Abstract
Background:
In focused radiotherapy for prostate cancer (PC), a full dose of radiation is delivered to the index lesion while reduced dose is delivered to the remaining prostate to reduce morbidity. As PC is commonly multifocal, we investigated whether baseline clinical characteristics or multiparametric magnetic resonance imaging (mpMRI) may be useful to predict the actual pathologic distribution of PC in men with intermediate- or high-risk PC, which may better inform how to deliver focused radiotherapy.
Methods:
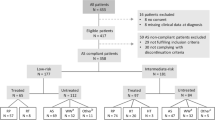
A retrospective single-institutional study was performed on 71 consecutive men with clinically localized, intermediate- or high-risk PC who underwent mpMRI followed by radical prostatectomy (RP) from January 2012 to December 2012. Logistic regression analysis was performed to evaluate preoperative predictors for satellite lesions. Performance characteristics of mpMRI to detect satellite lesions and the extent of prostate disease (one hemi-gland vs both) were also evaluated.
Results:
In all, 50.7% had satellite lesions on mpMRI. On RP specimen analysis, 66.2% had satellite lesions and 55.3% of these satellite lesions had pathologic Gleason score (pGS)⩾3+4. The sensitivity, specificity, positive predictive value, negative predictive value and accuracy for mpMRI detecting a satellite lesion being present in the RP specimen were 59.6%, 66.7%, 77.8%, 45.7% and 62.0%, respectively. The presence of MRI satellite lesions was the only preoperative predictor significantly associated with finding satellite lesions on final pathology (hazard ratio (HR), 2.95, P=0.040). There was agreement in 76.1% of the entire cohort for unilateral vs bilateral disease when incorporating both biopsy and mpMRI information and comparing with the RP specimen.
Conclusions:
In intermediate risk or greater PC, only the presence of mpMRI satellite lesions could predict for pathologic satellite lesions. While combining biopsy and mpMRI information may improve preoperative disease localization, the relatively high incidence of bilateral hemi-gland involvement with pGS ⩾7 satellite lesions makes it challenging to appropriately select men eligible for hemi-gland therapy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Donaldson IA, Alonzi R, Barratt D, Barret E, Berge V, Bott S et al. Focal therapy: patients, interventions, and outcomes—a report from a consensus meeting. Eur Urol 2015; 67: 771–777.
Karavitakis M, Winkler M, Abel P, Livni N, Beckley I, Ahmed HU . Histological characteristics of the index lesion in whole-mount radical prostatectomy specimens: implications for focal therapy. Prostate Cancer Prostatic Dis 2011; 14: 46–52.
Mouraviev V, Mayes JM, Sun L, Madden JF, Moul JW, Polascik TJ . Prostate cancer laterality as a rationale of focal ablative therapy for the treatment of clinically localized prostate cancer. Cancer 2007; 110: 906–910.
Mohler JL, Armstrong AJ, Bahnson RR, D’Amico AV, Davis BJ, Eastham JA et al. Prostate Cancer, Version 1.2016. J Natl Compr Cancer Netw 2016; 14: 19–30.
Zumsteg ZS, Spratt DE, Pei I, Zhang Z, Yamada Y, Kollmeier M et al. A new risk classification system for therapeutic decision making with intermediate-risk prostate cancer patients undergoing dose-escalated external-beam radiation therapy. Eur Urol 2013; 64: 895–902.
Rosenkrantz AB, Kim S, Lim RP, Hindman N, Deng FM, Babb JS et al. Prostate cancer localization using multiparametric MR imaging: comparison of Prostate Imaging Reporting and Data System (PI-RADS) and Likert scales. Radiology 2013; 269: 482–492.
Mouraviev V, Villers A, Bostwick DG, Wheeler TM, Montironi R, Polascik TJ . Understanding the pathological features of focality, grade and tumour volume of early-stage prostate cancer as a foundation for parenchyma-sparing prostate cancer therapies: active surveillance and focal targeted therapy. BJU Int 2011; 108: 1074–1085.
Wise AM, Stamey TA, McNeal JE, Clayton JL . Morphologic and clinical significance of multifocal prostate cancers in radical prostatectomy specimens. Urology 2002; 60: 264–269.
Noguchi M, Stamey TA, McNeal JE, Nolley R . Prognostic factors for multifocal prostate cancer in radical prostatectomy specimens: lack of significance of secondary cancers. J Urol 2003; 170: 459–463.
Ploussard G, Epstein JI, Montironi R, Carroll PR, Wirth M, Grimm MO et al. The contemporary concept of significant versus insignificant prostate cancer. Eur Urol 2011; 60: 291–303.
Le JD, Tan N, Shkolyar E, Lu DY, Kwan L, Marks LS et al. Multifocality and prostate cancer detection by multiparametric magnetic resonance imaging: correlation with whole-mount histopathology. Eur Urol 2015; 67: 569–576.
Gomez-Iturriaga A, Casquero F, Urresola A, Ezquerro A, Lopez JI, Espinosa JM et al. Dose escalation to dominant intraprostatic lesions with MRI-transrectal ultrasound fusion High-Dose-Rate prostate brachytherapy. Prospective phase II trial. Radiother Oncol 2016; 119: 91–96.
von Eyben FE, Kiljunen T, Kangasmaki A, Kairemo K, von Eyben R, Joensuu T . Radiotherapy boost for the dominant intraprostatic cancer lesion—a systematic review and meta-analysis. Clin Genitourin Cancer 2016; 14: 189–197.
Hollmann BG, van Triest B, Ghobadi G, Groenendaal G, de Jong J, van der Poel HG et al. Gross tumor volume and clinical target volume in prostate cancer: how do satellites relate to the index lesion. Radiother Oncol 2015; 115: 96–100.
Priester A, Natarajan S, Khoshnoodi P, Margolis DJ, Raman SS, Reiter RE et al. MRI underestimation of prostate cancer geometry: use of patient-specific molds to correlate images with whole-mount pathology. J Urol 2017; 197: 320–326.
Eiber M, Weirich G, Holzapfel K, Souvatzoglou M, Haller B, Rauscher I et al. Simultaneous 68Ga-PSMA HBED-CC PET/MRI improves the localization of primary prostate cancer. Eur Urol 2016; 70: 829–836.
Ahmed HU . The index lesion and the origin of prostate cancer. N Engl J Med 2009; 361: 1704–1706.
Steenbergen P, Haustermans K, Lerut E, Oyen R, De Wever L, Van den Bergh L et al. Prostate tumor delineation using multiparametric magnetic resonance imaging: Inter-observer variability and pathology validation. Radiother Oncol 2015; 115: 186–190.
Tan N, Margolis DJ, Lu DY, King KG, Huang J, Reiter RE et al. Characteristics of detected and missed prostate cancer foci on 3-T multiparametric MRI using an endorectal coil correlated with whole-mount thin-section histopathology. Am J Roentgenol 2015; 205: W87–W92.
Sfoungaristos S, Perimenis P . Parameters predicting postoperative unilateral disease in patients with unilateral prostate cancer in diagnostic biopsy: a rationale for selecting hemiablative focal therapy candidates. Can Urol Assoc J 2013; 7: E82–E87.
Gallina A, Maccagnano C, Suardi N, Capitanio U, Abdollah F, Raber M et al. Unilateral positive biopsies in low risk prostate cancer patients diagnosed with extended transrectal ultrasound-guided biopsy schemes do not predict unilateral prostate cancer at radical prostatectomy. BJU Int 2012; 110: E64–E68.
Polascik TJ, Mayes JM, Schroeck FR, Sun L, Madden JF, Moul JW et al. Patient selection for hemiablative focal therapy of prostate cancer: variables predictive of tumor unilaterality based upon radical prostatectomy. Cancer 2009; 115: 2104–2110.
Wegelin O, van Melick HH, Hooft L, Bosch JL, Reitsma HB, Barentsz JO et al. Comparing three different techniques for magnetic resonance imaging-targeted prostate biopsies: a systematic review of in-bore versus magnetic resonance imaging-transrectal ultrasound fusion versus cognitive registration. Is there a preferred technique? Eur Urol 2016.
Davis R, Salmasi A, Koprowski C, Kim S, Kwon YS, Faiena I et al. Accuracy of multiparametric magnetic resonance imaging for extracapsular extension of prostate cancer in community practice. Clin Genitourin Cancer 2016; 14: e617–e622.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Dr Margolis reports personal fees from Blue Earth Diagnostics, outside the submitted work. The remaining authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Hegde, J., Margolis, D., Wang, PC. et al. Establishing the distribution of satellite lesions in intermediate- and high-risk prostate cancer: implications for focused radiotherapy. Prostate Cancer Prostatic Dis 20, 241–248 (2017). https://doi.org/10.1038/pcan.2016.75
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2016.75
This article is cited by
-
Impact of preoperative prostate magnetic resonance imaging on the surgical management of high-risk prostate cancer
Prostate Cancer and Prostatic Diseases (2020)