(1), e47–e57 (2019).
Ogawa, K. et al. Association between birth weight and risk of pregnancy-induced hypertension and gestational diabetes in Japanese women: JPHC-NEXT study. J. Epidemiol. 32, JE20200302 (2021).
Lambiris, M. J. et al. Birth weight and adult earnings: A systematic review and meta-analysis. J. Dev. Origins Health Dis. 13, 1–8 (2021).
Bunyoli, A. B. Factors Associated with Fetal Macrosomia at Kenyatta National Hospital (University of Nairobi, 2017).
Hack, M., Klein, N. K. & Taylor, H. G. Long-term developmental outcomes of low birth weight infants. Future Child. 5, 176–196 (1995).
Kwinta, P. et al. Assessment of long-term renal complications in extremely low birth weight children. Pediatr. Nephrol. 26(7), 1095–1103 (2011).
Júnior, E. A. et al. Macrosomia. Best Pract. Res. Clin. Obstet. Gynaecol. 38, 83–96 (2017).
Shiono, P. H. & Behrman, R. E. Low birth weight: Analysis and recommendations. Future Child. 5, 4–18 (1995).
Conley, D. & Bennett, N. G. Birth weight and income: Interactions across generations. J. Health Soc. Behav. 42, 450–465 (2001).
Negrato, C. A. & Gomes, M. B. Low birth weight: Causes and consequences. Diabetol. Metab. Syndr. 5(1), 1–8 (2013).
Luo, Z. et al. Tracing the origins of “fetal origins” of adult diseases: Programming by oxidative stress?. Med. Hypoth. 66(1), 38–44 (2006).
McCormick, M. C., Gortmaker, S. L. & Sobol, A. M. Very low birth weight children: Behavior problems and school difficulty in a national sample. J. Pediatr. 117(5), 687–693 (1990).
Karande, S. & Kulkarni, M. Poor school performance. Indian J. Pediatr. 72(11), 961–967 (2005).
Weindrich, D. et al. Late sequelae of low birthweight: Mediators of poor school performance at 11 years. Dev. Med. Child Neurol. 45(7), 463–469 (2003).
Lee, K.-S. et al. Maternal age and incidence of low birth weight at term: A population study. Am. J. Obstet. Gynecol. 158(1), 84–89 (1988).
Aras, R. Y. Is maternal age risk factor for low birth weight?. Arch. Med. Health Sci. 1(1), 33 (2013).
Khoshnood, B., Wall, S. & Lee, K.-S. Risk of low birth weight associated with advanced maternal age among four ethnic groups in the United States. Matern. Child Health J. 9(1), 3–9 (2005).
Moise, J. et al. The outcome of twin pregnancies after IVF. Hum. Reprod. (Oxford, England) 13(6), 1702–1705 (1998).
Wang, Y. A. et al. Preterm birth and low birth weight after assisted reproductive technology-related pregnancy in Australia between 1996 and 2000. Fertil. Steril. 83(6), 1650–1658 (2005).
Muula, A., Siziya, S. & Rudatsikira, E. Parity and maternal education are associated with low birth weight in Malawi. Afr. Health Sci. 11(1), 65–71 (2011).
Shah, P. S. Parity and low birth weight and preterm birth: A systematic review and meta-analyses. Acta Obstet. Gynecol. Scand. 89(7), 862–875 (2010).
Khan, N. & Jamal, M. Maternal risk factors associated with low birth weight. J. Coll. Phys. Surg. Pak. JCPSP 13(1), 25–28 (2003).
Ng, S.-K. et al. Risk factors and obstetric complications of large for gestational age births with adjustments for community effects: Results from a new cohort study. BMC Public Health 10(1), 1–10 (2010).
Rizvi, S. et al. Maternal risk factors associated with low birth weight in Karachi: A case-control study. EMHJ-East. Mediterr. Health J. 13(6), 1343–1352 (2007).
Desta, S. A., Damte, A. & Hailu, T. Maternal factors associated with low birth weight in public hospitals of Mekelle city, Ethiopia: A case-control study. Ital. J. Pediatr. 46(1), 1–9 (2020).
Leviton, A. et al. Maternal infection, fetal inflammatory response, and brain damage in very low birth weight infants. Pediatr. Res. 46(5), 566–566 (1999).
Cottrell, G. et al. Submicroscopic Plasmodium falciparum infections are associated with maternal anemia, premature births, and low birth weight. Clin. Infect. Dis. 60(10), 1481–1488 (2015).
Miele, M. J. et al. Maternal nutrition status associated with pregnancy-related adverse outcomes. Nutrients 13(7), 2398 (2021).
Dharmalingam, A., Navaneetham, K. & Krishnakumar, C. Nutritional status of mothers and low birth weight in India. Matern. Child Health J. 14(2), 290–298 (2010).
Kelly, R. H. et al. Psychiatric and substance use disorders as risk factors for low birth weight and preterm delivery. Obstetr. Gynecol. 100(2), 297–304 (2002).
Savona-Ventura, C. & Savona-Ventura, S. The inheritance of obesity. Best Pract. Res. Clin. Obstet. Gynaecol. 29(3), 300–308 (2015).
Phillips, D. Birth weight and adulthood disease and the controversies. Fetal Matern. Med. Rev. 17(3), 205–227 (2006).
Nwi-ue, L. Predictors of Poor Pregnancy Outcomes Among Pregnant Women in Island Maternity, Nigeria (Walden University, 2019).
Ornoy, A. Prenatal origin of obesity and their complications: Gestational diabetes, maternal overweight and the paradoxical effects of fetal growth restriction and macrosomia. Reprod. Toxicol. 32(2), 205–212 (2011).
Santangeli, L., Sattar, N. & Huda, S. S. Impact of maternal obesity on perinatal and childhood outcomes. Best Pract. Res. Clin. Obstet. Gynaecol. 29(3), 438–448 (2015).
Neel, N. R. & Alvarez, J. O. Maternal risk factor for low birth weight and intrauterine growth retardation in a Guatemalan population. Bull. Pan Am. Health Org. (PAHO) 25(2), 1991 (1991).
Bereczkei, T., Hofer, A. & Ivan, Z. Low birth weight, maternal birth-spacing decisions, and future reproduction. Hum. Nat. 11(2), 183–205 (2000).
Kunz, L. H. & King, J. C. Impact of maternal nutrition and metabolism on health of the offspring. Semin. Fetal Neonatal Med. 12, 71–77 (2007).
Rutstein, S. O. & Rojas, G. Guide to DHS statistics Vol. 38 (Macro, 2006).
Tessema, Z. T. et al. Prevalence of low birth weight and its associated factor at birth in Sub-Saharan Africa: A generalized linear mixed model. PLoS One 16(3), e0248417 (2021).
Aboye, W. et al. Prevalence and associated factors of low birth weight in Axum town, Tigray, North Ethiopia. BMC Res. Notes 11(1), 1–6 (2018).
Rodriguez, G. & Elo, I. Intra-class correlation in random-effects models for binary data. Stata J. 3(1), 32–46 (2003).
Mahumud, R. A., Sultana, M. & Sarker, A. R. Distribution and determinants of low birth weight in developing countries. J. Prev. Med. Public Health 50(1), 18 (2017).
Khan, J. R. et al. Analysis of low birth weight and its co-variants in Bangladesh based on a sub-sample from nationally representative survey. BMC Pediatr. 18(1), 1–9 (2018).
Kader, M. & Perera, N. K. P. Socio-economic and nutritional determinants of low birth weight in India. N. Am. J. Med. Sci. 6(7), 302 (2014).
Parker, J. D., Schoendorf, K. C. & Kiely, J. L. Associations between measures of socioeconomic status and low birth weight, small for gestational age, and premature delivery in the United States. Ann. Epidemiol. 4(4), 271–278 (1994).
Ntoimo, L. F. C. et al. Why rural women do not use primary health centres for pregnancy care: Evidence from a qualitative study in Nigeria. BMC Pregnancy Childbirth 19(1), 1–13 (2019).
Chakraborty, N. et al. Determinants of the use of maternal health services in rural Bangladesh. Health Promot. Int. 18(4), 327–337 (2003).
Loomans, E. M. et al. Psychosocial stress during pregnancy is related to adverse birth outcomes: Results from a large multi-ethnic community-based birth cohort. Eur. J. Public Health 23(3), 485–491 (2013).
Rondó, P. H. et al. Maternal psychological stress and distress as predictors of low birth weight, prematurity and intrauterine growth retardation. Eur. J. Clin. Nutr. 57(2), 266–272 (2003).
de Souza Buriol, V. C. et al. Temporal evolution of the risk factors associated with low birth weight rates in Brazilian capitals (1996–2011). Popul. Health Met. 14(1), 1–10 (2016).
Bhaskar, R. K. et al. A case control study on risk factors associated with low birth weight babies in Eastern Nepal. Int. J. Pediatr. 2015, 1–7 (2015).
Pei, L. et al. Changes in socioeconomic inequality of low birth weight and Macrosomia in Shaanxi Province of Northwest China, 2010–2013: A cross-sectional study. Medicine 95(5), e2471 (2016).
Shen, L. et al. Prevalence of low birth weight and macrosomia estimates based on heaping adjustment method in China. Sci. Rep. 11(1), 1–9 (2021).
Gizaw, B. & Gebremedhin, S. Factors associated with low birthweight in North Shewa zone, Central Ethiopia: Case-control study. Ital. J. Pediatr. 44(1), 1–9 (2018).
Chomitz, V. R., Cheung, L. W. & Lieberman, E. The role of lifestyle in preventing low birth weight. Future Child. 1, 121–138 (1995).
Kramer, M. S. et al. Socio-economic disparities in pregnancy outcome: Why do the poor fare so poorly?. Paediatr. Perinatal Epidemiol. 14(3), 194–210 (2000).
Zere, E. et al. Inequities in utilization of maternal health interventions in Namibia: Implications for progress towards MDG 5 targets. Int. J. Equity Health 9(1), 1–11 (2010).
Kim, H.-E. et al. Trends in birth weight and the incidence of low birth weight and advanced maternal age in Korea between 1993 and 2016. J. Korean Med. Sci. https://doi.org/10.3346/jkms.2019.34.e34 (2019).
Bian, Y. et al. Maternal risk factors for low birth weight for term births in a developed region in China: A hospital-based study of 55,633 pregnancies. J. Biomed. Res. 27(1), 14 (2013).
Dougherty, C. R. & Jones, A. D. The determinants of birth weight. Am. J. Obstet. Gynecol. 144(2), 190–200 (1982).
Khan, A., Nasrullah, F. D. & Jaleel, R. Frequency and risk factors of low birth weight in term pregnancy. Pak. J. Med. Sci. 32(1), 138 (2016).
Yadav, D. K. et al. Maternal and obstetric factors associated with low birth weight. J. Nepal Health Res. Council 17(4), 443–450 (2019).
Goisis, A. et al. Advanced maternal age and the risk of low birth weight and preterm delivery: A within-family analysis using Finnish population registers. Am. J. Epidemiol. 186(11), 1219–1226 (2017).
Delbaere, I. et al. Pregnancy outcome in primiparae of advanced maternal age. Eur. J. Obstet. Gynecol. Reprod. Biol. 135(1), 41–46 (2007).
Eggleston, E., Tsui, A. O. & Kotelchuck, M. Unintended pregnancy and low birthweight in Ecuador. Am. J. Public Health 91(5), 808 (2001).
Pinzón-Rondón, Á. M. et al. Low birth weight and prenatal care in Colombia: A cross-sectional study. BMC Pregnancy Childbirth 15(1), 1–7 (2015).
Chapman, R. R. Endangering safe motherhood in Mozambique: Prenatal care as pregnancy risk. Soc. Sci. Med. 57(2), 355–374 (2003).
Wang, J. et al. Risk factors for low birth weight and preterm birth: A population-based case-control study in Wuhan, China. J. Huazhong Univ. Sci. Technol. [Med. Sci.] 37(2), 286–292 (2017).
Chumnijarakij, T. and N. Dusitsin, Maternal risk factors for low birth weight newborns in Thailand (1988).
Zaveri, A. et al. Maternal determinants of low birth weight among Indian children: Evidence from the National Family Health Survey-4, 2015–16. PLoS One 15(12), e0244562 (2020).
Aday, L. A. & Andersen, R. A framework for the study of access to medical care. Health Serv. Res. 9(3), 208 (1974).
Acknowledgements
We are grateful to the DHS survey team.
Author information
Authors and Affiliations
Contributions
MMB conceived the study. MMB, GAT, and BLS performed data management. All authors analyzed the data, wrote, revised, and approved the manuscript. All the authors read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bezie, M.M., Tesema, G.A. & Seifu, B.L. Multilevel multinomial regression analysis of factors associated with birth weight in sub-Saharan Africa. Sci Rep 14, 9210 (2024). https://doi.org/10.1038/s41598-024-58517-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-58517-6
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.