Abstract
Thrombocytopenia (platelets <150 × 109/L) is common in the early newborn period. Recent evidence suggests this is due mainly to impaired fetal megakaryocytopoiesis/platelet production. The cause remains unknown. Thrombopoietin (Tpo) is now recognized as the major regulator of platelet production in adults. However, nothing is known about Tpo levels, or the role of Tpo in megakaryocytopoiesis/platelet production, in the fetus/newborn. To answer these questions we: 1) measured plasma Tpo levels by ELISA at birth in healthy term (n = 17) and preterm (gestational age, 24-34 wk) babies (n = 16), and in thrombocytopenic preterm babies(n = 13); and 2) assessed the in vitro Tpo dose response characteristics of circulating megakaryocyte precursor cells (MKp) from all three groups. The median Tpo levels were similar in term babies 145 pg/mL (range 52-237 pg/mL) compared with preterm babies 132 pg/mL (32-318 pg/mL). In the thrombocytopenic preterm babies the median Tpo level of 185(46-264) was not significantly higher than in healthy babies, despite the fact that their median platelet counts were significantly lower-82 × 109/L (range 21-135), compared with the healthy preterm babies 252× 109/L (152-320)- p < 0.0001. Tpo levels in the thrombocytopenic preterm babies were also much lower than levels measured in three thrombocytopenic children (905, 2138, and 2700 pg/mL). MKp from all three groups showed dose-dependent proliferation in response to Tpo(p < 0.01 at 100 ng/mL Tpo). Increases in MKp were greater in healthy and thrombocytopenic preterm babies when compared with term babies: 48.2-, 24.6-, and 9.8-fold, respectively (p < 0.05 for both comparisons). These results strongly suggest that: 1) Tpo is a major regulator of megakaryocytopoiesis/platelet production in the fetus/newborn,2) impaired fetal Tpo production may be a factor in early thrombocytopenia in preterm babies, and 3) recombinant human Tpo is likely to be effective in the treatment of early neonatal thrombocytopenia.
Similar content being viewed by others
Main
Thrombocytopenia (platelets <150 × 109/L) is the commonest hematologic abnormality presenting in the newborn(1–3). Nearly 1 in 4 of all newborns admitted to neonatal intensive care units will develop thrombocytopenia(1), whereas in sick preterm babies the incidence of thrombocytopenia can be as high as 72%(2). Thrombocytopenia occurs by 48 h of life in 75% of affected babies(1, 3). Recent evidence demonstrates that the majority of such babies with early thrombocytopenia have vastly reduced numbers of circulating megakaryocyte progenitor and precursor cells at birth(3). This strongly suggests that impaired fetal megakaryocytopoiesis and platelet production is the principal underlying mechanism responsible for their thrombocytopenia. The cause of this is unknown.
Tpo, the recently characterized specific and principal regulator of megakaryocytopoiesis and platelet production, is present in small amounts in healthy adults but is considerably raised in most thrombocytopenic adults(4, 5). Whether Tpo plays an equally pivotal role in megakaryocytopoiesis and platelet production in the healthy fetus and newborn is yet to be confirmed. Indeed nothing is currently known about Tpo levels in healthy term or preterm babies or if Tpo levels change in response to thrombocytopenia in the fetus and newborn. In addition, although megakaryocyte progenitor cells from healthy preterm babies appear to have increased sensitivity to Tpo compared with healthy term babies(6), it is not known if this sensitivity changes in disease states leading to early neonatal thrombocytopenia.
To answer these questions the experiments in this study were designed to:1) measure Tpo levels at birth in healthy term and preterm babies and in preterm babies who develop early thrombocytopenia (≤48 h of age); and 2) assess the in vitro effect of recombinant human Tpo on megakaryocyte precursors from each group.
METHODS
Patients. The study was performed at the Hammersmith Hospital, London. Cord/peripheral blood was obtained at birth from 17 healthy term babies (GA range 37-41 wk) and 29 preterm babies (GA range 24-34 wk). Samples were collected into 10 U/mL preservative-free heparin (CP Pharmaceuticals Ltd). All the term babies were from normal pregnancies and had uncomplicated neonatal courses. All the preterm babies were admitted to the neonatal intensive care unit. 13/29 (45%) developed thrombocytopenia (platelets < 150 × 109/L) by 48 h of age, whereas the remaining 16/29 maintained normal platelet counts until at least d 5. Clinical characteristics and platelet counts of the 29 preterm babies are shown in Table 1. For comparison peripheral blood for Tpo levels was also obtained from three children (age range 7-14 y) with severe nonimmune thrombocytopenia (platelets <50 × 109/L). This study was approved by the local ethical committee.
Thrombopoietin ELISA. Plasma for Tpo ELISA was obtained from blood samples by centrifugation at 500 × g for 10 min within 1 h of collection. Plasma samples were stored at -20°C until analyzed. Tpo levels were measured using a commercially available ELISA (R & D Systems Quantikine Human Tpo ELISA kit), with a lower limit of detection of 15 pg/mL.
MKp Assay. Remaining cell samples (after removal of plasma) were resuspended in an equal volume of RPMI 1640 medium (GIBCO). MNC were separated by density centrifugation on Lymphoprep (Nycomed) (density 1.077 g/mL) and depleted of adherent cells as previously described(7). These MNC are a plentiful source of normal megakaryocyte lineage precursor cells(7)-see below. MNC were cultured over a recombinant human Tpo (R & D Systems) dose range 0-100 ng/mL in a modification of the serum-dependent liquid culture system previously described(7). Briefly, MNC were suspended at 2 × 105/mL in 10 mL tissue culture tubes (Nunc) in Iscove's modified Dulbecco's medium (GIBCO), supplemented with 20% FCS (Harlan Sera-Lab), 1% BSA (GIBCO), 200 μg/mL iron saturated transferrin (Sigma Chemical Co.), 2 × 10-5 M α-monothioglycerol (Sigma Chemical Co.), 10 μL/mL minimal essential medium nonessential amino acids(100x) (GIBCO), and 10 μL/mL minimal essential medium vitamins solution(100×) (GIBCO). Cultures were incubated at 37°C in a humidified atmosphere of 5% CO2 in air in a tissue culture incubator for 10 d. After this, MKp were identified by alkaline phosphatase anti-alkaline phosphatase using a anti-human CD61 primary antibody (Dako) by the criteria previously described(7). (In brief, this assay measures the total number of megakaryocyte lineage precursor cells-from burst-forming unit-megakaryocyte (BFU-MK) to mononuclear megakaryoblasts, which can be produced in liquid culture from a given sample of MNC.) CD61 labeling of preculture MNC showed that no more than 1% of these cells (i.e.<2000) belonged to the megakaryocyte lineage (data not shown). This is in keeping with previous estimations of circulating megakaryocyte lineage cells at birth(8, 9). Where blood samples yielded sufficient MNC, response characteristics of MKp at 100 ng/mL recombinant human IL-3 (R & D Systems) were assessed in parallel by identical methods.
Statistics. All results are expressed as median (range) unless otherwise stated. Comparisons within groups were carried out using the Wilcoxon matched pairs test, and when comparing results between groups the Kruskal-Wallis and Mann-Whitney tests (with Bonferroni correction) were used as appropriate.
RESULTS
Thrombopoietin levels. Tpo was detected in plasma from all 46 babies (Table 2). Healthy term and preterm babies and thrombocytopenic preterm babies all had Tpo levels marginally higher than the normal adult range(4, 5): term, 145 pg/mL (52-237 pg/mL); preterm, 132 pg/mL (32-318 pg/mL); preterm thrombocytopenic, 185(46-264 pg/mL). However, despite the fact that the thrombocytopenic preterm babies had significantly lower platelet counts at birth, and during the 1st wk of life (Table 1), when compared with the healthy preterm babies, there was no significant difference between the Tpo levels in any of the groups (p = 0.311). Moreover, Tpo levels in the thrombocytopenic preterm babies were much lower than the levels seen in the three thrombocytopenic children assessed (905, 2138, and 2700 pg/mL) and as previously reported in thrombocytopenic adults(4, 5).
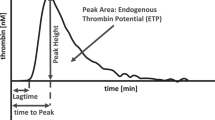
Response of MKp to exogenous Tpo. MKp from all three groups showed dose-dependent proliferation in response to Tpo. In term and healthy preterm babies MKp numbers in culture showed a significant increase over baseline (no Tpo) at both 50 and 100 ng/mL Tpo (p < 0.01 for both comparisons), (Fig 1). MKp from thrombocytopenic preterm babies also showed a similar significant increase (p < 0.01) in response to 100 ng/mL Tpo (Table 2). [As, there are fewer MKp in cord/peripheral blood at birth in preterm babies with early thrombocytopenia(3) (Table 2), we were only able to assess the MKp Tpo response in these babies at 0 and 100 ng/mL Tpo.] MKp from both healthy and thrombocytopenic preterm babies showed a significantly greater response to Tpo than MKp from term babies when the MKp response to Tpo at 100 ng/mL in each group was expressed as a ratio of increase of MKp numbers over cultures containing no Tpo-48.2-, 24.6-, and 9.9-fold, respectively (p < 0.05 for both comparisons,Table 2). MKp from healthy term and preterm babies also showed significant proliferation in response to 100 ng/mL IL-3(Fig. 1); however, this increase was significantly less than that seen with 100 ng/mL Tpo (p < 0.05)(Fig 1).
Dose-response characteristics of MKp to Tpo and IL-3 in healthy term and preterm babies. MKp in both groups show significant proliferation over baseline (no Tpo) at 50 and 100 ng/mL Tpo (p < 0.01 for both comparisons). MKp in both groups also show proliferation over baseline (no Tpo) at 100 ng/mL IL-3; however, this is significantly less pronounced when compared with 100 ng/mL Tpo (p < 0.05).
DISCUSSION
Although c-Mpl ligand or thrombopoietin (Tpo) was only cloned and sequenced in 1994(10–13), characterization of its in vitro and in vivo activity clearly show it to be the major physiologic regulator of megakaryocytopoiesis and platelet production in adults(14). Early onset thrombocytopenia is very common in sick newborns, especially those born preterm. In the main this appears to be the consequence of impaired fetal megakaryocytopoiesis and platelet production occurring at least as early as the most primitive committed megakaryocyte progenitor cell-BFU-MK(3). This suggests that abnormalities of Tpo production and/or Tpo responsiveness of megakaryocyte progenitor and precursor cells in the fetus and newborn may play a role in the development of thrombocytopenia in these groups. However, until now Tpo levels in healthy or thrombocytopenic newborns of all gestations were unknown, as was the responsiveness of megakaryocyte lineage precursor cells to Tpo in thrombocytopenic preterm babies.
This study shows that healthy term and preterm babies and preterm babies with early onset thrombocytopenia (≤48 h) all have detectable levels of Tpo in their plasma at birth-145 pg/mL (52-237 pg/mL), 132 pg/mL (32-318 pg/mL), and 185 (46-264 pg/mL), respectively. These levels are marginally higher than Tpo levels previously reported in healthy adults(4, 5). Preterm babies with early onset thrombocytopenia have slightly higher Tpo levels than those seen in healthy term and preterm babies, but this difference is not statistically significant. MKp from healthy term and preterm babies and from preterm babies with early onset thrombocytopenia all show in vitro dose-dependent proliferation in response to Tpo. This response is greater than that to IL-3. In both healthy and thrombocytopenic preterm babies MKp show significantly greater proliferation in response to Tpo than term babies. These data demonstrate, for the first time, a number of important points in relation to megakaryocytopoiesis and platelet production in the fetus/newborn. First, Tpo is detectable in the human fetus/newborn baby from as early as 24 wk of gestation. In addition, MKp from newborn babies of all viable gestations show a significant proliferative response to Tpo. Because this response is greater than that to IL-3 (the most potent in vitro hemopoietic growth factor stimulator of fetal/neonatal megakaryocyte precursors previously known)(3, 15), this indicates that Tpo is likely to be the major regulator of megakaryocytopoiesis and platelet production in the fetus/newborn, as it is in adults. Second, MKp from both healthy and thrombocytopenic preterm babies show a greater proliferative response to Tpo than MKp from term babies. This is similar to the enhanced response of other “preterm” hemopoietic progenitors to their specific hemopoietic growth factors(16–19). Third, preterm babies appear to have an impaired ability to significantly increase Tpo levels, even in response to thrombocytopenia (as evidenced by the much higher levels of Tpo seen in the thrombocytopenic children we studied and levels reported in thrombocytopenic adults)(4, 5). Inappropriately low Tpo production may have considerable implications for the etiology of early neonatal thrombocytopenia and might be analogous to the impaired erythropoietin production which characterizes “anemia of prematurity”(20). Megakaryocytopoiesis is already impaired in these babies at birth, as evidenced by the reduced numbers of MKp present in cord blood(3) (Table 2), and their lower platelet counts at birth (Table 1). This suggests that there is a dysregulation of fetal megakaryocytopoiesis and that the fetus may not be able to increase platelet production appropriately as a consequence of an inadequate Tpo response. A caveat to this conclusion is that because we measured Tpo levels in the thrombocytopenic babies at birth, and the platelet nadir for most babies was not reached until d 4, it is possible that Tpo levels measured at the platelet nadir would show higher values. (We are currently conducting a study to answer this question.)
In conclusion these studies are the first to begin to define the role of Tpo production/Tpo action in the clinically important setting of neonatal thrombocytopenia. Although more studies will clearly be required, the data from this and from studies in neonatal rats(21) suggest that rh Tpo may have a role in the treatment of neonatal thrombocytopenia, particularly in preterm babies in the early days of life.
Abbreviations
- MKp:
-
megakaryocyte precursor cells
- Tpo:
-
thrombopoietin
- GA:
-
gestational age
- Mnc:
-
mononuclear cell
References
Castle V, Andrew M, Kelton J, Giron D, Johnston M, Carter C 1986 Frequency and mechanism of neonatal thrombocytopenia. J Pediatr 108: 749–755
Metha P, Rohitkumar V, Neumann L, Karpatkin M 1980 Thrombocytopenia in the high risk infant. J Pediatr 97: 791–794
Murray NA, Roberts IAG 1996 Circulating megakaryocytes and their progenitors in early thrombocytopenia in preterm neonates. Pediatr Res 40: 112–119
Tahara T, Usuki K, Sato H, Ohashi H, Morita H, Tsumura H, Matsumoto A, Miyazaki H, Urabe A, Kato T 1996 A sensitive sandwich ELISA for measuring thrombopoietin in human serum: serum thrombopoietin levels in healthy volunteers and in patients with haemopoietic disorders. Br J Haematol 93: 783–788
Emmons RV, Reid DM, Cohen RL, Meng G, Young NS, Dunbar CE, Shulman NR 1996 Human thrombopoietin levels are high when thrombocytopenia is due to megakaryocyte deficiency and low when due to increased platelet destruction. Blood 87: 4068–4071
Nishihira H, Toyoda Y, Miyazaki H, Kigasawa H, Ohsaki E 1996 Growth of macroscopic human megakaryocyte colonies from cord blood with recombinant human thrombopoietin (c-Mpl ligand) and the effects of gestational age on frequency of colonies. Br J Haematol 92: 23–28
Murray NA, Roberts IAG 1995 Circulating megakaryocytes and their progenitors (BFU-MK and CFU-MK) in term and preterm neonates. Br J Haematol 89: 41–46
Warren MK, Guertin M, Rudzinski I, Seidman MM 1993 A new culture and quantitation system for megakaryocyte growth using cord blood CD 34+ cells and the GP IIb/IIIa marker. Exp Hematol 21: 1473–1479
Zucker-Franklin D, Yang JS, Grusky G 1992 Characterization of glycoprotein IIb/IIIa-positive cells in human cord blood: their potential usefulness as megakaryocyte progenitors. Blood 79: 347–355
de Sauvage FJ, Hass PE, Spencer SD, Malloy BE, Gurney AL, Spencer SA, Darbonne WC, Henzel WJ, Wong SC, Kuang W-J, Oles KJ, Hultgren B, Solberg LA Jr, Goeddel DV, Eaton DL 1994 Stimulation of megakaryocytopoiesis and thrombopoiesis by the c-Mpl ligand. Nature 369: 533–538
Lok S, Kaushansky K, Holly RD, Kuijper JL, Lofton-Day CE, Oort PJ, Grant FJ, Heipel MD, Burkhead SK, Kramer JM, Bell LA, Sprecher CA, Blumberg H, Johnson R, Prunkard D, Ching AFT, Mathewes SL, Bailey MC, Forstrom JW, Buddle MM, Osborn SG, Evans SJ, Sheppard PO, Presnell SR, O'Hara PJ, Hagen FS, Roth GJ, Foster DC 1994 Cloning and expression of murine thrombopoietin cDNA and stimulation of platelet production in vivo. Nature 369: 565–568
Kaushansky K, Lok S, Holly RD, Broudy VC, Lin N, Bailey MC, Forstrom JW, Buddle MM, Oort PJ, Hagen FS, Roth GJ, Papayannopoulou T, Foster DC 1994 Promotion of megakaryocyte progenitor expansion and differentiation by the c-Mpl ligand thrombopoietin. Nature 369: 568–571
Wendling F, Maraskovsky E, Debill N, Florindo C, Teepe M, Titeux M, Methia N, Breton-Gorius J, Cosman D, Vainchenker W 1994 c-Mpl ligand is a humoral regulator of megakaryocytopoiesis. Nature 369: 571–574
Eaton DL, de Sauvage FJ 1997 Thrombopoietin: The primary regulator of megakaryocytopoiesis and thrombopoiesis. Exp Hematol 25: 1–7
Teramura M, Katahira J, Hoshino S, Motoji T, Oshimi K 1988 Clonal growth of human megakaryocyte progenitors in serum-free cultures: effect of recombinant human interleukin 3. Exp Hematol 16: 843–848
Traycoff CM, Abboud MR, Laver J, Clapp DW, Hoffman R, Law P, Srour EF 1994 Human umbilical cord blood hematopoietic progenitor cells: are they the same as their adult bone marrow counterparts?. Blood Cells 20: 382–391
Christensen RD, Liechty KW, Koenig JM, Schibler KR, Ohls RK 1991 Administration of erythropoietin to newborn rats results in diminished neutrophil production. Blood 78: 1241–1246
Koenig JM, Christensen RD 1990 Effect of erythropoietin on granulopoiesis: in vitro and in vivo studies in weanling rats. Pediatr Res 27: 583–587
Christensen RD, Koenig JM, Viskochil DH, Rothstein G 1989 Down-modulation of neutrophil production by erythropoietin in human hematopoietic clones. Blood 74: 817–822
Shannon KM 1990 Anaemia of prematurity: progress and prospects. Am J Pediatr Hematol Oncol 12: 16–22
van den Ven C, Fernandez GW, Herbst T, Knoppel A, Cairo MS 1997 Sequential treatment with rmIL-3 or simultaneous treatment with rmIL-3 or rhIL-11 with thrombopoietin (TPO) fails to enhance in vivo neonatal rat thrombocytopoiesis. Exp Hematol 25: 1005–1012
Author information
Authors and Affiliations
Additional information
Supported by grants from Action Research.
Rights and permissions
About this article
Cite this article
Murray, N., Watts, T. & Roberts, A. Endogenous Thrombopoietin Levels and Effect of Recombinant Human Thrombopoietin on Megakaryocyte Precursors in Term and Preterm Babies. Pediatr Res 43, 148–151 (1998). https://doi.org/10.1203/00006450-199801000-00023
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199801000-00023
This article is cited by
-
Developmental changes in hematopoietic stem cell properties
Experimental & Molecular Medicine (2013)
-
Serum thrombopoietin level and thrombocytopenia during the neonatal period in infants with Down's syndrome
Journal of Perinatology (2010)
-
Increasing platelets without transfusion: is it time to introduce novel thrombopoietic agents in neonatal care?
Journal of Perinatology (2010)
-
Thrombocytosis in preterm infants: a possible involvement of thrombopoietin receptor gene expression
Journal of Molecular Medicine (2005)
-
Hematologic Abnormalities in Severe Neonatal Necrotizing Enterocolitis: 25 Years Later
Journal of Perinatology (2003)