Abstract
Several studies link increasing body mass index (BMI) to cognitive decline both as a consequence of obesity per se and as a sequela of obesity-induced type 2 diabetes. Obese individuals are prone to a chronic low-grade inflammation as the metabolically active visceral fat produces proinflammatory cytokines. Animal studies indicate that these cytokines can cross the blood–brain barrier. Such crossover could potentially affect the immune system in the brain by inducing gene expression of proinflammatory genes. The relationship between obesity and neuroinflammation in the human brain is currently unknown. Therefore we aim to examine the relationship between BMI and gene expression of central inflammatory markers in the human frontal cortex. Microarray data of 141 neurologically and psychiatrically healthy individuals were obtained through the BrainCloud database. A simple linear regression analysis was performed with BMI as variable on data on IL10, IL1β, IL6, PTGS2 (COX2) and NOS2 (iNOS). Increasing BMI is associated with a decrease in the mRNA expression of IL10 (P=0.014) and an increase in the expression of NOS2 (iNOS; P=0.040). Expressions of IL10 and NOS2 (iNOS) were negatively correlated (P<0.001). The expression of IL10 was mostly affected by individuals with BMI ⩾40. Multiple linear regression analyses with BMI, age, sex and race as variables were performed in order to identify potential confounders. In conclusion, increasing BMI could affect the IL10-mediated anti-inflammatory defense in the brain and induce iNOS-mediated inflammatory activity.
Similar content being viewed by others

Introduction
The World Health Organization (WHO) estimates that about 1.9 billion adults are currently overweight,1 and obesity represents a massive economic burden on health-care systems worldwide. Much evidence links obesity in midlife to increased risk of dementia in later life.2, 3, 4, 5, 6, 7 However, a recent large-scale retrospective study of 2 million individuals reported that midlife obesity associates with a lower risk of dementia.8 To what extent obesity should be considered an independent risk factor for dementia remains to be settled. A better understanding of the link between obesity and neurodegeneration would be beneficial in the search for new therapeutic targets for common neurodegenerative diseases with an inflammatory component, such as Alzheimer's disease.
Several factors could contribute to an increased risk of developing dementia in the obese. Obese individuals have a higher prevalence of atherosclerosis,9 endothelial dysfunction and cerebral hypoperfusion. These are among the possible mechanisms of obesity-associated cognitive decline.10, 11 Obese individuals are more likely to develop diabetes, insulin resistance and/or metabolic syndrome (MetS). MetS is characterized by elevated plasma glucose levels, hypertension and dyslipidemia.12 It is estimated that 20–25% of all adults suffer from MetS and about 1 in 11 adults have diabetes, of which 90% have type 2 diabetes.13, 14 Type 2 diabetes patients carry a two to five times increased risk of both Alzheimer's disease and vascular dementia15 and MetS is a known risk factor for cognitive decline and overall dementia risk.16 Although the literature is not conclusive on the role of MetS in Alzheimer's disease development,16 the severity of Alzheimer's disease is greater in patients with MetS.17 Likewise, the role of insulin resistance in the brain is currently being investigated.18
Insulin resistance is linked to inflammation.19 Chronic systemic low-grade inflammation is a cardinal feature in obesity as visceral adipose tissue is a highly metabolically active organ that contributes to an increased level of proinflammatory cytokines such as interleukin (IL)-1β and IL6.20, 21, 22 Rodent studies have shown that circulating proinflammatory cytokines can cross the blood–brain barrier.23, 24 The communication between the brain and the periphery occurs via several routes.
Saturable carrier-mediated transport systems have been identified, which transport cytokines IL-1β, IL6 and tumor necrosis factor-α from the blood to the central nervous system (CNS).23, 24 Inflammatory cytokines interact with the circumventricular organs and the brain endothelium24, 25 and circulating proinflammatory cytokines are believed to activate perivascular macrophages and microglia, and also signal through receptors on the cerebral endothelial cells.26, 27 Systemic inflammation in rats triggers microglia and astrocytes to induce IL10, tumor necrosis factor-α, IL-1β and IL6 in cerebral cortex.27 Such activation can affect microglia function within the brain, and microglia activity has been proposed as the link between inflammatory stimuli and altered neuroplasticity.28, 29, 30
Knowledge about the relationship between obesity and inflammation in the human brain is relatively sparse, but obesity has been associated with decreased human white matter integrity.31 In rodents, on the other hand, several studies have shown that obesity and high-fat diets leads to increased gene or protein expression of inflammatory cytokines in the hypothalamus, neocortex and hippocampus.19, 32, 33, 34, 35, 36, 37
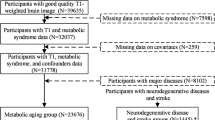
The aim of the present study was to examine the hypothesis that obesity per se will induce an inflammatory response in the human brain. Utilizing microarray data from the BrainCloud database (http://braincloud.jhmi.edu/) of the Lieber Institute for Brain Development, this study analyzes microarray data from frontal cortex in individuals without neurological and psychiatric diseases at the time of death. The potential effect of body mass index (BMI) on the gene expression of selected genes, that is, IL10, IL6, IL1β, NOS2 (iNOS) and PTGS2 (COX2) was investigated by performing simple linear regression analyses treating BMI as the continuous variable including all adult individuals (age⩾18 years) in the cohort (n=141). In order to describe the impact of morbidly obese individuals, additional simple linear regression analyses were performed (n=122) excluding all individuals with a BMI ⩾40 from the analyses.
Several studies indicate that increased inflammatory levels are part of the aging process in the brain.38, 39, 40 In order to investigate possible confounders, we performed multiple linear regression analyses with BMI, age, sex and race as explanatory variables.
Materials and methods
Demographics
The BrainCloud database (http://braincloud.jhmi.edu/) contains a collection of microarray data on post-mortem samples from the human frontal cortex (Brodmann’s area 9 and 46). The samples were collected from individuals aged 0–78 years. The BrainCloud cohort only includes neurologically and psychiatrically healthy individuals. Additional information on sex, race and BMI (defined as: weight (masskg/heightm2) at the time of death was also available. We excluded individuals <18 years of age (n=34), individuals with known diabetes (n=4) and individuals of whom no information on BMI was available (n=17) leaving a total of 141 samples (77 African-Americans, 56 Caucasians, 4 Asian and 4 Hispanic individuals) to be included in the analyses. A detail description of the demographics can be seen in Table 1. All tissue collection was performed with informed consent obtained from the next of kin. All the data were subsequently anonymized in accordance with the rules and regulations of the National Institute of Health (using protocol 90-M-0142).
Genes
Gene expressions analyzed in this study are mRNA expression data. The data were obtained through the use of a complementary DNA microarray chip performed at the NIH/NHGRI microarray core facility using the Illumina Oligoset HEEBO7 chip. A detailed description of tissue preparation and data analysis of BrainCloud is available in Colantuoni et al.41
The genes Il10, 1L1β, IL6, PTGS2 (COX2) and NOS2 (iNOS) were selected for the analyses.
Statistics
Simple linear regression analyses of the expression for each gene was performed treating BMI as a continuous exploratory variable. To investigate the impact of very high BMI, this analysis was also performed on all individuals with a BMI below 40. This was choosen because of the WHO classification of morbidly obesity (BMI ⩾40).42 To identify potential confounders, we performed multiple linear regression analyses including BMI, age, sex and race. This was done for each gene (each probe of each gene if more than one probe was available) treating BMI and age as continuous variables and race and sex as categorical variables. For each data set assumptions of the multiple linear regression model was examined. To this end, normal distribution of the residuals was investigated by inspecting a QQ plot, whereas the linearity and the homoscedasticity of residuals were assessed by inspecting a plot of the residuals against the explanatory variables. Moreover, a squared residual versus leverage plot was made in order to examine the impact of each single observation of the model. No outliers were removed from the analyses. To obtain data fulfilling the assumptions of the multiple regression model, mathematical transformation of some gene expression/BMI data sets was performed, that is, transformation of the gene expression data by an exponential function or the application of a natural logarithm transformation of the variable BMI. In all analyses, a level of 0.05 was considered statistically significant. All analyses were carried out using STATA version 12.1 (College Station, TX, USA).
Results
Careful analysis of assumptions and squared residual versus leverage plots confirmed that the data sets could be appropriately analyzed applying a simple linear regression model and a multiple linear regression model. The relationship between BMI and the mRNA expression of the investigated inflammatory cytokines was not affected by age, sex and race. See Table 2a and b and Figure 1a–e for the simple linear regression analyses, and see Table 3 for the multiple linear regression analyses.
The figure shows simple linear regression models with mRNA expression level of IL10, IL1β, IL6, PTGS2 and NOS2 probe 29594 in relationship to increasing BMI (n=141; a–e). See Table 2a for details. The y axis presents arbitrary mRNA expression values and the x axis presents values of BMI. For NOS2 probe 29594 the y axis presents arbitrary mRNA expression values transformed to an exponential function and the x axis presents values of natural logarithm transformed values of BMI. The figure also shows a simple linear regression model describing the relationship between mRNA expression levels of IL10 in relationship to the mRNA expression levels of NOS2 (iNOS; probe 29594; n=141). (f) For this model the y axis presents arbitrary mRNA expression values transformed to an exponential function and the x axis presents values of mRNA expression of IL10 transformed to an exponential function. (a) The mRNA expression level of IL10 in relationship to increasing BMI (P=0.014). (b) The mRNA expression level of IL1β in relationship to increasing BMI (P=0.485). (c) The mRNA expression level of IL6 in relationship to increasing BMI (P=0.518). (d) The mRNA expression level of PTGS2 (COX2) in relationship to increasing BMI (P=0.468). (e) The mRNA expression level of NOS2 (probe 29594) in relationship to increasing BMI (P=0.040). (f) The mRNA expression level of IL10 in relationship to the mRNA expression of NOS2 (iNOS; probe 29594), coefficient −0.0819 (−0.1190; −0.0447), F(1,139)=19.00, R2=0.120, P<0.001). BMI, body mass index; IL, interleukin.
BMI is associated with an altered mRNA expression of IL10 and iNOS, whereas BMI does not significantly affect the expression level of IL1β, IL6 and PTGS2 (COX2)
Performing a simple linear regression analysis, we found a significantly reduced IL10 expression P=0.014 with increasing BMI (Figure 1a and Table 2a). The expression of NOS2, that is, iNOS (probe 29 594), was significantly upregulated with increasing BMI (P=0.040), whereas no significant effects of BMI were seen on NOS2 probes 30 645 and 37 928 (P=0.136, P=0.801, respectively). The mRNA expression of the proinflammatory cytokines IL1β, IL6 and PTGS2 gene (COX2) was not significantly affected by increasing BMI (P=0.485, P=0.518 and P=0.468, respectively; Figure 1b–e and Table 2a).
In addition, we performed multiple linear regression models including age, race and sex in the analyses confirming the overall association between BMI and IL10 and NOS2 (iNOS) expression (Table 3). There was no statically significant effect of age, race and sex on the mRNA expression of IL10, IL1β, IL6, PTGS2 and NOS2 probe 29 594 and probe 37 928 (Table 3).
To examine the impact of the most markedly obese individuals (BMI ⩾40), we applied a simple linear regression analysis for BMI, omitting these individuals with BMI ⩾40 from the analyses. Looking at the remaining 122 individuals, the expression of NOS2 remains significantly increased with increasing BMI for probes 29 594 and 30 645 (P=0.006 and P=0.006, respectively), whereas probe 37 928 is not statistically significantly affected (P=0.660; Table 2b). On the other hand, the statistical significance of the BMI induced alterations in the expression of IL10 seemed to depend more on the highly obese individuals (P=0.258, simple linear regression analysis with n=122). As seen in Table 2b, the mRNA expression patterns of IL1β, IL6 and PTGS2 (COX2) were not significantly different when looking only at individuals with a BMI below 40.
The mRNA expression of IL10 is inversely correlated with the expression of NOS2
Performing a simple linear regression analysis, we found that there was an inverse relationship between IL10 and NOS2 mRNA expression, assessing NOS2 with probe 29 594 (P<0.001; Figure 1f). We found a similar significant inverse relationship between IL10 and NOS2 expression with NOS2 probe 30 645 and NOS2 probe 37 928 (P=0.017 and P=0.004, respectively).
Increasing age is reflected by a significant downregulation of NOS2 (iNOS), whereas there is no significant effect of aging on PTGS2 (COX2), IL6, IL1β and IL10
In the multiple linear regression analyses, increasing age was associated with a significant downregulation of NOS2 (probe 30645) (P=0.047; Table 3), whereas the expression of NOS2 probe 29 594 and probe 37 928 was not significantly affected by increasing age (P=0.981, P=0.213, respectively). Aging had no significant effect of the expression level of IL10, IL1β, IL6 and PTGS2 (COX2) (P=0.205, P=0.996, P=0.467, P=0.285, respectively) in this cohort.
Discussion
This study demonstrates that in prefrontal cortex of neurologically and psychiatrically healthy humans, a gradual increase in BMI is associated with discrete signs of altered gene expression, that is, reduced mRNA expression of the anti-inflammatory cytokine IL10 and increased mRNA expression of NOS2 (iNOS), albeit with a marked effect of the ~15% (n=19) morbidly obese individuals on the BMI-related changes in IL10 expression. To the best of our knowledge, this study is the first to investigate the relationship between BMI and inflammatory gene expression in human brains without any neurological disease.
Accumulated evidence from animal studies suggests that active inflammation is a neuronal stress factor, which may per se affect higher mental functions such as cognition.26, 30 Increased levels of IL-1β and other inflammatory factors in CNS may damage synaptic function and inhibit long-term potentiation.30 Experimental studies of the endotoxin lipopolysaccharide in rodents support the notion that activation of microglia partly occurs through the toll-like receptor 4 (TLR4), subsequently resulting in the decrease in long-term potentiation.29, 43
Unlike the rodent studies showing a notable increase in IL-1β within brain tissue,33, 34, 36 mRNA expression of the proinflammatory genes IL1β, IL6 and PTGS2 (COX2) appeared to be unrelated to BMI in our study sample. These differences might reflect that this study focused on a neocortical area rather than hypothalamic areas, which are outside the limitations of the blood–brain barrier. One study does describe an association between inflammation in cortical and hippocampal regions and BMI.34 Given the sample size, we cannot be certain that additional inflammatory features could be present selectively in extremely obese individuals, that is, BMI> 40–45, but the present study sample included only 19 morbidly obese individuals limiting our analyses. Supporting an effect of severe obesity, the association between BMI and IL10 expression was only significantly affected when analyses included the 19 individuals with a BMI ⩾40. Expression of NOS2 was still significantly upregulated when excluding the most obese individuals, although expression of probe 37 928 designed to fit an alternative isoform of the NOS2 gene was not statistically affected by BMI. Both the importance of NOS2 isoforms for the activity of this gene and the actual number of individuals displaying this alternative splice variant in our cohort is unknown—but our findings might simply reflect that only few individuals display the alternative isoform detected by probe 37 928. Perhaps more surprisingly, the probe 30 645, which targets a constitutive portion of the NOS2 gene and displays some overlap with the location of the 29 594 probe, appears unaffected by increasing BMI when including all 141 individuals. However, looking at the coefficients for the BMI impact on gene expression in Table 2a it appears that the effect of BMI on NOS2 expression is similar for the two groups and a significant increase with BMI is seen in both cases when excluding the 19 morbidly obese individuals (Table 2b). With the heterogeneity of our sample—in which variations in, eating habits, D-vitamin status and so on are likely to be present—it is noteworthy that the mRNA expressions of both IL10 and NOS2 (iNOS) display an association with increasing BMI in this relatively small cohort. Still, this emphasizes the need for further studies supporting the present microarray findings, through deep RNA sequencing, qPCR and/or protein expression.
Lending support to a potential biological relevance of the altered mRNA expression of NOS2 (iNOS) in the present study, we saw a negative relationship between the increased mRNA expression of NOS2 and the reduced mRNA expression of IL10 (Figure 1f). An attenuated microglial production of nitric oxide as a response of microglia cultured with IL10 has been reported in rats.44 IL10 also downregulates mRNA expression of iNOS in human macrophages.45 Moreover, IL10-deficient mice injected with lipopolysaccharide respond with a higher expression of iNOS than their wild-type counterparts.46 Despite the production of IL10 in adipose tissue22 others have found a reduced IL10 level in the blood of obese individuals.47 On the other hand, Esposito et al.48 found a higher IL10 level in the blood of obese individuals compared with their lean counterparts, but also identified a subgroup of both obese and non-obese individuals suffering from MetS who had significantly lower circulating IL10 levels.
Local production of IL10 in CNS promotes neuronal and glial survival.49 Reduced IL10 levels in the brain would likely increase the sensitivity of the brain toward harmful stimuli. In a murine study, IL10 in the subventricular zone modulates ERK and STAT3 activity. Via these factors, IL10 may play a role in adult neurogenesis,50, 51 hence linking Il10 levels to cognitive abilities. Although the role of obesity as such in cognitive performance is not clear-cut,52 several studies found a negative effect of obesity on cognition, leading to mild cognitive impairment.53, 54 Moreover, there are beneficial effects of weight loss on brain function, such as improved verbal memory, executive functions and global cognition, have been reported in mild cognitive impairment patients.53, 54
In the present study we applied simple linear regression analyses to evaluate the effects of BMI on gene expression. We used multiple linear regression analyses to elucidate whether potential confounders such as age, sex and race affected the results. Similar effects of BMI were seen in both analyses. The resulting R2 values in both the simple linear and the multiple linear regression analyses are, however, while statistically significant, relatively small. This is likely influenced by the nature of the sample in which the number of individuals with very high BMI was somewhat smaller than the large number with average BMI. We believe our findings in conjunction with recent literature point toward a need for further studies of both the impact of BMI and the role of IL10 in the brain during metabolic and inflammatory challenges.
When setting up the study, we included the effect of aging on the investigated genes; however, little impact of age was seen despite the apparent small but significant downregulation of NOS2 on the 37 928 probe. In a previous study using the same data set, others have found a correlation between age and alterations in expression levels of NFKB1, TRAF6, TLR4, IL1R1, BDNF and NGF among others. However, they have not investigated the role of BMI.55 Others have described increased microglia activation in the human brain with increasing age56 and an overall increase in inflammatory activity, which might become detrimental in old age.57 Our cohort is relatively young, and we cannot conclude that neuroinflammation will not be a problem in senescent.
In conclusion, in a population of 141 non-diabetic adult individuals with no known psychiatric or neurological disease, we have found an association between altered gene expression in prefrontal cortex and increasing BMI levels involving a decreased mRNA expression of IL10 and an increased mRNA expression of NOS2 (iNOS) despite indication of an age-related downregulation of this gene in our population. In light of the increasing prevalence of obesity, further research into the long-term effects of obesity on the brain is needed to obtain a better understanding of the underlying mechanisms linking obesity, aging and brain inflammation.
References
WHO 2015 Obesity and overweight. Available at http://www.who.int/mediacentre/factsheets/fs311/en/ (Accessed on July 2016).
Beydoun MA, Beydoun HA, Wang Y . Obesity and central obesity as risk factors for incident dementia and its subtypes: a systematic review and meta-analysis. Obes Rev 2008; 9: 204–218.
Xu WL, Atti AR, Gatz M, Pedersen NL, Johansson B, Fratiglioni L . Midlife overweight and obesity increase late-life dementia risk: a population-based twin study. Neurology 2011; 76: 1568–1574.
Tolppanen AM, Ngandu T, Kareholt I, Laatikainen T, Rusanen M, Soininen H et al. Midlife and late-life body mass index and late-life dementia: results from a prospective population-based cohort. J Alzheimers Dis 2014; 38: 201–209.
Whitmer RA, Gustafson DR, Barrett-Connor E, Haan MN, Gunderson EP, Yaffe K . Central obesity and increased risk of dementia more than three decades later. Neurology 2008; 71: 1057–1064.
Gustafson DR, Backman K, Joas E, Waern M, Ostling S, Guo X et al. 37 years of body mass index and dementia: observations from the prospective population study of women in Gothenburg, Sweden. J Alzheimers Dis 2012; 28: 163–171.
Ng TP, Feng L, Nyunt MS, Feng L, Gao Q, Lim ML et al. Metabolic syndrome and the risk of mild cognitive impairment and progression to dementia: follow-up of the Singapore Longitudinal Ageing Study Cohort. JAMA Neurol 2016; 73: 456–463.
Qizilbash N, Gregson J, Johnson ME, Pearce N, Douglas I, Wing K et al. BMI and risk of dementia in two million people over two decades: a retrospective cohort study. Lancet Diabetes Endocrinol 2015; 3: 431–436.
NIH 2015. Who Is at Risk for Atherosclerosis? Available at https://www.nhlbi.nih.gov/health/health-topics/topics/atherosclerosis/atrisk (Accessed on July 2016).
Garcia-Prieto CF, Hernandez-Nuno F, Rio DD, Ruiz-Hurtado G, Aranguez I, Ruiz-Gayo M et al. High-fat diet induces endothelial dysfunction through a down-regulation of the endothelial AMPK-PI3K-Akt-eNOS pathway. Mol Nutr Food Res 2015; 59: 520–532.
Toda N, Ayajiki K, Okamura T . Obesity-induced cerebral hypoperfusion derived from endothelial dysfunction: one of the risk factors for Alzheimer's disease. Curr Alzheimer Res 2014; 11: 733–744.
Eckel RH, Grundy SM, Zimmet PZ . The metabolic syndrome. Lancet 2005; 365: 1415–1428.
International Diabetes Federation. IDF Diabetes Atlas, 7th edn. International Diabetes Federation: Brussels, Belgium, 2015.
Bak AM, Egefjord L, Gejl M, Steffensen C, Stecher CW, Smidt K et al. Targeting amyloid-beta by glucagon-like peptide -1 (GLP-1) in Alzheimer's disease and diabetes. Exp Opin Ther Targets 2011; 15: 1153–1162.
Biessels GJ, Staekenborg S, Brunner E, Brayne C, Scheltens P . Risk of dementia in diabetes mellitus: a systematic review. Lancet Neurol 2006; 5: 64–74.
Panza F, Frisardi V, Capurso C, Imbimbo BP, Vendemiale G, Santamato A et al. Metabolic syndrome and cognitive impairment: current epidemiology and possible underlying mechanisms. J Alzheimers Dis 2010; 21: 691–724.
Hishikawa N, Fukui Y, Sato K, Kono S, Yamashita T, Ohta Y et al. Cognitive and affective functions in Alzheimer's disease patients with metabolic syndrome. Eur J Neurol 2016; 23: 339–345.
Kim B, Feldman EL . Insulin resistance as a key link for the increased risk of cognitive impairment in the metabolic syndrome. Exp Mol Med 2015; 47: e149.
Chan PC, Hsiao FC, Chang HM, Wabitsch M, Hsieh PS . Importance of adipocyte cyclooxygenase-2 and prostaglandin E2-prostaglandin E receptor 3 signaling in the development of obesity-induced adipose tissue inflammation and insulin resistance. FASEB J 2016; 30: 2282–2297.
Gregor MF, Hotamisligil GS . Inflammatory mechanisms in obesity. Annu Rev Immunol 2011; 29: 415–445.
Bastard JP, Maachi M, Lagathu C, Kim MJ, Caron M, Vidal H et al. Recent advances in the relationship between obesity, inflammation, and insulin resistance. Eur Cytokine Netw 2006; 17: 4–12.
Fjeldborg K, Pedersen SB, Moller HJ, Christiansen T, Bennetzen M, Richelsen B . Human adipose tissue macrophages are enhanced but changed to an anti-inflammatory profile in obesity. J Immunol Res 2014; 2014: 309548.
Banks WA . Blood-brain barrier transport of cytokines: a mechanism for neuropathology. Curr Pharm Desgn 2005; 11: 973–984.
Quan N, Banks WA . Brain-immune communication pathways. Brain Behav Immun 2007; 21: 727–735.
Konsman JP, Parnet P, Dantzer R . Cytokine-induced sickness behaviour: mechanisms and implications. Trends Neurosci 2002; 25: 154–159.
Perry VH, Holmes C . Microglial priming in neurodegenerative disease. Nat Rev Neurol 2014; 10: 217–224.
Wu Z, Zhang J, Nakanishi H . Leptomeningeal cells activate microglia and astrocytes to induce IL-10 production by releasing pro-inflammatory cytokines during systemic inflammation. J Neuroimmunol 2005; 167: 90–98.
Zhang J, Malik A, Choi HB, Ko RW, Dissing-Olesen L, MacVicar BA . Microglial CR3 activation triggers long-term synaptic depression in the hippocampus via NADPH oxidase. Neuron 2014; 82: 195–207.
Hauss-Wegrzyniak B, Lynch MA, Vraniak PD, Wenk GL . Chronic brain inflammation results in cell loss in the entorhinal cortex and impaired LTP in perforant path-granule cell synapses. Exp Neurol 2002; 176: 336–341.
Lyman M, Lloyd DG, Ji X, Vizcaychipi MP, Ma D . Neuroinflammation: the role and consequences. Neurosci Res 2014; 79: 1–12.
Kullmann S, Schweizer F, Veit R, Fritsche A, Preissl H . Compromised white matter integrity in obesity. Obes Rev 2015; 16: 273–281.
de Kloet AD, Pioquinto DJ, Nguyen D, Wang L, Smith JA, Hiller H et al. Obesity induces neuroinflammation mediated by altered expression of the renin-angiotensin system in mouse forebrain nuclei. Physiol Behav 2014; 136: 31–38.
De Souza CT, Araujo EP, Bordin S, Ashimine R, Zollner RL, Boschero AC et al. Consumption of a fat-rich diet activates a proinflammatory response and induces insulin resistance in the hypothalamus. Endocrinology 2005; 146: 4192–4199.
Erion JR, Wosiski-Kuhn M, Dey A, Hao S, Davis CL, Pollock NK et al. Obesity elicits interleukin 1-mediated deficits in hippocampal synaptic plasticity. J Neurosci 2014; 34: 2618–2631.
Kalin S, Heppner FL, Bechmann I, Prinz M, Tschop MH, Yi CX . Hypothalamic innate immune reaction in obesity. Nat Rev Endocrinol 2015; 11: 339–351.
Maric T, Woodside B, Luheshi GN . The effects of dietary saturated fat on basal hypothalamic neuroinflammation in rats. Brain Behav Immunity 2014; 36: 35–45.
Zhang X, Dong F, Ren J, Driscoll MJ, Culver B . High dietary fat induces NADPH oxidase-associated oxidative stress and inflammation in rat cerebral cortex. Exp Neurol 2005; 191: 318–325.
Hopp SC, Royer S, Brothers HM, Kaercher RM, D'Angelo H, Bardou I et al. Age-associated alterations in the time-dependent profile of pro- and anti-inflammatory proteins within the hippocampus in response to acute exposure to interleukin-1beta. J Neuroimmunol 2014; 267: 86–91.
Kohman RA . Aging microglia: relevance to cognition and neural plasticity. Methods Mol Biol 2012; 934: 193–218.
Lynch MA . Age-related neuroinflammatory changes negatively impact on neuronal function. Front Aging Neurosci 2010; 1: 6.
Colantuoni C, Lipska BK, Ye T, Hyde TM, Tao R, Leek JT et al. Temporal dynamics and genetic control of transcription in the human prefrontal cortex. Nature 2011; 478: 519–523.
WHO. BMI Classification. Available at http://apps.who.int/bmi/index.jsp?introPage=intro_3.html (Accessed on July 2016).
Strekalova T, Evans M, Costa-Nunes J, Bachurin S, Yeritsyan N, Couch Y et al. Tlr4 upregulation in the brain accompanies depression- and anxiety-like behaviors induced by a high-cholesterol diet. Brain Behav Immunity 2015; 48: 42–47.
Qian L, Hong JS, Flood PM . Role of microglia in inflammation-mediated degeneration of dopaminergic neurons: neuroprotective effect of interleukin 10. J Neural Trans Suppl 2006; 70: 367–371.
Dugas N, Palacios-Calender M, Dugas B, Riveros-Moreno V, Delfraissy JF, Kolb JP et al. Regulation by endogenous INTERLEUKIN-10 of the expression of nitric oxide synthase induced after ligation of CD23 in human macrophages. Cytokine 1998; 10: 680–689.
Gunnett CA, Berg DJ, Faraci FM, Feuerstein G . Vascular effects of lipopolysaccharide are enhanced in interleukin-10-deficient mice. Stroke 1999; 30: 2191–2195, discussion 2195-2196.
Dorneles GP, Haddad DO, Fagundes VO, Vargas BK, Kloecker A, Romao PR et al. High intensity interval exercise decreases IL-8 and enhances the immunomodulatory cytokine interleukin-10 in lean and overweight-obese individuals. Cytokine 2016; 77: 1–9.
Esposito K, Pontillo A, Giugliano F, Giugliano G, Marfella R, Nicoletti G et al. Association of low interleukin-10 levels with the metabolic syndrome in obese women. J Clin Endocrinol Metab 2003; 88: 1055–1058.
Strle K, Zhou JH, Shen WH, Broussard SR, Johnson RW, Freund GG et al. Interleukin-10 in the brain. Crit Rev Immunol 2001; 21: 427–449.
Pereira L, Font-Nieves M, Van den Haute C, Baekelandt V, Planas AM, Pozas E . IL-10 regulates adult neurogenesis by modulating ERK and STAT3 activity. Front Cell Neurosci 2015; 9: 57.
Wang J, Xie L, Yang C, Ren C, Zhou K, Wang B et al. Activated regulatory T cell regulates neural stem cell proliferation in the subventricular zone of normal and ischemic mouse brain through interleukin 10. Front Cell Neurosci 2015; 9: 361.
Chen B, Jin X, Guo R, Chen Z, Hou X, Gao F et al. Metabolic syndrome and cognitive performance among chinese >/=50 years: a cross-sectional study with 3988 participants. Metab Syndrome Relat Disord 2016; 14: 222–227.
Lara E, Koyanagi A, Olaya B, Lobo A, Miret M, Tyrovolas S et al. Mild cognitive impairment in a Spanish representative sample: prevalence and associated factors. Int J Geriatr Psychiatry 2016; 31: 858–867.
Horie NC, Serrao VT, Simon SS, Gascon MR, Dos Santos AX, Zambone MA et al. Cognitive effects of intentional weight loss in elderly obese individuals with mild cognitive impairment. J Clin Endocrinol Metab 2016; 101: 1104–1112.
Primiani CT, Ryan VH, Rao JS, Cam MC, Ahn K, Modi HR et al. Coordinated gene expression of neuroinflammatory and cell signaling markers in dorsolateral prefrontal cortex during human brain development and aging. PLoS One 2014; 9: e110972.
Schuitemaker A, van der Doef TF, Boellaard R, van der Flier WM, Yaqub M, Windhorst AD et al. Microglial activation in healthy aging. Neurobiol Aging 2012; 33: 1067–1072.
Ritzel RM, Crapser J, Patel AR, Verma R, Grenier JM, Chauhan A et al. Age-associated resident memory CD8 T cells in the central nervous system are primed to potentiate inflammation after ischemic brain injury. J Immunol 2016; 196: 3318–3330.
Acknowledgements
We thank the families who donated tissue to this research. We are grateful for the vision and generosity of the Lieber and Maltz Families who helped make this work possible and thank The AP Møller Foundation for the Advancement of Medical Science and the Lundbeck Foundation, for their contribution to this project. We also thank Amy Deep-Soboslay and Lewellyn B Bigelow for their contributions in the diagnostic review of the subjects included in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Lauridsen, J., Olesen, R., Vendelbo, J. et al. High BMI levels associate with reduced mRNA expression of IL10 and increased mRNA expression of iNOS (NOS2) in human frontal cortex. Transl Psychiatry 7, e1044 (2017). https://doi.org/10.1038/tp.2016.259
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tp.2016.259
This article is cited by
-
High-fat diet feeding triggers a regenerative response in the adult zebrafish brain
Molecular Neurobiology (2023)
-
Daidzein Pro-cognitive Effects Coincided with Changes of Brain Neurotensin1 Receptor and Interleukin-10 Expression Levels in Obese Hamsters
Neurotoxicity Research (2021)
-
Neuroinflammation in frontotemporal dementia
Nature Reviews Neurology (2019)
-
Association between polymorphisms of NOS1, NOS2 and NOS3 genes and suicide behavior: a systematic review and meta-analysis
Metabolic Brain Disease (2019)
-
Intracellular inflammatory and antioxidant pathways in postmortem frontal cortex of subjects with major depression: effect of antidepressants
Journal of Neuroinflammation (2018)