Abstract
In the wake of concerns about the level of antibiotic resistance, governments worldwide are pressing for reduced antibiotic use, hoping thereby to reverse resistance trends. Is success likely? The evidence is mixed, and expectations should be tempered by the growing realization that many resistant bacteria are biologically fit, making them difficult to displace. If resistance is unlikely to be reduced significantly by changing prescription practices, how can clinicians outpace increased resistance, particularly when much of 'big pharma' is abandoning antibiotic development?
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Ibrahim, E. H., Sherman, G., Ward, S., Fraser, V. J. & Kollef, M. H. The influence of inadequate antimicrobial treatment of bloodstream infections on patient outcomes in the ICU setting. Chest 118, 146–155 (2000).
Report of the Joint Committee on the Use of Antimicrobials in Animal Husbandry and Veterinary Medicine. (Her Majesty's Stationery Office, UK, 1969).
House of Lords Select Committee on Science and Technology Seventh Report. Resistance to Antibiotics and other Antimicrobial Agents. (Her Majesty's Stationery Office, UK, 1998).
UK Standing Medical Advisory Committee (SMAC). The Path of Least Resistance. (Department of Health, UK, 1998).
WHO Global Strategy for Containment of Antimicrobial Resistance. (World Health Organization, Geneva, 2001).
Opinion of the Scientific Steering Committee on Antimicrobial Resistance. (European Commission, 2003).
Interagency Task Force on Antimicrobial Resistance. [online], (cited 20 Nov 2003), <http://www.cdc.gov/drugresistance/actionplan/html/index.htm> (2001).
Livermore, D. M. Bacterial resistance: origins, epidemiology, and impact. Clin. Infect. Dis. 36, S11–S23 (2003).
McCaig, L. F., Besser, R. E. & Hughes, J. M. Antimicrobial drug prescription in ambulatory care settings, United States, 1992–2000. Emerg. Infect. Dis. 9, 432–437 (2003).
Livermore, D. M. et al. Trends in fluoroquinolone (ciprofloxacin) resistance among Enterobacteriaceae from bacteraemias in England and Wales, 1990–1999. Emerg. Infect. Dis. 8, 473–478 (2002).
Fenton, K. A. et al. Ciprofloxacin resistance in Neisseria gonorrhoeae in England and Wales in 2002. Lancet 361, 1867–1869 (2003).
Staphylococcus aureus with reduced susceptibility to vancomycin. CDR Weekly 12, 2–3 [online], (cited 20 Nov 2003), <http://www.hpa.org.uk/cdr/PDFfiles/2002/cdr2002.pdf> (17 May 2002).
Alobwede, I. et al. CTX-M extended-spectrum β-lactamase arrives in the UK. J. Antimicrob. Chemother. 51, 470–471 (2003).
Tysall, L. et al. IMP-1 carbapenemase detected in an Acinetobacter clinical isolate from the UK. J. Antimicrob. Chemother. 49, 217–218 (2002).
Seppala, H. et al. The effect of changes in the consumption of macrolide antibiotics on erythromycin resistance in group A streptococci in Finland. Finnish study group for antimicrobial resistance. N. Engl. J. Med. 337, 441–446 (1997).
Austin, D. J., Kristinsson, K. G. & Anderson, R. M. The relationship between the volume of antimicrobial consumption in human communities and the frequency of resistance. Proc. Natl Acad. Sci. USA 96, 1152–1156 (1999).
Aarestrup, F. M. et al. Effect of abolishment of the use of antimicrobial agents for growth promotion on occurrence of antimicrobial resistance in fecal enterococci from food animals in Denmark. Antimicrob. Agents Chemother. 45, 2054–2059 (2001).
Manninen, R., Huovinen, P. & Nissinen, A. Increasing antimicrobial resistance in Streptococcus pneumoniae, Haemophilus influenzae and Moraxella catarrhalis in Finland. J. Antimicrob. Chemother. 40, 387–392 (1997).
Chiew, Y. F., Yeo, S. F., Hall, L. M. & Livermore, D. M. Can susceptibility to an antimicrobial be restored by halting its use? The case of streptomycin versus Enterobacteriaceae. J. Antimicrob. Chemother. 41, 247–251 (1998).
Enne, V. I., Livermore, D. M., Stephens, P. & Hall, L. M. Persistence of sulphonamide resistance in Escherichia coli in the UK despite national prescribing restriction. Lancet 357, 1325–1328 (2001).
Kataja, J. et al. Clonal spread of group A streptococcus with the new type of erythromycin resistance. Finnish study group for antimicrobial resistance. J. Infect. Dis. 177, 786–789 (1998).
Soares, S., Kristinsson, K. G., Musser, J. M. & Tomasz, A. Evidence for the introduction of a multiresistant clone of serotype 6B Streptococcus pneumoniae from Spain to Iceland in the late 1980s. J. Infect. Dis. 168, 158–163 (1993).
Bradley, S. J. et al. The control of hyperendemic glycopeptide-resistant Enterococcus spp. on a haematology unit by changing antibiotic usage. J. Antimicrob. Chemother. 43, 261–266 (1999).
Settle, C. D., Wilcox, M. H., Fawley, W. N., Corrado, O. J. & Hawkey, P. M. Prospective study of the risk of Clostridium difficile diarrhoea in elderly patients following treatment with cefotaxime or piperacillin-tazobactam. Aliment. Pharmacol. Ther. 12, 1217–1223 (1998).
Patterson, J. E., Hardin, T. C., Kelly, C. A., Garcia, R. C. & Jorgensen, J. H. Association of antibiotic utilization measures and control of multiple-drug resistance in Klebsiella pneumoniae. Infect. Control Hosp. Epidemiol. 21, 455–458 (2000).
Rahal, J. J. et al. Class restriction of cephalosporin use to control total cephalosporin resistance in nosocomial Klebsiella. JAMA 280, 1233–1237 (1998).
Burke, J. P. Antibiotic resistance — squeezing the balloon? JAMA 280, 1270–1271 (1998).
Cunha, B. A. Effective antibiotic-resistance control strategies. Lancet 357, 1307–1308 (2001).
Mendelson, G. et al. Staphylococcus aureus carrier state among elderly residents of a long-term care facility. J. Am. Med. Dir. Assoc. 4, 125–127 (2003).
Wiener, J. et al. Multiple antibiotic-resistant Klebsiella and Escherichia coli in nursing homes. JAMA 281, 517–523 (1999).
Corkill, J. E. et al. Molecular epidemiology of endemic ciprofloxacin-resistant Neisseria gonorrhoeae in Liverpool. Int. J. STD AIDS 14, 379–385 (2003).
Bouchard, O. et al. Experience with an 'isolation unit' for patients infected with multi-resistant bacteria. Retrospective study of 49 patients. Presse Med. 28, 1405–1408 (1999).
Muto, C. A. et al. SHEA guideline for preventing nosocomial transmission of multidrug-resistant strains of Staphylococcus aureus and enterococcus. Infect. Control Hosp. Epidemiol. 24, 362–386 (2003).
Kollef, M. H. & Ward, S. The influence of mini-BAL cultures on patient outcomes: implications for the antibiotic management of ventilator-associated pneumonia. Chest 113, 412–420 (1998).
Gillespie, S. H. Antibiotic resistance in the absence of selective pressure. Int. J. Antimicrob. Agents 17, 171–176 (2001).
Nagaev, I., Bjorkman, J., Andersson, D. I. & Hughes, D. Biological cost and compensatory evolution in fusidic acid-resistant Staphylococcus aureus. Mol. Microbiol. 40, 433–439 (2001).
Maisnier-Patin, S., Berg, O. G., Liljas, L. & Andersson, D. I. Compensatory adaptation to the deleterious effect of antibiotic resistance in Salmonella typhimurium. Mol. Microbiol. 46, 355–366 (2002).
Lenski, R. E. The cost of antibiotic resistance — from the perspective of a bacterium. Ciba Found. Symp. 207, 131–140 (1997).
Bouma, J. E. & Lenski, R. E. Evolution of a bacteria/plasmid association. Nature 335, 351–352 (1988).
Rawlings, D. E. Proteic toxin-antitoxin, bacterial plasmid addiction systems and their evolution with special reference to the pas system of pTF-FC2. FEMS Microbiol. Lett. 176, 269–277 (1999).
Galdbart, J. O. et al. TEM-24 extended-spectrum β-lactamase-producing Enterobacter aerogenes: long-term clonal dissemination in French hospitals. Clin. Microbiol. Infect. 6, 316–323 (2000).
Klugman, K. P. The successful clone: the vector of dissemination of resistance in Streptococcus pneumoniae. J. Antimicrob. Chemother. 50, S1–S5 (2002).
Arlet, G. et al. Molecular epidemiology of Klebsiella pneumoniae strains that produce SHV-4 β-lactamase and which were isolated in 14 French hospitals. J. Clin. Microbiol. 32, 2553–2558 (1994).
Johnson, A. P. et al. Dominance of EMRSA-15 and -16 among MRSA causing nosocomial bacteraemia in the UK: analysis of isolates from the European antimicrobial resistance surveillance system (EARSS). J. Antimicrob. Chemother. 48, 143–144 (2001).
Livermore, D. M. The threat from the pink corner. Ann. Med. 35, 226–234 (2003).
Projan, S. Why is big pharma getting out of antibacterial drug discovery? Curr. Opin. Microbiol. 6, 427–430 (2003).
Paterson, D. L. Recommendation for treatment of severe infections caused by Enterobacteriaceae-producing extended-spectrum β-lactamases (ESBLs). Clin. Microbiol. Infect. 6, 460–463 (2000).
Miller, H. I. Dying for FDA reform. Washington Times [online], (cited 20 Nov), <http://washingtontimes.com/commentary/20030615-121434-1657r.htm> (15 Jun 2003).
Sheehan, G. & Chew, N. S. Y. in Fluoroquinolone Antibiotics (eds Ronald, A. R. & Low, D. E.) 1–9 (Birkhauser–Verlag, 2003).
Baquero, F., Bax, R. & Phillips, I. Antibiotic clinical trials revisited. J. Antimicrob. Chemother. 46, 651–652 (2000).
Chopra, I., O'Neill, A. J. & Miller, K. The role of mutators in the emergence of antibiotic-resistant bacteria. Drug Resist. Updat. 6, 137–145 (2003).
Spratt, B. G. Resistance to antibiotics mediated by target alterations. Science 264, 388–393 (1994).
Reacher, M. H. et al. Bacteraemia and antibiotic resistance of its pathogens reported in England and Wales between 1990 and 1998: trend analysis. BMJ 320, 213–216 (2000).
Acknowledgements
The author is grateful to many colleagues past and present whose collaboration has enabled his own work and the development of the views expressed here.
Author information
Authors and Affiliations
Ethics declarations
Competing interests
D. Livermore, and his laboratory staff, are employed by the Health Protection Agency, and so have an interest in it's (and ultimately the state's) continued interest in resistance. He has received sponsorship and research grants from numerous pharmaceutical, biotech and diagnostics companies. Directly, or as attorney, he manages personal and family shareholdings, including in pharmaceutical companies.
Related links
Glossary
- COMMUNITY PRESCRIBING
-
The prescription of antibiotics outside hospitals.
- BACTERAEMIAS
-
A bacterial infection of the bloodstream.
- COMMUNITY-ACQUIRED INFECTIONS
-
An infection that is acquired outside of a hospital.
- EPIDEMIC CLONES
-
Bacterial strains that have spread widely among communities or hospitals.
- FORMULARY CHANGE
-
A change to standard therapies in hospitals.
- EMPIRICAL ANTIBIOTIC TREATMENT
-
A treatment that is based on the pathogens that are likely to be present on the basis of the clinical condition, but before confirmation by culturing bacteria in the laboratory.
- STEP-DOWN THERAPY
-
A switch from powerful to less powerful antibiotics — for example, because the patient is recovering well or a highly sensitive pathogen has been isolated.
- COMPENSATION
-
Adaptations or mutations that enable bacteria to adjust to the fitness burden that is caused by acquired resistance.
Rights and permissions
About this article
Cite this article
Livermore, D. Can better prescribing turn the tide of resistance?. Nat Rev Microbiol 2, 73–78 (2004). https://doi.org/10.1038/nrmicro798
Issue Date:
DOI: https://doi.org/10.1038/nrmicro798
This article is cited by
-
Leidt samen beslissen tot minder antibioticagebruik?
Huisarts en wetenschap (2019)
-
Effectiveness of audit and feedback in addressing over prescribing of antibiotics and injectable medicines in a middle-income country: an RCT
DARU Journal of Pharmaceutical Sciences (2019)
-
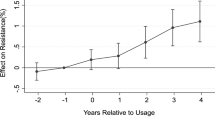
Resistance decay in individuals after antibiotic exposure in primary care: a systematic review and meta-analysis
BMC Medicine (2018)
-
Occurrence and removal of antibiotics and the corresponding resistance genes in wastewater treatment plants: effluents’ influence to downstream water environment
Environmental Science and Pollution Research (2016)
-
Trends and correlation of antibacterial usage and bacterial resistance: time series analysis for antibacterial stewardship in a Chinese teaching hospital (2009–2013)
European Journal of Clinical Microbiology & Infectious Diseases (2015)