Abstract
Social anxiety disorder (SAD) has been associated with hyper-reactivity in limbic brain regions like the amygdala, both during symptom provocation and emotional face processing tasks. In this functional magnetic resonance imaging study we sought to examine brain regions implicated in emotional face processing, and the connectivity between them, in patients with SAD (n=14) compared with healthy controls (n=12). We furthermore aimed to relate brain reactivity and connectivity to self-reported social anxiety symptom severity. SAD patients exhibited hyper-reactivity in the bilateral fusiform gyrus in response to fearful faces, as well as greater connectivity between the fusiform gyrus and amygdala, and decreased connectivity between the fusiform gyrus and ventromedial prefrontal cortex. Within the SAD group, social anxiety severity correlated positively with amygdala reactivity to emotional faces, amygdala-fusiform connectivity and connectivity between the amygdala and superior temporal sulcus (STS). These findings point to a pivotal role for the fusiform gyrus in SAD neuropathology, and further suggest that altered amygdala-fusiform and amygdala-STS connectivity could underlie previous findings of aberrant socio-emotional information processing in this anxiety disorder.
Similar content being viewed by others
Introduction
Social anxiety disorder (SAD) is one of the most common anxiety disorders, with a lifetime prevalence exceeding 10% in Western societies.1, 2 It is characterized by fear of being negatively evaluated or scrutinized in social situations such as public speaking.3 The excessive concern of negative evaluation leads to marked anxiety in, or avoidance of, social situations. Untreated SAD is considered to be a chronic condition associated with social and workplace impairment, individual suffering and high societal cost.4, 5
Research on the neurobiological underpinnings of SAD has indicated alterations in the fear processing network, including the amygdala, hippocampus, insula, anterior cingulate cortex and medial prefrontal cortex (PFC).6, 7, 8 For example, studies on symptom provocation, implemented as anticipating or delivering a public speech, indicate amygdalar and insular hyperactivity, as well as frontal hypoactivity,9, 10, 11, 12 suggesting dysfunctional emotion regulation and excessive emotional expression during feared situations.
Emotional face stimuli, such as photographs of facial expressions of fear, are also commonly used to activate the fear processing network.8 Facial expressions of fear may have a twofold impact in SAD, both as a threatening stimulus and as a conveyor of the presence of threat in the environment. The most consistent finding from neuroimaging studies of negative emotional face stimuli in SAD is amygdala hyper-reactivity.13, 14 Amygdala reactivity to threatening face stimuli has further been shown to be positively correlated with clinical ratings of SAD severity,15, 16, 17 suggesting a central role for this brain region in the neuropathology of SAD. Altered responses to emotional faces, both in medial prefrontal and insular regions, have also been found in SAD.13, 18 Additionally, reduced structural and functional connectivity between amygdala and the aforementioned medial frontal regions have been demonstrated in SAD patients,19, 20, 21 as well as negative functional connectivity between the insula and dorsal anterior cingulate cortex.22
Also other regions in the face perception network23 have been suggested to be involved in the neuropathology of SAD, with aberrant activity being associated with elevated social anxiety.18, 24, 25, 26 In particular, the fusiform gyrus is a central node in this network implicated in social functions such as face recognition.23, 27 This posterior cortical region has been found to be functionally related to SAD,18, 25 but null findings have also been reported.14, 17 Moreover, in a recent study, Danti and colleagues24 examined functional connectivity between regions in the face perception network in patients with SAD, in comparison with healthy control (HC) participants. The authors used three seed regions involved in face perception, that is, the fusiform gyrus, superior temporal sulcus (STS) and amygdala. The results suggested decreased negative connectivity in SAD patients between the fusiform gyrus and the precuneus, posterior cingulate and sensorimotor cortical areas, as well as aberrant connectivity between the amygdala and frontal, temporal, parietal and sensorimotor areas. However, this study24 examined face processing in general and did not directly target the affective component of the task. Taken together, functional neuroimaging studies imply that SAD is not a disorder of only one central node (e.g., the amygdala). Rather it involves larger parts of the fear network,8 as well as the face perception circuitry.18, 24, 25
Even though negative face stimuli activate both the fear and the face processing networks, and the two probably work together, the functional connectivity between the two networks in SAD is not well understood. One previous brain imaging study of emotional face perception reported altered contribution of fusiform activity to amygdala response, but did so by controlling for fusiform activity while analyzing correlations between social anxiety scores and amygdala response in a non-clinical population.26 Brain connectivity is regularly studied by correlating task-related activity in a seed region with the activity in other regions, a process known as psychophysiological interaction (PPI).28 In this study, we utilized PPI from functional magnetic resonance imaging data to investigate functional brain connectivity within regions implicated in face and fear processing in patients with SAD relative to HC subjects. Specifically, the aim of the study was to investigate neural responses to fearful vs neutral faces and the connectivity between the implicated brain regions. Furthermore, following previous reports of association between social anxiety severity and amygdala reactivity,15, 16, 17 we sought to examine the relationship between SAD symptom severity, brain reactivity and brain connectivity during the face processing task.
Methods
Participants
Fourteen patients who met the DSM-IV3 criteria for SAD (mean±s.d. age 32.4±8.8 years) were included together with 12 HC subjects (age 28.0±8.2 years). Mean age did not differ significantly (t(24)=1.28, P=0.21) between the two groups. The SAD group contained five patients with a high school level education and nine patients with a university level education. The corresponding numbers in the HC group were five and seven, respectively, and level of education did not differ significantly between the groups (χ2(1)=0.097, P=0.76). All participants were right-handed males. Patients were recruited through newspaper advertisements, whereas HC subjects were recruited from public billboards at a nearby hospital. All participants underwent the Structured Clinical Interview for DSM-IV (SCID).29 Patients were initially screened with the Social Phobia Screening Questionnaire30 and interviewed with SCID only if they fulfilled the screening criteria for SAD.30 In addition, the Liebowitz Social Anxiety Scale (LSAS-SR) was administered as a self-report questionnaire 31 to measure severity of social anxiety in the patient group (M=72.1, s.d.=25.7). All patients fulfilled the DSM-IV criteria for SAD as primary diagnosis. Two patients had mild or subthreshold obsessive compulsive disorder and one had comorbid specific phobia.
Exclusion criteria for the patient group were: ongoing psychological treatment; recently started pharmacological treatment; other primary anxiety diagnosis than SAD; current alcohol or drug dependency/abuse and other major psychiatric or organic disorder (e.g., bipolar disorder and schizophrenia) that may have major influence on the results. The SAD patient with comorbid obsessive compulsive disorder was on a steady dose of psychotropic medication (venlafaxine). HC participants did not suffer from any DSM-IV axis I disorder, nor did they have a history of psychiatric disorders.
Ethics statement
The study was approved by the Regional Ethical Committee at the Karolinska Institutet, Stockholm and conducted in accordance with the Helsinki Declaration. All participants provided written informed consent before commencement of the study. During the clinical assessments none of the participants were deemed to have a compromised capacity or ability to consent.
Image acquisition
A Siemens Avanto 1.5 T whole-body MR-scanner equipped with a 12-channel matrix head coil was used to acquire structural and functional scans. Participants entered the scanner head first in supine position with their heads fixated using a vacuum pillow. For structural scans, 176 slices were collected using a 3D magnetization-prepared rapid acquisition gradient echo sequence, repetition time 2300 ms, inversion time 1100 ms, echo time 3.93 ms, slice thickness 1 mm, field of view 256 × 256 mm, matrix 256 × 256. Functional scans were acquired using a T2*-weighted gradient echo planar imaging sequence, 30 interleaved coronal slices, 114 volumes, repetition time 3000 ms, echo time 50 ms, slice thickness 5 mm, gap between slices 0.5 mm, field of view 220 mm, matrix 64 × 64, inplane voxel dimension 3.4 × 3.4 mm.
Stimuli
Participants underwent a standard emotional face paradigm during functional MRI. The paradigm consisted of alternating blocks of neutral and fearful faces interspersed with blocks showing a fixation cross. Photographs of faces from the Ekman and Friesen face collection32 were used as stimuli. Three neutral face blocks and three fearful face blocks were presented. Both blocks consisted of 15 faces presented for 2 s each followed by a fixation cross for 400 ms. In between the face blocks, an 18 s rest block was presented consisting of a white fixation cross on a black background. The task at hand required subjects to identify the sex of the face by pressing buttons with their right index and middle fingers. Mean reaction time and accuracy (percent correct responses) were measured. The total duration of the paradigm was 5 min and 42 s. All participants started with the neutral face block. Participants viewed the stimuli projected on a screen through a mirror on top of the head coil.
Behavior and demographic analyses
Reaction time and accuracy data were analyzed using between-group t-tests with the alpha level set to P<0.05. Demographic and behavior data were analyzed with R 2.14.1 (R Foundation for Statistical Computing, Vienna, Austria).
Functional magnetic resonance imaging analyses
The functional magnetic resonance imaging analyses were carried out using Statistical Parametric Mapping 8 (SPM8; www.fil.ion.ucl.ac.uk/spm) implemented in MATLAB R2012a (The Mathworks, Natick, MA, USA). The first three volumes for each participant were discarded to allow for T1 equilibration effects. Standard image preprocessing steps were performed: (1) slice timing correction to middle slice, (2) motion correction by realignment of functional volumes to mean volume, (3) coregistration of functional and structural scans, (4) normalizing functional scans to Montreal Neurological Institute standard space and reslicing to 3 mm isotropic voxels and (5) smoothing of functional scans with an 8 mm 3D Gaussian kernel (full width, half maximum).
The blood oxygenation level-dependent signal was modeled with the general linear model at each voxel using a canonical hemodynamic response function and a 128 s high-pass filter. Neutral and fearful face-blocks were included as regressors in the model together with six realignment parameters from the motion correction step. Brain reactivity to fearful over neutral faces was used as the contrast of interest, making it possible to selectively study the effect of the fearful expression. First level contrast images (individual level) were subsequently used in second level random effects analyses (group level).
Initially, patients were compared with HC participants on reactivity to fearful over neutral faces. Subsequent PPI analyses were performed with the fusiform gyrus as seed (anatomically defined), motivated by being the site of maximum activation in the reactivity analyses. Additionally, within group regression analysis of brain reactivity was carried out for the SAD group with LSAS-SR total score as predictor. To further examine the association between social anxiety severity and brain connectivity, we conducted a PPI analysis within the SAD group for the fearful over neutral faces contrast with the amygdala as seed region (anatomically defined). LSAS-SR was included as predictor in the second-level, group analysis. The amygdala was chosen as seed region, because reactivity here was associated with SAD severity, in accordance with earlier studies15, 16, 17 and because the amygdala is a core component of the fear network that is proposed to be crucially involved in SAD neuropathology.6, 8
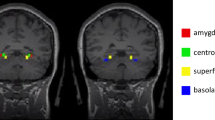
A priori analyses used inclusive masks to examine two predefined anatomical regions highly implicated in face and fear processing: the fusiform gyrus and amygdala.8, 23 The regions were defined anatomically using the Talairach Daemon atlas from Wake Forest University (WFU) Pickatlas.33, 34 The volume of the right fusiform gyrus mask was 510 voxels and the left 516 voxels. The Talairach Daemon atlas was also used to map voxel coordinates to brain regions. All coordinates are reported in Montreal Neurological Institute standard space. To correct for multiple comparisons in the fusiform gyrus mask, the program 3dClustSim from the AFNI library (afni.nimh.nih.gov) was used to calculate a minimum cluster extent from the joint peak threshold P<0.005 and cluster extent threshold P<0.05. This resulted in a minimum cluster size of 11 voxels (297 mm3). Analyses of the fusiform gyrus were thus carried out with peak P-threshold of 0.005 and minimum cluster extent of 11 voxels. The amygdala masks were too small to generate reliable minimum cluster extents, hence we here utilized a family-wise error small volume corrected P-threshold of 0.05. Plots of mean (s.e.m.) extracted β weights in arbitrary units from significant clusters are used to illustrate group differences in connectivity.
Results
Behavioral performance
No significant group differences were found in accuracy or reaction times during the sex-identification task (all P-values>0.3) (see Table 1).
Brain reactivity
Greater reactivity to fearful vs neutral faces was noted in SAD compared with HC bilaterally in the fusiform gyrus (see Table 2 and Figure 1). Exploratory whole brain analyses revealed significantly greater reactivity in SAD compared with HC in the cerebellum, precentral gyrus and superior frontal gyrus (see Table 2).
PPI analyses
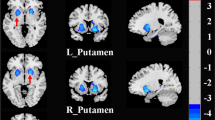
The PPI analyses showed greater connectivity between the fusiform gyrus and right amygdala for the patients compared with the HC group when viewing fearful relative to neutral faces (Table 2 and Figure 2). An exploratory whole brain PPI analysis, further revealed less connectivity (SAD<HC) between the fusiform gyrus and a cluster with its statistical maxium in the ventromedial PFC (vmPFC; see Table 2 and Figure 2).
Changes in fusiform gyrus connectivity in patients with social anxiety disorder (SAD) compared with healthy controls (HC) during processing of fearful over neutral faces. The fusiform showed greater connectivity (SAD>HC) with the amygdala (left, coronal plane at y=−7; illustrative P-threshold of P<0.05 uncorrected) and less connectivity (SAD<HC) with the ventromedial prefrontal cortex (vmPFC; right, sagittal plane at x=−3; illustrative P-threshold of P<0.005). The colorbar indicates t-values. The graphs display extracted measures of connectivity. Error bars represent s.e.m.
Impact of symptom severity
Within group regressions revealed significant positive correlations between LSAS-SR total score and bilateral amygdala reactivity to fearful over neutral faces in the patient group (see Table 3). Subsequent PPI analysis yielded a positive correlation between LSAS-SR score and connectivity between the amygdala and right fusiform gyrus (see Table 3). Exploratory whole brain analyses showed further positive correlations between LSAS-SR score and amygdala connectivity with the cerebellum, precentral gyrus, middle temporal gyrus, middle occipital gyrus, superior temporal gyrus stretching into the STS and supramarginal gyrus (see Table 3).
Discussion
This study examined brain reactivity and functional connectivity in central face and fear processing regions in patients with SAD compared with HC subjects. The patients exhibited heightened reactivity (>HC) to fearful over neutral faces bilaterally in the fusiform gyrus. Furthermore, the patients showed greater fusiform connectivity with right amygdala and less connectivity with the vmPFC compared with the HC group. Social anxiety severity correlated positively with bilateral amygdala reactivity and also with amygdala connectivity with the right fusiform gyrus in SAD patients.
Our finding of increased neural reactivity to emotional faces in the bilateral fusiform gyrus in SAD is interesting in light of previous imaging studies demonstrating involvement of this region in face processing23 and studies showing altered processing of emotional faces in SAD.13, 14 Earlier, studies of functional alterations in the fusiform gyrus to emotional faces have been inconsistent in SAD with reports of hypo-25 and hyper-reactivity,18 as well as null findings.14, 17 In line with our results, a meta-analysis by Etkin and Wager6 showed that SAD was associated with fusiform hyper-reactivity to negative emotional stimuli. In contrast to the study by Gentili et al.25 that showed fusiform hypoactivation in response to both emotional and neutral faces in combination compared with scrambled pictures, we studied the difference in activation between fearful and neutral faces including only the emotional component of face processing. Moreover, the peak voxel of the fusiform clusters in the two studies differ, ours being more posterior and inferior in comparison with Gentili et al.25 These differences may indicate functional segregation of emotional and non-emotional face processing in the fusiform gyrus. Notably, an earlier study18 also found fusiform hyper-reactivity to emotional faces in SAD. We argue, therefore, that processing of emotional face information is associated with fusiform hyper-reactivity in SAD.
Additionally, we found that SAD was associated with greater connectivity between the fusiform gyrus and the amygdala and lesser connectivity between the fusiform gyrus and the vmPFC, during processing of fearful faces. This is consistent with findings of increased bidirectional effective connectivity between amygdala and visual processing areas during the resting state in SAD.35 The vmPFC is involved in regulation of emotions36 and may thus be less activated during processing of fearful faces, indicative of dysfunctional emotion regulation in SAD. Our findings are, however, in contrast to a recent study by Danti et al.,24 who re-analyzed the data from Gentili and colleagues25 to evaluate fusiform connectivity during general face processing. They found increased connectivity to the posterior cingulate cortex and precuneus, but no difference in connectivity to the vmPFC. The difference in results may be due to the focus on fearful face processing in the present study.
Within the SAD group, we also found a positive relationship between social anxiety severity and amygdala reactivity as well as amygdala connectivity, such that more severe social anxiety was associated with stronger amygdala reactivity and stronger amygdala-fusiform connectivity. These findings are in line with previous reports on amygdala hyper-reactivity to emotional faces in anxiety disorders,8, 13 as well as a positive association between amygdala activity and social anxiety symptom severity.15, 16, 17 The amygdala may in turn drive fusiform activity, which would be consistent with cognitive therories of increased attentional bias to negative social stimuli in SAD.37 Interestingly, Prater et al.21 recently showed decreased connectivity between the amygdala and frontal cortex during processing of fearful vs happy faces in SAD. This strengthens the notion of a dysfunctional fear regulatory network and aberrant connectivity between fear and face processing networks in this disorder. Effective treatment may target these regulatory networks.38 Amygdala activity may partly reflect emotion evaluation/awareness, which presumably is more pronounced in individuals with more severe social anxiety. In this study, however, we did not find an effect of group on amygdala reactivity. This may be due to low power, as we did find a significant relationship between social anxiety severity and amygdala reactivity to fearful over neutral faces. A potential bias may also have been introduced by the neutral face comparison, as SAD patients may interpret neutral faces as more threat-provoking than HC.13 Comparison between fearful and happy faces may be a better contrast for this reason.
Furthermore, we found an association between social anxiety severity and connectivity between the amygdala and the STS during processing of fearful over neutral faces in SAD. The STS has been associated with social face processing, such as processing of the intention of others and facial expression of emotions,27, 39 making this region interesting in social cognition. Indeed, abnormal responses to face processing has been found in the STS in SAD.18, 25 It has further been suggested that the interaction between the STS and amygdala may underlie processing of the emotional state of others.27 Our finding of a positive association between symptom severity and amygdala-STS connectivity suggests that the amygdala may be recruited to a larger extent during processing of the emotional state of others and thereby contributing to increased anxiety during social interactions. This enhanced coupling may also contribute to amygdala hyper-reactivity to emotional faces found in SAD.13, 14
Some limitations of the current study deserve mentioning. First, because only males were studied, generalization to women must be done with caution. Also, the number of participants was low for the within-group regression analyses limiting statistical power. However, the magnitudes of the effects were generally large and our results fit well with earlier studies. All study participants were not drug-naïve, meaning that some noise may have been introduced into the data by earlier treatment in the patient group.
In summary, this study demonstrates that SAD is associated with increased reactivity in the fusiform gyrus, greater fusiform-amygdala connectivity and less fusiform-vmPFC connectivity during processing of fearful faces. Furthermore, social anxiety scores correlated with amygdala reactivity, as well as connectivity between amygdala and other regions involved in face and fear processing. Thus, the face perception and fear processing networks, as well as connections between these systems, seem to be affected in SAD, which may help explain earlier findings of aberrant processing of social-affective stimuli in this disorder.
References
Furmark T . Social phobia: overview of community surveys. Acta Psychiatr Scand 2002; 105: 84–93.
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE . Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry 2005; 62: 593–602.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 4th edn, Text Revision. American Psychiatric Publishing, Inc: Washington, DC, USA, 2000.
Acarturk C, Smit F, de Graaf R, van Straten A, Ten Have M, Cuijpers P . Economic costs of social phobia: a population-based study. J Affect Disord 2009; 115: 421–429.
Fehm L, Pelissolo A, Furmark T, Wittchen H-U . Size and burden of social phobia in Europe. Eur Neuropsychopharmacol 2005; 15: 453–462.
Etkin A, Wager TD . Functional neuroimaging of anxiety: a meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. Am J Psychiatry 2007; 164: 1476–1488.
Hattingh CJ, Ipser J, Tromp SA, Syal S, Lochner C, Brooks SJ et al. Functional magnetic resonance imaging during emotion recognition in social anxiety disorder: an activation likelihood meta-analysis. Front Hum Neurosci 2012; 6: 347.
Shin LM, Liberzon I . The neurocircuitry of fear, stress, and anxiety disorders. Neuropsychopharmacology 2010; 35: 169–191.
Furmark T, Tillfors M, Marteinsdottir I, Fischer H, Pissiota A, Långström B et al. Common changes in cerebral blood flow in patients with social phobia treated with citalopram or cognitive-behavioral therapy. Arch Gen Psychiatry 2002; 59: 425–433.
Lorberbaum JP, Kose S, Johnson MR, Arana GW, Sullivan LK, Hamner MB et al. Neural correlates of speech anticipatory anxiety in generalized social phobia. Neuroreport 2004; 15: 2701–2705.
Tillfors M, Furmark T, Marteinsdottir I, Fischer H, Pissiota A, Långström B et al. Cerebral blood flow in subjects with social phobia during stressful speaking tasks: a PET study. Am J Psychiatry 2001; 158: 1220–1226.
Tillfors M, Furmark T, Marteinsdottir I, Fredrikson M . Cerebral blood flow during anticipation of public speaking in social phobia: a PET study. Biol Psychiatry 2002; 52: 1113–1119.
Freitas-Ferrari MC, Hallak JEC, Trzesniak C, Filho AS, Machado-de-Sousa JP, Chagas MHN et al. neuroimaging in social anxiety disorder: a systematic review of the literature. Prog Neuropsychopharmacol Biol Psychiatry 2010; 34: 565–580.
Stein MB, Goldin PR, Sareen J, Zorrilla LTE, Brown GG . Increased amygdala activation to angry and contemptuous faces in generalized social phobia. Arch Gen Psychiatry 2002; 59: 1027–1034.
Evans KC, Wright CI, Wedig MM, Gold AL, Pollack MH, Rauch SL . A functional MRI study of amygdala responses to angry schematic faces in social anxiety disorder. Depress Anxiety 2008; 25: 496–505.
Goldin PR, Manber T, Hakimi S, Canli T, Gross JJ . Neural bases of social anxiety disorder: emotional reactivity and cognitive regulation during social and physical threat. Arch Gen Psychiatry 2009; 66: 170–180.
Phan KL, Fitzgerald DA, Nathan PJ, Tancer ME . Association between amygdala hyperactivity to harsh faces and severity of social anxiety in generalized social phobia. Biol Psychiatry 2006; 59: 424–429.
Straube T, Kolassa I-T, Glauer M, Mentzel H-J, Miltner WHR . Effect of task conditions on brain responses to threatening faces in social phobics: an event-related functional magnetic resonance imaging study. Biol Psychiatry 2004; 56: 921–930.
Miskovic V, Schmidt LA . Social fearfulness in the human brain. Neurosci Biobehav Rev 2012; 36: 459–478.
Phan KL, Orlichenko A, Boyd E, Angstadt M, Coccaro EF, Liberzon I et al. Preliminary evidence of white matter abnormality in the uncinate fasciculus in generalized social anxiety disorder. Biol Psychiatry 2009; 66: 691–694.
Prater KE, Hosanagar A, Klumpp H, Angstadt M, Phan KL . Aberrant amygdala-frontal cortex connectivity during perception of fearful faces and at rest in generalized social anxiety disorder. Depress Anxiety 2012; 3: 234–241.
Klumpp H, Angstadt M, Phan KL . Insula reactivity and connectivity to anterior cingulate cortex when processing threat in generalized social anxiety disorder. Biol Psychol 2012; 89: 273–276.
Haxby JV, Hoffman EA, Gobbini MI . The distributed human neural system for face perception. Trends Cogn Sci 2000; 4: 223–233.
Danti S, Ricciardi E, Gentili C, Gobbini MI, Pietrini P, Guazzelli M . Is social phobia a ‘mis-communication’ disorder? brain functional connectivity during face perception differs between patients with social phobia and healthy control subjects. Front Syst Neurosci 2010; 4: 152.
Gentili C, Gobbini MI, Ricciardi E, Vanello N, Pietrini P, Haxby JV et al. Differential modulation of neural activity throughout the distributed neural system for face perception in patients with social phobia and healthy subjects. Brain Res Bull 2008; 77: 286–292.
Pujol J, Harrison BJ, Ortiz H, Deus J, Soriano-Mas C, López-Solà M et al. Influence of the fusiform gyrus on amygdala response to emotional faces in the non-clinical range of social anxiety. Psychol Med 2009; 39: 1177–1187.
Haxby JV, Hoffman EA, Gobbini MI . Human neural systems for face recognition and social communication. Biol Psychiatry 2002; 51: 59–67.
Friston KJ, Buechel C, Fink GR, Morris J, Rolls E, Dolan RJ . Psychophysiological and modulatory interactions in neuroimaging. Neuroimage 1997; 6: 218–229.
First MB, Spitzer RL, Gibbon M, Williams JBW . Structured Clinical Interview for DSM-IV Axis I Disorders - Non-Patient Edition. Biometrics Research, New York State Psychiatric Institute: New York, NY, USA, 1997.
Furmark T, Tillfors M, Everz P, Marteinsdottir I, Gefvert O, Fredrikson M . Social phobia in the general population: prevalence and sociodemographic profile. Soc Psychiatry Psychiatr Epidemiol 1999; 34: 416–424.
Fresco DM, Coles ME, Heimberg RG, Liebowitz MR, Hami S, Stein MB et al. The Liebowitz social anxiety scale: a comparison of the psychometric properties of self-report and clinician-administered formats. Psychol Med 2001; 31: 1025–1035.
Ekman P, Friesen WV. . Pictures of Facial Affect. Consulting Psychologist Press, Inc: Palo Alto, CA, USA, 1976.
Lancaster JL, Woldorff MG, Parsons LM, Liotti M, Freitas CS, Rainey L et al. Automated Talairach atlas labels for functional brain mapping. Hum Brain Mapp 2000; 10: 120–131.
Maldjian JA, Laurienti PJ, Kraft RA, Burdette JH . An automated method for neuroanatomic and cytoarchitectonic atlas-based interrogation of fMRI data sets. Neuroimage 2003; 19: 1233–1239.
Liao W, Qiu C, Gentili C, Walter M, Pan Z, Ding J et al. Altered effective connectivity network of the amygdala in social anxiety disorder: a resting-state FMRI study. PLoS ONE 2010; 5: e15238.
Hartley CA, Phelps EA . Changing fear: the neurocircuitry of emotion regulation. Neuropsychopharmacology 2010; 35: 136–146.
Schultz LT, Heimberg RG . Attentional focus in social anxiety disorder: potential for interactive processes. Clin Psychol Rev 2008; 28: 1206–1221.
Phan KL, Coccaro EF, Angstadt M, Kreger KJ, Mayberg HS, Liberzon I et al. Corticolimbic brain reactivity to social signals of threat before and after sertraline treatment in generalized social phobia. Biol Psychiatry 2013; 73: 329–336.
Pelphrey KA, Morris JP, McCarthy G . Grasping the intentions of others: the perceived intentionality of an action influences activity in the superior temporal sulcus during social perception. J Cogn Neurosci 2004; 16: 1706–1716.
Acknowledgements
We thank Sara Marklund for help with the data collection. We are also grateful to the study participants, without whom this research would not have been possible. This research has made use of the SMILE medical imaging laboratory at Karolinska University Hospital, Stockholm. Financial support was provided through the Swedish Research Council, the regional agreement on medical training and clinical research between Stockholm County Council and the Karolinska Institutet (ALF) and grants from the National Board of Forensic Medicine in Sweden.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Frick, A., Howner, K., Fischer, H. et al. Altered fusiform connectivity during processing of fearful faces in social anxiety disorder. Transl Psychiatry 3, e312 (2013). https://doi.org/10.1038/tp.2013.85
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tp.2013.85
Keywords
This article is cited by
-
Distinct Effects of Social Stress on Working Memory in Obsessive-Compulsive Disorder
Neuroscience Bulletin (2021)
-
Die Domäne „soziale Prozesse“ im System der Research Domain Criteria: aktueller Stand und Perspektive
Der Nervenarzt (2021)
-
Brain structure correlates of expected social threat and reward
Scientific Reports (2020)
-
Brain structural connectivity and neuroticism in healthy adults
Scientific Reports (2018)
-
Neuroimaging Predictors and Mechanisms of Treatment Response in Social Anxiety Disorder: an Overview of the Amygdala
Current Psychiatry Reports (2018)